Red Papules and Nodules
Peter J. Lynch
Genital disorders that present as red papules or nodules are most often either neoplasms or inflammatory lesions. Vascular neoplasms present as bright red, dusky red, or violaceous papules and nodules with sharply demarcated borders. Nonvascular neoplasms are also sharply marginated but tend to be lighter red in color. Inflammatory papules and nodules are most often medium to dark red toward the center and fade to light red or pink at their less distinctly marginated borders. Most of the lesions considered in this chapter lack scale and therefore are smooth surfaced. Many skin-colored papules and nodules appear pink or red at times because of secondary inflammation or increased vascularity. This is particularly notable in patients with a light complexion. Therefore, when encountering pink or red papules or nodules, the clinician may also need to consider lesions from Chapter 12. The lesions in the first part of this chapter represent the smaller lesions (the red papules) and those in latter part represent the larger lesions (the red nodules). Note, however, that this is not a hard and fast distinction since some of the conditions discussed may present with a mixture of papules and nodules.
FOLLICULITIS
Both bacterial and dermatophyte fungal folliculitis can present as small red papules. (Figs. 7-1 and 7-2). Generally, multiple, often clustered, lesions are present. At least a few of these lesions will have a white or yellow-white pustule at the summit. This distinguishing feature, followed by appropriate culture, allows for establishment of the correct diagnosis. The primary discussion of these conditions can be found in Chapter 8, The Purulent and Pustular Disorders.
KERATOSIS PILARIS
Clinical Presentation
Keratosis pilaris (KP) is a noninfectious form of folliculitis. It is a very common condition with a prevalence of about 10% in children and 2 or 3% in adults (1). The prevalence of KP gradually decreases with age and it is not often seen after the fourth decade. The clinical appearance is that of minute (1 to 2 mm) closely set, clustered papules. Some, but not all of the papules will have a small hair emerging from the summit of the papule. All of the lesions are approximately the same size and are equidistant from one another (Fig. 7-3). This lends a monomorphic appearance to the process.
In those individuals with the least severe involvement the papules may be skin-colored or pink, but in most patients, both the papules and a narrow halo around them are distinctly red. A few of the larger lesions may be capped by a firm, solid, white summit (pseudopustule) consisting of compacted keratin retained in the follicular orifice. If this solid white “ball” of keratin is scraped away, it sometime contains a fine, rolled-up hair within it. The most commonly involved sites are the upper arms, thighs, and buttocks. There is a sandpaper-like, slightly rough, feel when the fingertips are lightly passed over clustered lesions of KP. KP is usually asymptomatic though mild pruritus is sometimes present.
Diagnosis
KP is diagnosed on a clinical basis. The key features include (i) a large number of closely set homogeneous papules, (ii) location on lateral, upper arms, thighs, and buttocks, (iii) long duration with little or no change in clinical appearance, and (iv) failure to respond to antibiotic therapy.
KERATOSIS PILARIS: Diagnosis
Clustered, small (1 to 2 mm) red papules
Hairs emerging from the summit of some papules
Location on the arms, thighs, and/or buttocks
Rough, sandpaper-like feel on palpation
Failure to respond to antibiotics
Pathophysiology
KP is caused by excess keratinization (keratin plugging) of the outermost portion of hair follicles. The cause of this accumulation of keratin is unknown but it is likely related to an abnormality of keratinocyte differentiation since KP occurs primarily in those with ichthyosis vulgaris and atopic dermatitis, two conditions that are
almost always associated with keratinocyte differentiation abnormalities secondary to mutations in the filaggrin gene.
almost always associated with keratinocyte differentiation abnormalities secondary to mutations in the filaggrin gene.
Management
No therapy is necessary. This is fortunate as no treatment is very effective. Patients who are bothered by the appearance or the pruritus may periodically undertake a prolonged bathtub soak followed by the use of light abrasion with a loofah sponge or soft brush. Lubrication, especially with products containing humectants such as urea or alpha hydroxy acids, improves the textural feel of the skin. Topical retinoids, while theoretically attractive as therapeutic agents, tend to increase the inflammation and thus are not routinely useful.
KERATOSIS PILARIS: Management
20-minute bathtub soak
Light scrubbing with a soft brush or loofah
Application of a moisturizer after soak and scrub
Cautious trial of topical tretinoin
NODULAR SCABIES
The primary discussion of scabies can be found in Chapter 14. Only the nodular form of the infestation will be considered here. Nodular scabies occurs as a hypersensitivity reaction to mite proteins. It occurs weeks or months after the initial lesions of scabies are first noted and often develops after successful treatment of more generalized disease. The lesions contain no live organisms and thus are not a cause of transmission to others.
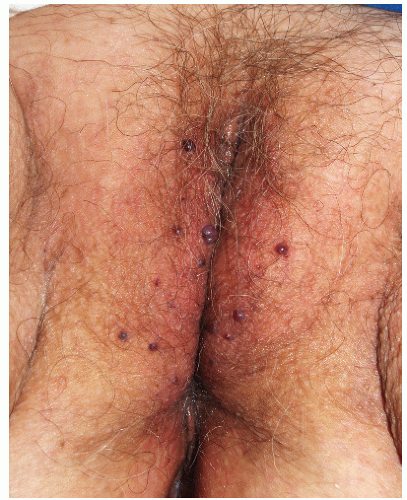
Nodular scabies occurs almost solely in males. The reason for this site and gender predilection is unknown. The lesions of nodular scabies may be papules or nodules or a mixture of both. These dome-shaped, red to brown-red lesions are usually 5 to 20 mm in diameter (Figs. 7-4 and 7-5). The surface of some of the lesions may demonstrate erosions occurring as a result of excoriation. Nodular scabies
has a special predilection for the glans penis, penile shaft, and scrotum but occasionally lesions are found in the pubic region, groin, buttocks, and axillae. The clinical features overlap appreciably with the lesions of prurigo nodularis. The correct diagnosis is usually established on the basis of clinical features, but when uncertainty is present, biopsy, while not usually revealing the presence of mites, ova, or feces, does demonstrate a characteristic heavy infiltrate of eosinophils.
has a special predilection for the glans penis, penile shaft, and scrotum but occasionally lesions are found in the pubic region, groin, buttocks, and axillae. The clinical features overlap appreciably with the lesions of prurigo nodularis. The correct diagnosis is usually established on the basis of clinical features, but when uncertainty is present, biopsy, while not usually revealing the presence of mites, ova, or feces, does demonstrate a characteristic heavy infiltrate of eosinophils.
 FIG. 7-4. These lesions on the penis and scrotum, with a predilection for the glans, are typical of nodular genital scabies. |
Left untreated, the lesions of nodular scabies may persist for months but do eventually resolve spontaneously. Assuming that the patient has been successfully treated for more generalized infestation, repeated applications of scabicides are not helpful. The use of high-potency topical steroids does little to improve the situation. However, improvement in both the pruritus and appearance of the lesions can be obtained with intralesional injections of 0.2 to 0.4 mL of triamcinolone acetonide (Kenalog), 10 mg/mL, into each lesion.
MISCELLANEOUS BITES AND INFESTATIONS
Insect bites in the genital area are uncommon because this area is usually protected by clothing. However, such bites do occur in campers and hikers who expose the genital area when urinating, defecating, or having intercourse alfresco. The most common of these bites are due to chiggers. Chiggers, also called harvest mites, bite and fall off, rather than burrowing into the skin as occurs with the scabies mite. In nonsensitized people, chigger bites are tiny red papules that are minimally symptomatic and resolve quickly. However, those patients who are allergic to chigger proteins develop extremely pruritic, pink, nonscaling, dome-shaped 0.5- to 1.5-cm papules, occasionally with a central vesicle (2) (Fig. 7-6). Such bites are particularly likely to occur where clothing binds against the skin such as at waistbands. Lesions due to chigger bites resolve spontaneously in about 2 weeks. Oral antihistamines and topical steroids provide some symptomatic improvement. The best approach is to avoid the possibility of chigger bites through the use of standard insect repellents.
Lesions due to other biting insects (Fig. 7-7) also appear as pruritic red papules. While there is nothing that clinically identifies which insect is responsible, the likelihood that a given red papule is due to some type of insect bite can be ascertained by the presence of numerous eosinophils within the inflammatory infiltrate in a biopsy specimen.
CHERRY ANGIOMA
Cherry angiomas (Campbell de Morgan spots) represent a benign neoplasm of clustered capillary blood vessels. They first appear in young adult life and generally increase with age. These angiomas occur as sharply marginated dome-shaped papules that are bright red, dusky red, or even violaceous in color (Fig. 7-8). They vary in size from nearly flat, pinpoint lesions to 3- to 6-mm papules. The majority of light-skinned persons will have developed at least one by age 40 and the average adult has 30 to 50 scattered lesions. Cherry angiomas are most commonly found on the trunk and proximal extremities but occasionally are also noted on the pubis and genitalia.
The cause of cherry angiomas is not known though the frequency of familial development suggests a genetic predisposition. The diagnosis is made on a clinical basis. The differential diagnosis is that of angiokeratomas. Since both are asymptomatic and benign it is not really necessary to differentiate these lesions. No treatment is necessary. Lesions that bleed frequently with trauma may be excised or may be destroyed with electrosurgery or laser ablation.
