Technologic Applications in Dermatology
Frank Custer Koranda MD, MBA
The therapeutic options of dermatologists have widely expanded with advances in technology. Most of these technologies can be employed in an office setting. Some of the more common technologic applications include lasers, intense pulsed light (IPL), photodynamic therapy, radiofrequency devices, liposuction, lipotransfer, fat autograft mesenchymal injection (FAMI), Botox injections, tissue fillers, and augmentation.
Lasers
Laser is an acronym for light (L) amplification (A) by the stimulated (S) emissions (E) of radiation (R). The characteristics of laser light are that the light is monochromatic (a single wavelength), collimated (the rays are parallel or nondivergent), and coherent (the rays are in phase so that they can pass over distances without loss of energy).
Carbon Dioxide Laser
When laser light contacts the skin, the light energy is absorbed. The energy causes thermal coagulation or, with greater energy, tissue vaporization. The carbon dioxide (CO2) laser has a wavelength of 1600 nm in the mid-infrared spectrum, which is invisible. The CO2 laser is absorbed by water in the tissue. It is an ablative laser, causing damage to all tissue because the water content is the laser target. When the CO2 laser is used in a focused mode, it can be used as a cutting instrument with a width of 0.2 mm as compared with the 0.25 mm width of a #15 scalpel blade. As the CO2 laser cuts, it vaporizes the tissue. In a defocused mode, the CO2 laser’s effect is that of tissue coagulation, and in this mode it can seal blood vessels 0.5 mm or smaller in diameter. The CO2 laser produces thermal damage that can spread beyond the target tissue.
The depth of penetration of the CO2 laser is controlled by the power output measured in watts and by the time on target. Fluence is the measurement of the energy density to the target and is expressed as joules per square centimeter.
Because the CO2 laser is invisible, it is coupled and coaxially aligned with a low-power laser in the visible spectrum that serves as an aiming device. The helium-neon-aiming laser produces a red light.
The initial CO2 lasers were of a continuous wave output unless deactivated by the foot control. In the early 1990s, pulsed focused CO2 lasers were introduced. The goal of pulsing the laser was to decrease the thermal damage to surrounding nontargeted skin. The initial pulsed CO2 lasers were of 0.1 to 1.0 seconds in duration. To further reduce thermal transfer, ultrapulsed CO2 lasers were developed to deliver high-energy output over a very short duration. The Coherent UltraPulse CO2 laser can deliver 250 to 500 W of power in less than a 1-millisecond pulse.
The ultrapulsed laser reduces tissue damage by timing the pulse duration to approximate the tissues’ thermal relaxation time, that is, the time for a tissue to significantly cool by heat conduction. The principles of selective photothermolysis apply to most lasers: first, there is selective absorption of the laser energy or light by the target tissue; second, with the use of a brief pulse at high enough power, effective energy may be transmitted to the target with limited heat dispersal beyond the target. The CO2 laser is used for a wide variety of treatments and conditions:
Resurfacing of the face for rejuvenation of the skin and reduction of wrinkles
Vaporization of actinic cheilitis
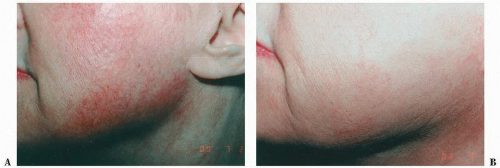
Planning for rhinophyma (Fig. 5-1), angiofibromata of tuberous sclerosis, sebaceous hyperplasia
Removal of common warts and condylomata accuminatum
Removal of keloids and hypertrohic scars (Fig. 5-2)
Incisional surgery requiring more precision and when hemostasis by methods other than electrocoagulation is needed
These examples are a limited list of the applications of the CO2 laser.
The CO2 laser was one of the first lasers to have been widely employed for a variety of cutaneous conditions. Today there are hosts of other lasers with different wavelength outputs and other characteristics such as pulsed modes, pulsed durations, and pulsed repetitions. Each laser has different uses depending on the absorption spectrum of the target tissues. The wavelength of the laser is matched to the absorption peaks of the target tissues.
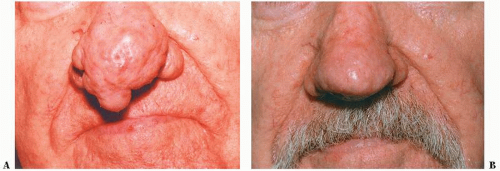 FIGURE 5-1 ▪ Rhinophyma before (A) and after (B) nasal planing with the Coherent CO2 Ultrapulse laser. |
These other lasers have wavelengths in the visible (400 to 700 nm) to near-infrared (700 to 1200 nm) spectra. In general, as the wavelength of the light increases, the depth of penetration into the skin increases and so does the depth at which the energy is absorbed. In addition to identifying the absorption spectrum of the targeted structure, the depth of the structure in the skin also influences the selection of a laser with the appropriate wavelength output. The wavelength must also be different from the absorption peaks of any intervening tissue that could absorb the laser light before it reaches its target tissue.
Pulsed Dye, Nd:YG, Q-switched, and Diode Lasers
The pulsed dye laser, usually with a 585-nm wavelength and a 450-microsecond or 0.45-millisecond pulse, has been used extensively for congenital hemangiomas, particularly port wine stains (Fig. 5-3). Multiple treatments, sometimes more than 20, are required. The necessity for retreatment 5 to 8 years after apparently successful treatment is not unusual. Recurrence may be due to blood vessels at a depth beyond the reach of the 585-nm wavelength laser.
For deeper penetration, a neodymium:yttrium aluminum garnet (Nd:YAG) laser at 1064 nm can be directed toward deeper vasculature while sparing the overlying melanin. This type of laser has also been used for deeper and larger leg vein treatments (Fig. 5-4).
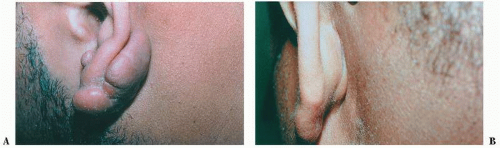 FIGURE 5-2 ▪ Keloid of the ear before (A) and after (B) removal with the Coherent CO2 Ultrapulse laser. |
Q-switched (QS) lasers have a pulse duration of 10 to 20 nanoseconds. QS lasers are most frequently used for tattoo removal by heating and fracturing the ink pigment particles. The fragmented particles are extruded through the epidermis and cleared by the lymphatic system. Usually six or more treatments are required and often all the remnants of the tattoo cannot be removed. Some residual scarring or pigmentary changes in the skin are common. The selection of the proper laser depends on the color of the tattoo. Green pigment is best removed by a red light laser; red pigment, by a green light laser; and yellow pigment is poorly removed by all lasers. The QS Ruby (694 nm) and QS Alexandrite (77 nm) lasers are used for blue and green inks, the QS Nd:YAG (1064 nm) for black ink, and the QS Nd:YAG/2 (532 nm) for red inks. Most professional tattoos require the use of different lasers for effective treatment because of the multicolors. Homemade tattoos with India ink are easier to remove than professional tattoos (Fig. 5-5).
Hair removal lasers are usually in the 694- to 1064-nm wavelengths so that there is sufficient depth of penetration for absorption by the melanin in the hair follicle. The 800-nm diode laser is also effective for hair removal. This laser contains a cooling system to afford additional protection against
injury to the overlying skin. Although the lasers have been touted for permanent removal of hair, more truly this is a process for the progressive reduction of hair. This process requires several treatments and often follow-up treatments in ensuing years. Usually laser treatment is only effective for pigmented hair, since melanin is the target. The most common side effects are hyper- or hypopigmentation. The darker the skin and the higher the fluences applied to the tissue, the more aptly these effects may develop.
injury to the overlying skin. Although the lasers have been touted for permanent removal of hair, more truly this is a process for the progressive reduction of hair. This process requires several treatments and often follow-up treatments in ensuing years. Usually laser treatment is only effective for pigmented hair, since melanin is the target. The most common side effects are hyper- or hypopigmentation. The darker the skin and the higher the fluences applied to the tissue, the more aptly these effects may develop.
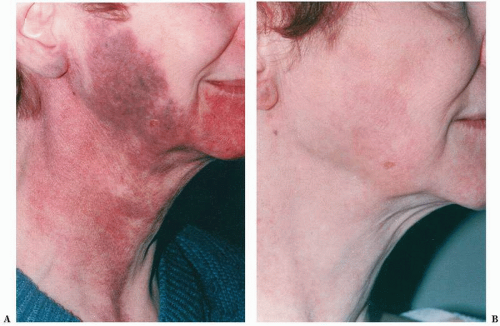 FIGURE 5-3 ▪ Congenital port wine stain hemangioma before (A) and after (B) treatment with candelapulsed tuneable 585-nm dye laser. |
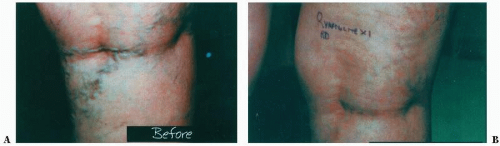 FIGURE 5-4 ▪ Varicose veins of the leg before (A) and after (B) treatment with Lumenis Vasculite laser. |
Fractional Laser Therapy
Fractional laser therapy is based on the principle of selective photothermolysis. A specific wavelength of light is selected, which is matched to a target in the skin such as hemoglobin, water, and melanin. It is then delivered rapidly enough to limit thermal damage to the target before it diffuses out to the surrounding tissue. With the fractional laser a microarray of laser energy is delivered, creating zones or microscopic tunnels of thermal damage in the epidermis and dermis separated by intervening areas of undamaged tissue. In other words, only a fraction of the area is treated. This allows for more rapid healing and for less risk of adverse outcomes. Fractional laser therapy is used for photodamaged skin, melasma, atrophic acne scars, and surgical scars. Two of the popular fractional lasers are the Fraxel SR laser, which is an erbium-doped 1550-nm device with fluences from 35 to 40 mJ per microthermal zone, and the Palomar Lux 1540 Fractional laser, which is an erbium-doped 1540-nm device with fluences of 70 mJ per microthermal zone. Since only a fraction of the area is treated at one time, treatments are carried out every 3 to 4 weeks for four to eight times.
Intense Pulsed Light
IPL is a noncoherent, broad band of wavelengths from 515 to 1,200 nm generated by a high-energy flash lamp. For treatment, wavelengths of light are selected by the use of optical cut-off filters that eliminate wavelengths less than the filter’s wavelength of light transmission. The first IPL device was the Photoderm system by Lumenis. There are other good systems available, such as the Palomar. Initially in the mid-1990s, the IPL was promoted for the treatment of leg veins, but the indications for IPL have greatly expanded and leg veins are the least indication. IPL is very effective for:
Facial telangiectasias (Fig. 5-6)
The vascular component of rosacea
Poikiloderma of Civatte
Mottled facial pigmentation from actinic damage (Fig. 5-7)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree