Classification
A patient comes into your office for care of a tumor on his skin. What kind is it? What is the best treatment? This complex process of diagnosing and managing skin tumors is not learned easily. As an aid to the establishment of the correct diagnosis, all skin tumors (excluding warts, which are caused by a virus) are classified
2. according to the patient’s age group (
Table 27-2),
4. on the basis of clinical appearance (
Table 27-4).
A complete histologic classification is found at the end of this chapter; only the more common tumors are classified and discussed here. This histologic classification is divided into epidermal tumors, mesodermal tumors, nevus cell tumors, lymphomas, and myeloses. In making a clinical diagnosis of any skin tumor, one should apply a histopathologic label if possible. Whether the label is correct or not depends on the clinical acumen of the physician and whether the tumor, or a part of it, has been examined microscopically.
An age group classification is helpful from a differential diagnostic viewpoint. Viral warts are considered in this classification because of the frequent necessity of differentiating them from other skin tumors.
The clinical appearance of any tumor is a most important diagnostic factor. Some tumors have a characteristic color and growth that is readily distinguishable from any other tumor, but a large number, unfortunately, have clinical characteristics common to several similar tumors or are nonspecific in appearance even to the most trained observer. A further hindrance to making a correct diagnosis is that the same histopathologic lesion may vary in clinical appearance. The following generalizing classification should be helpful, but, if in doubt, the lesion should be examined histologically.
Seborrheic Keratoses
It is a rare elderly patient who does not have any seborrheic keratoses. These are the unattractive “moles” or “warts” that perturb the elderly patient, occasionally become irritated, but are benign (
Fig. 27-1).
Dermatosis papulosa nigra is a form of seborrheic keratosis of African-Americans that occurs on the face, mainly in women. These small, black, multiple tumors can be removed, but there is a possibility of causing keloids or hypopigmentation. Stucco keratoses are numerous white 1- to 3-mm seborrheic keratoses mainly over the feet, ankles, and lower legs. A very large seborrheic keratosis is sometimes referred to as a melanoacanthoma.
Presentation and Characteristics
Description
The size of the seborrheic keratoses varies up to 3 cm for the largest, but the average diameter is 1 cm. The color may be flesh-colored, tan, brown, or coal black. They are usually oval in shape, elevated, and have a greasy, warty sensation to the touch. White, brown, or black pinhead-sized keratotic areas called pseudohorned cysts are commonly seen within this tumor. They have the appearance of being superficial and “stuck on” the skin. Markings on the skin may be accentuated in superficial seborrheic keratoses. Pruritus is common and sudden appearance may occur. Numerous lesions coming on rapidly can be a marker of underlying cancer (sign of Leser-Trélat). They can suddenly appear at the site of inflamed skin (Myerson’s phenomenon) and may dissipate as the inflammation is brought under control.
Distribution
The lesions appear on the face, neck, scalp, back, and upper chest, and less frequently on the arms, legs, and the lower part of the trunk. Mucous membranes, palms, and soles are spared.
Course
Lesions become darker and enlarge slowly. However, sometimes they can enlarge rapidly and this can be accompanied by bleeding and inflammation, which can be very frightening to the patient. Trauma from clothing occasionally results in infection and bleeding, and this prompts the patient to seek
medical care. Any inflammatory dermatitis around these lesions causes them to enlarge temporarily and become more evident, so much so that many patients suddenly note them for the first time. After the inflammation subsides the seborrheic keratosis may dissipate. Malignant degeneration of seborrheic keratoses does not occur.
Cause
Heredity is the biggest factor, along with old age.
Differential Diagnosis
Pigmented nevi: Longer duration, smoother surface, softer to the touch; may not be able to differentiate clinically (see later in this chapter)
Flat warts: In younger patients; acute onset, with rapid development of new lesions, colorless and flat topped without pseudohorned cysts; tiny black
thrombosed capillaries may be seen, usually smaller; may koebnerize (see
Chapter 23)
Malignant melanoma: Less common, usually with rapid growth, indurated; histological examination with biopsy may be necessary (see later)
Treatment
Case Example: A 58-year-old woman requests the removal of a warty, tannish, slightly elevated 2 × 2 cm lesion of the right side of her forehead.
1. The lesion should be examined carefully. The diagnosis usually can be made clinically, but if there is any question, a scissor biopsy (see
Chapter 2) can be performed. It would be ideal if all of these seborrheic keratoses could be examined histologically, but this is not economically feasible or necessary. If in doubt, always send for histologic examination.
2. An adequate form of therapy is curettement, with or without local anesthesia, followed by a light application of trichloroacetic acid, Monsel’s solution, or aluminum
chloride. The resulting fine atrophic scar will hardly be noticeable in several months.
3. Electrosurgery can be used, but this usually requires anesthesia and if the physician is not careful, it may scar.
4. If available, liquid nitrogen freezing therapy works well. It is the therapy of choice of most dermatologists. Do not freeze excessively.
5. Laser therapy has been used recently by some authors.
6. Surgical excision is an unnecessary and more expensive form of removal.
Pedunculated Fibromas (Skin Tags, Acrochordons)
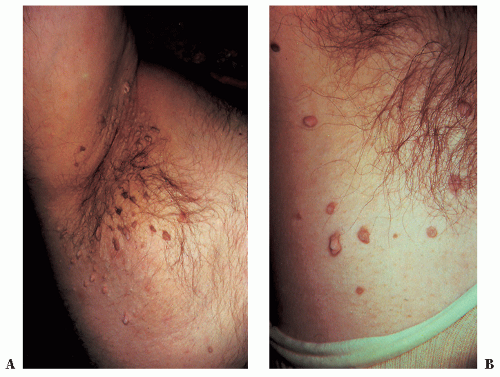
Multiple skin tags are common on the neck and the axillae of middle-aged, usually obese, men and women (
Fig. 27-2). The indications for removal are twofold: cosmetic, as desired and requested by the patient, and to prevent the irritation and the secondary infection of the pedicle that frequently develops from trauma of a collar, necklace, or other article of clothing. These are often inherited and may be part of the metabolic syndrome.
Presentation and Characteristics
Description
Pedunculated pinhead-sized to pea-sized soft tumors of normal skin color or light brown are seen. The base may be inflamed from injury, and the lesion may thrombose and turn black if twisted. This can cause alarm in the patient.
Distribution
The lesions occur on the neck, axillae, submammary or groin, or less frequently on any area.
Course
These fibromas grow very slowly. They may increase in size during pregnancy. Some become infected or thrombosed and drop off.
Differential Diagnosis
Filiform wart: Digitate projections, more horny; also seen on the chin area (see
Chapter 23)
Pedunculated seborrheic keratosis: Larger lesion, darker color, warty, or velvety appearance (see preceding section)
Neurofibromatosis: Lesions seen elsewhere; larger; can be pushed back into the skin; also café-au-lait spots; hereditary; single lesions do not indicate systemic disease (see
Chapters 38 and
40)
Treatment
Case Example: A 42-year-old woman has 20 small pedunculated fibromas on her neck and axillae that she wants removed. This could be done by electrosurgery. Without anesthesia, gently grab the small tumor in a thumb forceps
and stretch the pedicle. Touch this pedicle with the electrosurgery needle and turn on the current for a split second. The tumor separates from the skin, and no bleeding occurs. The site heals in 4 to 7 days.
For very small lesions, a short spark with the electrosurgical needle suffices. Scissor excision with or without local anesthetic is commonly done.
Cysts
The three common types are
An
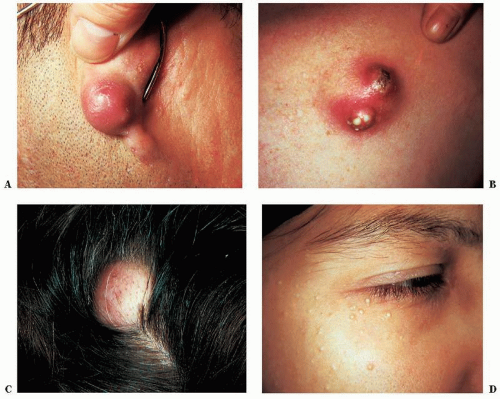
epidermal cyst (
Fig. 27-3A and B) has a wall composed of true epidermis and probably originates from an invagination of the epidermis into the dermis and subsequent detachment from the epidermis, or it can originate spontaneously. The most common locations for epidermal cysts are the face, ears, neck, back, and scalp, where tumors of varying size can be found. A central pore may be seen over the surface. There may be a history of drainage of foul smelling cheesy debris.