ANGIOKERATOMA
Angiokeratomas represent clusters of ectatic superficial cutaneous blood vessels. These asymptomatic papules are sometimes given the eponymous epithet of Fordyce but should not be confused with Fordyce spots referring to prominent sebaceous glands on the lip or genitalia.
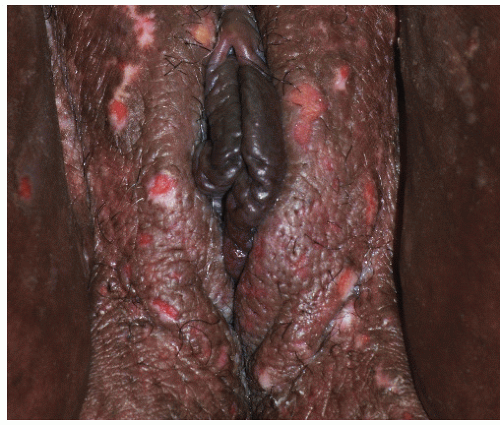
Angiokeratomas are sufficiently common to be considered as a normal variant rather than a disease. The prevalence is not known, but based on our experience they develop in early adulthood in about 10% of men but less that 1% of women. In men they appear as 1- to 2-mm red, smooth-surfaced, dome-shaped papules occurring primarily on the scrotum and, rarely, on the penile shaft (Fig. 7-9). Sometimes they are lined up as minute (“beads on a string”) outpouchings along a linear telangiectatic vessel. Generally 10 to 30 papules are present. In women, the lesions are found on the labia majora where they are fewer in number (often solitary), larger in size (3 to 8 mm), and darker in color (dusky red, violaceous, or blue) (Fig. 7-10). In both sexes, they are asymptomatic.
The diagnosis is made on a clinical basis. In men they may resemble benign cherry angiomas (Campbell de Morgan spots). The angiokeratomas found in the extremely rare condition, angiokeratoma corporis diffusum (Anderson-Fabry disease), are similar in appearance but in this life-threatening systemic disorder they are more numerous and occur throughout the lower
trunk and upper thighs. In women, darker lesions may be confused with nevi or even melanoma. Histologically, clustered, dilated vessels are noted in the upper dermis. The overlying epidermis is slightly thickened and elongated rete ridges usually extend into the dermis around the vessels, sometimes entirely encircling them. The cause of these lesions is unknown. However, based on their frequent occurrence along a dilated vessel in men, it is possible that they develop as saccular varices in aging, weak-walled capillaries.
trunk and upper thighs. In women, darker lesions may be confused with nevi or even melanoma. Histologically, clustered, dilated vessels are noted in the upper dermis. The overlying epidermis is slightly thickened and elongated rete ridges usually extend into the dermis around the vessels, sometimes entirely encircling them. The cause of these lesions is unknown. However, based on their frequent occurrence along a dilated vessel in men, it is possible that they develop as saccular varices in aging, weak-walled capillaries.
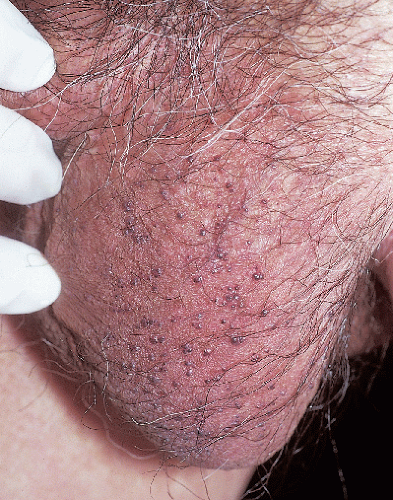 FIG. 7-9. Some patients exhibit large numbers of angiokeratomas, such as these tiny dark purple scrotal lesions. |
PRURIGO NODULARIS (PICKER’S NODULE)
Clinical Presentation
Prurigo nodules occur in patients who chronically pick or scratch at a small area of skin. This produces a callus-like reaction as the epithelial cells proliferate and produce increased amounts of keratin in response to chronic trauma (3). Individual lesions are 0.5- to 1.5-cm pink, red, or brown-red papules usually with overlying excoriation (Figs. 7-11 and 7-12). The surface is palpably rough due to the presence of compacted scale. Generally no primary lesions are seen, but occasionally a coexisting underlying problem such as folliculitis is present and serves as a focus for the initial scratching. Prurigo nodules may occur anywhere on the body but are fairly common on the labia majora in women, on the scrotum in men, and in the pubic area in both sexes. Picking may start as a result of pruritus, but habitual picking, often at the subconscious level, plays the major role in the perpetuation of these lesions.
Diagnosis
The diagnosis is made by the clinical appearance and history of scratching or picking. If biopsy is carried out, the histological features are those of epidermal hyperkeratosis with acanthosis and irregular downward proliferation of the rete ridges. Secondary nonspecific inflammation is present and there is usually a proliferation of nerve endings. Nodular scabies, particularly in males, and pseudowarts are the main conditions to be considered in differential diagnosis.
PRURIGO NODULARIS: Diagnosis
Excoriated, rough-surfaced papules or nodules
History of habitual scratching or picking
In some patients there is a belief that “something is in the skin and must be removed”
Confirmation by biopsy, if necessary
Pathophysiology
These nodules arise as a protective, callus-like response of the epithelial cells to the chronic trauma of picking, scratching, and rubbing. The process is analogous to that occurring with the itch-scratch cycle that results in lichenification (see Chapter 4) but is restricted to a much smaller area of skin. Some degree of psychological dysfunction is regularly present. The intensity and repetitiveness of the picking has many features of an obsessive-compulsive disorder.
Management
Treatment consists of the identification and elimination of any underlying pruritic condition such as folliculitis that initiates the picking. Patients with anxiety or depression, a common occurrence, should have these psychological issues addressed. Individual lesions can be treated fairly effectively by intralesional injections of 0.2 to 0.5 mL of triamcinolone acetonide 10 mg/mL. A light freeze with liquid nitrogen may help temporarily because cold temperatures selectively destroy nerve endings before causing other types of tissue damage. High-potency topical steroid therapy is usually prescribed but, used alone, this approach is rarely of help. Nighttime sedation with a tricyclic medication such as doxepin or amitriptyline can minimize scratching during sleep. An orally administered selective serotonin reuptake inhibitor (SSRI), used in doses recommended for the treatment of obsessive-compulsive disease, can be very helpful. In the most severe cases, use of one of the atypical antipsychotic agents may be worth trying. Additional approaches to help break up the itch-scratch cycle are covered in Chapter 4.
PRURIGO NODULARIS: Management
Intralesional steroid injection, triamcinolone 10 mg/mL, 0.2 to 0.5 mL each lesion
Trial of light, liquid nitrogen therapy
Hydroxyzine or doxepin, 25 mg 2 hours before bedtime. Increase weekly to 75 mg, if necessary
SSRI, such as citalopram, if daytime therapy is necessary
PYOGENIC GRANULOMA
This reactive neoplasm is most commonly encountered in children and pregnant women. The genitalia are not a usual site of predilection but there have been a few reported cases involving these areas (4) (Figs. 7-13 and 7-14). Clinically, pyogenic granuloma presents as a red papule or small nodule that is often slightly pedunculated (“pinched in” at the base). Because the surface epithelium of these lesions is markedly thinned, a glistening surface that bleeds easily following minimal trauma is often noted. The diagnosis is generally apparent on clinical examination but many of the lesions discussed in this chapter should be considered in the list of differential diagnoses. Importantly, amelanotic melanoma can closely mimic the appearance of
pyogenic granuloma. For this reason histologic confirmation of a clinical diagnosis is usually warranted.
pyogenic granuloma. For this reason histologic confirmation of a clinical diagnosis is usually warranted.
 FIG. 7-14. This pyogenic granuloma has occurred on a thigh in a background of unrelated lichenification from rubbing. |
Pyogenic granuloma is a benign reactive neoplasm. Bleeding represents the only important complication of these lesions. The cause of pyogenic granuloma is not known but in many cases they arise after trauma, perhaps developing as a result of disturbed normal reparative angiogenesis. Since these lesions occur with much increased frequency during pregnancy and in the prepubertal years of childhood, it is possible that hormonal factors play a role in pathogenesis.
The treatment of choice is shave excision at the level of the surrounding skin. This provides a specimen for histological examination. The base of the excision should be treated with electrosurgery as otherwise the recurrence rate is unacceptably high.
URETHRAL CARUNCLE
Urethral caruncle occurs in middle-aged and elderly women where it appears as a solitary red papule at the urethral meatus (Figs. 7-15 and 7-16). These caruncles are less than 1 cm in diameter and usually occur as pedunculated or dome-shaped lesions. The surface is friable and for this reason they usually come to the attention of the patient because of mild hematuria or the presence of blood on the toilet tissue after wiping. Microscopic features include vascular dilatation and an infiltration of neutrophils in a loose connective tissue stroma. The cause is unknown. Asymptomatic small lesions may be left untreated. If treatment is desirable, the lesion can be removed by shave excision at the base of the lesion. Light electrosurgery may be necessary to achieve hemostasis and prevent recurrence. The removed specimen should be submitted for histological examination to rule out other types of urethral tumors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree