Name (units) |
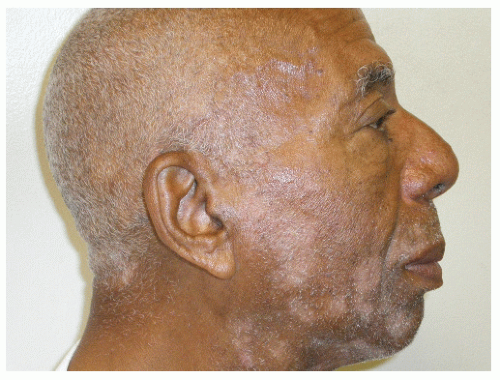
Fitzpatrick Scale (FZ) |
Roberts Hyperpigmentation Scale (H) |
Glogau Scale (G) |
Roberts Scarring Scale (S) |
Scale |
Measures skin phototypes |
Propensity for pigmentation |
Describes photoaging |
Describes scar morphology |
Categories |
FZ1 White skin. Always burns, never tans |
H0 Hypopigmentation |
G1 No wrinkles, early photoaging |
S0 Atrophy |
|
FZ2 White skin. Always burns, minimal tan |
H1 Minimal and transient (<1 year) hyperpigmentation |
G2 Wrinkles with motion, early to moderate photoaging |
S1 None |
FZ3 White skin. Burns minimally, tans moderately and gradually |
H2 Minimal and permanent (>1 year) hyperpigmentation |
G3 Wrinkles at rest, advanced photoaging |
S2 Macule |
|
FZ4 Light brown skin. Burns minimally, tans well |
H3 Moderate and transient (<1 year) hyperpigmentation |
G4 Only wrinkles, severe photoaging |
S3 Plaque within scarred boundaries |
|
FZ5 Brown skin. Rarely burns, tans deeply |
H4 Severe and transient (>1 year) hyperpigmentation |
|
S4 Keloid |
|
FZ6 Dark brown/black skin |
H5 Severe and transient (<1 year) hyperpigmentation |
|
S5 Keloid nodule |
|
|
H6 Severe and permanent (>1 year) hyperpigmentation |
|
|
Note: Reprinted with permission from Roberts WE. The Roberts skin type classification system. J Drugs Dermatol. 2008;7(5):452-456. |