Disorder |
Cutaneous Findings |
Associated Malignancies |
Acanthosis nigricans |
Velvety hyperpigmentation of flexures and, less commonly, mucosal surfaces and palms (tripe palms) |
Adenocarcinoma of genitourinary or gastrointestinal tract. Most commonly associated with adenocarcinoma of the stomach (55.5%)* |
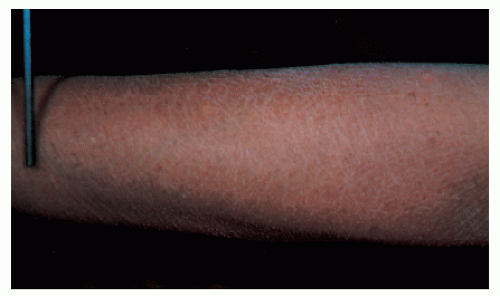
Acquired ichthyosis |
Adult onset hyperkeratosis indistinguishable from ichthyosis vulgaris |
Hodgkin’s lymphoma, mycosis fungoides, multiple myeloma, leiomyosarcoma |
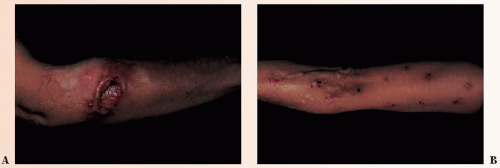
Acrokeratosis paraneoplastica (Bazex syndrome) |
Acral psoriasiform plaques with nail dystrophy |
Carcinomas of upper digestive and respiratory tracts. Also described in association with transitional cell bladder carcinoma† |
Carcinoid syndrome |
Deeply erythematous or violaceous flushing of upper body associated with pruritus, diaphoresis, lacrimation, and facial edema |
Foregut, midgut, and bronchial neuroendocrine tumors |
Cushing’s syndrome |
Generalized hyperpigmentation, including areolae, palmar creases, and scars; hirsutism; central obesity; moon facies, striae |
Ectopic ACTH production by small cell lung cancer, bronchial carcinoid tumors and cancers of the thyroid, pancreas, and adrenals |
Dermatomyositis |
Heliotrope dermatitis, proximal nail fold telangiectasias, Gottron’s papules, cutaneous necrosis |
Ovarian, gastrointestinal, and nasopharyngeal carcinomas; adenocarcinomas of the lung and prostate; hematologic malignancies |
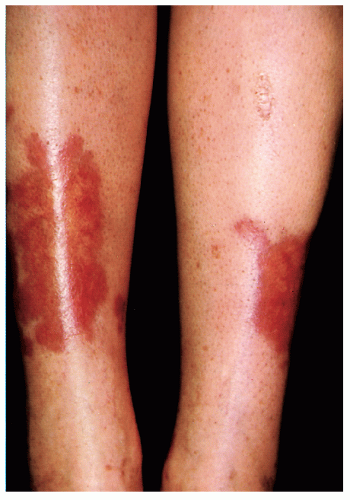
Erythema gyratum repens |
Migratory figurate erythema with “wood grain” pattern |
Malignancies of the lung, breast, female reproductive tract, gastrointestinal tract, and prostate |
Hypertrichosis lanuginosa acquisita |
Excessive growth of vellus hairs on neck and face, but can involve any body surface |
Most commonly observed with colorectal, breast, and lung cancers |
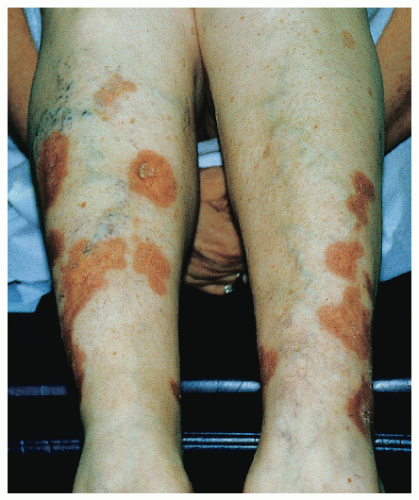
Necrolytic migratory erythema |
Acral and intertriginous papulosquamous dermatitis with occasional vesiculation |
Pancreatic α-cell tumor presents with glucagonoma syndrome |
Paget’s disease |
(1) Unilateral eczematous nipple plaque (2) Eczematous plaque of the anorectal, genital, and axillary regions (extramammary Paget’s disease) |
(1) Associated with ductal adenocarcinoma (2) Regional associations are (a) anorectal—adenocarcinoma of the anus and colorectum, (b) vulvar—epithelial, eccrine, and apocrine neoplasms, and (c) male genitourinary reproductive tract malignancies |
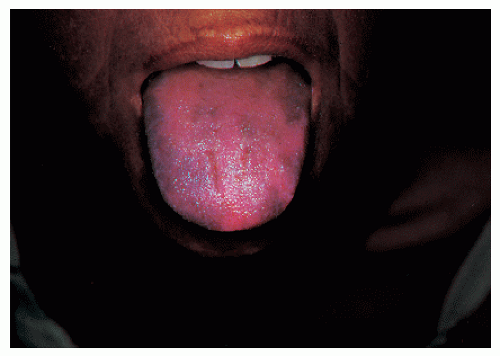
Paraneoplastic pemphigus |
Diffuse mucocutaneous involvement with blisters, erosions, lichenoid, and erythema multiforme-like lesions. Head and neck skin is usually spared. Extensive oral erosions are notable. |
Hematologic malignancies |
Porphyria cutanea tarda |
Vesicles and bullae with subsequent scarring, skin fragility on the dorsal hands, milia formation, and hypertrichosis on sun-exposed surfaces |
Hepatocellular carcinoma, hematologic malignancies, myelodysplastic syndromes |
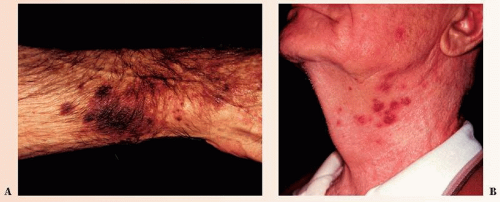
Sweet’s syndrome—atypical bullous pyoderma gangrenosum overlap |
Indurated erythematous to violaceous plaques with or without bulla formation and ulceration |
Hematologic malignancies, myeloproliferative disorders |
Sign of Leser-Trélat |
Eruptive multiple seborrheic keratoses |
Adenocarcinomas of the lung and gastrointestinal tract |
* From Rigel DS, Jacobs MI. Malignant acanthosis nigricans: a review. J Dermatol Surg Oncol. 1980;6(11):923-927.
† From Arregui MA, Raton JA, Landa N, et al. Bazex’s syndrome (acrokeratosis paraneoplastica)—first case report of association with a bladder carcinoma. Clin Exp Dermatol. 1993;18(5):445-448. |
Abbreviations: ACTH, Adrenocorticotropic hormone. |