Trichilemmal cysts, formerly known as
wens and
pilar or
sebaceous cysts (
Fig. 27-3C), are less common than epidermal cysts, occur mainly on the scalp, usually are multiple, and show an autosomal-dominant inheritance. The sac wall is thick, smooth, and whitish and can be quite easily enucleated.
Milia (
Fig. 27-3D) are very common, white, pinhead-sized, firm lesions that are seen on the face. They are formed by proliferation of epithelial buds following trauma to the skin (dermabrasion for acne scars), following certain dermatoses (pemphigus, epidermolysis bullosa, and acute contact dermatitis), or from no apparent cause. Occurrences with porphyria cutanea tarda, after 5-fluorouracil therapy, in areas of corticosteroid-induced atrophy, after burns, and after radiation therapy are other causes.
They can occur spontaneously at any age including newborns where they may dissipate. Treatment consists of opening the lesion with a No. 11 Bard Parker blade and expression with a comedone extractor. This is done for cosmetic reasons only.
Differential Diagnosis of Epidermal and Trichilemmal Cysts
Lipoma: Difficult to differentiate clinically; more firm, no central pore, lobulated; no cheesy material extrudes on incision; removal is by complete excision or by liposuction; clinically similar to hibernoma
Dermoid cyst: Clinically similar; can also be found internally; usually a solitary skin tumor; histologically, contains hairs, eccrine glands, and sebaceous glands
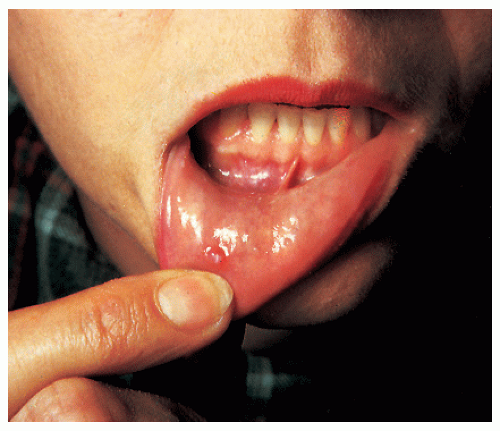
Mucous cysts (
Fig. 27-4): Translucent pea-sized or smaller lesions on the lips, treated by cutting off the top of the lesion and carefully, lightly cauterizing the base with a silver nitrate stick or light electrosurgery; laser therapy can also be used
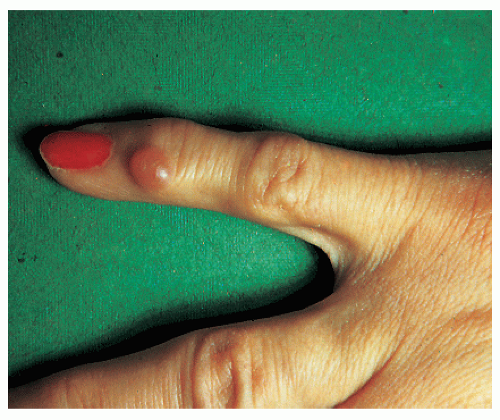
Synovial cysts (myxoid cysts) of the skin (
Fig. 27-5): Globoid, translucent, pea-sized swellings around the joints of fingers and toes that drain a syrupy clear liquid and are most common at the base of the nail on the proximal nail fold
Treatment of Epidermal and Trichilemmal Cysts
Several methods can be used with success. The choice depends on the ability of the operator, the site, and the number of cysts. Cysts can regrow after even the best surgical care because of incomplete removal of the sac.
1. A single 3-cm cyst on the back should be removed by surgical excision and suturing. This can be done in two ways: either by incising the skin and skillfully removing the intact cyst sac with an ellipse excision or by cutting straight into the sac with a small incision, shelling out the evacuated lining by applying strong pressure to the sides of the incision, and suturing the skin. The latter procedure is simpler, requires a smaller incision, and is quite successful.