Pediatric Dermatology
Kimberly A. Horii MD
Vidya Sharma MBBS, MPH
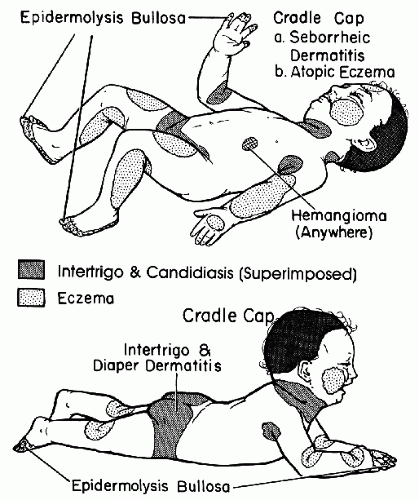
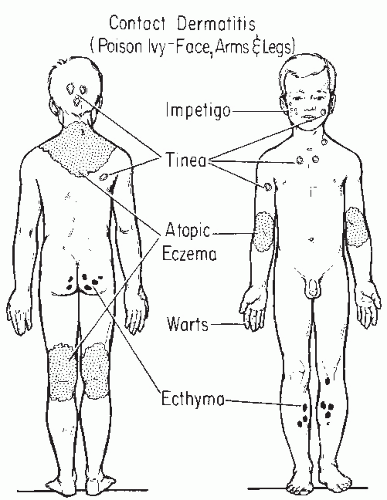
Skin disorders in infants and children may be different from the same diseases in older children or adults (Figs. 41-1 and 41-2). Certain skin conditions such as diaper dermatitis are typically seen only in infants; other conditions such as atopic dermatitis may appear different in children when compared with adults. Pediatric dermatology can be divided into neonatal dermatoses and dermatoses of infants and children. It is useful to describe a lesion by its morphology to develop a differential diagnosis of what the disorder might be.
Neonatal Dermatoses (Birth to 1 Month)
A few lesions may be noted at birth or shortly thereafter (Table 41-1). In the newborn period, an infectious etiology for a skin eruption needs to be ruled out because some neonatal infections can be life threatening.
Blistering (Vesiculobullous) Lesions
Blistering lesions can be mechanically induced or caused by infections.
Sucking blisters: Usually seen as oval bullae on the hand or forearm thought to be caused by sucking in utero. They resolve rapidly.
Epidermolysis bullosa (Fig. 41-3): A group of inherited disorders with fragile skin and bullous lesions that develop spontaneously or as a result of trauma.
Infections (Fig. 41-4): Herpes simplex, congenital varicella, candidiasis, and congenital syphilis can present as blisters in the newborn. Herpes simplex is important to recognize because disseminated neonatal herpes infection can be fatal.
SAUER’S NOTES
1. Pediatric dermatology has become a specialty unto itself.
2. Clinical appearances represent a different differential diagnosis than in adults.
3. Dermatopathology patterns have different meanings than in adults.
4. Numerous dermatology entities are specific for the pediatric age group.
Pustular Lesions
Some pustular dermatoses are self-limited and require no treatment; others may be a result of an infection requiring therapy.
Candidiasis (Fig. 41-4): Aside from blisters, candidiasis may also present with erythematous papules and pustules.
Erythema toxicum: A common, benign, and self-limited condition of the newborn usually noted during the first few days of life. Erythematous macules, papules, and pustules may occur anywhere on the body.
Transient neonatal pustular melanosis (Fig. 41-5): A benign, self-limited disorder characterized by sterile pustules that rupture and evolve into hyperpigmented macules.
Neonatal acne: Papules and pustules develop at 2 to 4 weeks of age. It is self-limited and usually does not scar. Topical erythromycin or benzoyl peroxide may be helpful. Neonatal cephalic pustulosis is considered synonymous by some authors, and response to topical ketoconazole has been reported. The role of yeast is yet to be determined.
Milia: Occurs commonly on the cheeks, nose, chin, and forehead. It presents as 1- to 2-mm white or yellow papules, which are frequently grouped. The lesions resolve without therapy.
Birthmarks
Newborns may have many different types of birthmarks that can be categorized by color.
White
Albinism: An uncommon inherited disorder with lack of pigment in the skin, hair, and eyes. A partial lack of pigmentation is termed piebaldism or partial albinism.
Ash leaf macules: Lance-shaped hypopigmented macules on the trunk, arms, or legs, usually associated with tuberous sclerosis.
Nevus anemicus: A solitary hypopigmented macule resulting from a localized vascular reaction. The surrounding borders classically blanch with pressure.
Nevus depigmentosus: A unilateral hypopigmented patch with poorly defined borders.
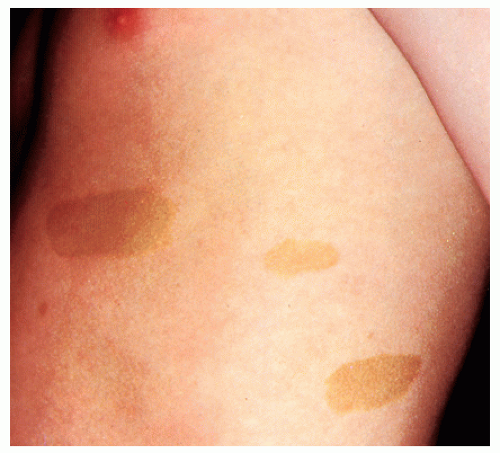
Brown
Café-au-lait spots (Fig. 41-6): Light brown round or oval macules. These can be normal findings, but may be seen in association with neurofibromatosis type I. This condition should be suspected if six or more café-au-lait spots greater than 0.5 cm in diameter are present in association with other clinical findings.
Congenital melanocytic nevus (Fig. 41-7): A tan to dark brown well-circumscribed papule or plaque. Nevi vary in size from small to large, and often have associated hypertrichosis. Congenital nevi have the potential of developing into a melanoma depending on their size (especially >20 cm), location, border (irregular), color (especially black and multicolored), and texture (nodules).
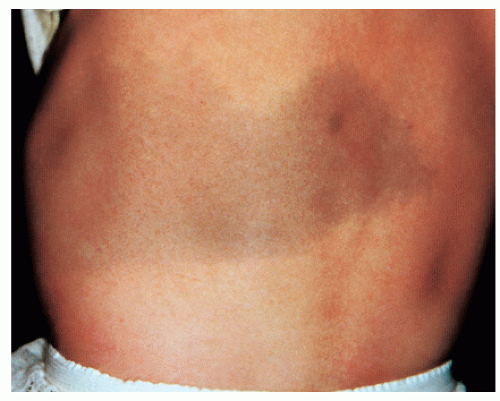
Dermal melanosis (Mongolian spots) (Fig. 41-8): Deep brown, slate gray, or blue-black macules found mostly over the lumbosacral area and buttocks in darker pigmented infants. These are benign and self-limited.
Epidermal nevus (Fig. 41-9): Tan to brown verrucous linear lesions noted at birth. They may rarely have other associated neurologic or skeletal abnormalities.
Vascular
Nevus simplex (Salmon patch) (Fig. 41-10): Dull pink macules on the glabella, upper eyelids, nasolabial regions (also referred to as angel kisses), or nape of the neck (also referred to as a stork bite or devil’s bite). Angel kisses usually fade when present on the face, but stork bites do not.
Port-wine stain (capillary malformation) (Fig. 41-11): A congenital vascular malformation composed of dilated capillaries. These are reddish purple macules or patches that do not involute. Laser therapy is a treatment option. Neurologic and ophthalmologic abnormalities (Sturge-Weber syndrome) may accompany a port-wine stain located on the face above the palpebral fissure.
Hemangioma of infancy (Fig. 41-12): Benign tumors of infancy composed of proliferating vascular endothelium. They grow rapidly in infancy, stabilize, and involute in childhood, most resolving by 10 years of age. They may be superficial, deep, or mixed. A new classification system separates hemangiomas based upon their configuration. Localized hemangiomas are symmetric and confined to a limited space. Segmental hemangiomas are large and appear to follow a geographic territory of the body (Fig. 41-13). Segmental hemangiomas can be associated with underlying anomalies and have been
associated with more complications and may require treatment more frequently. Numerous cutaneous lesions may be associated with hemangiomas in the viscera. Large facial hemangiomas may be associated with neurologic, ophthalmologic, and cardiac abnormalities (PHACE syndrome). Management may consist of observation alone, oral prednisolone, laser treatment, chemotherapy (interferon-α and vincristine), or surgery. Initial case series have also shown improvement with the use of propranolol.
TABLE 41-1 ▪ Neonatal Dermatoses (Birth to 1 Month) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Yellow
Nevus sebaceous: Noted at birth as a yellow orange oval or linear area of alopecia on the scalp. At puberty they become raised and warty. Basal cell carcinomas and squamous cell carcinomas can rarely develop within the nevus later in life. A benign warty tumor called syringocystadenoma papilliferum may occur in conjunction with a nevus sebaceous.
Papulosquamous Lesions
Ichthyosis (Fig. 41-14): Associated with dry, fishlike adherent scales. The rarer lamellar form and congenital ichthyosiform erythroderma are present at birth and may present with a shiny, tight layer of skin called a collodion membrane. Ichthyosis vulgaris, which is the commonest form, and X-linked ichthyosis are usually not present at birth.
Neonatal lupus erythematosus (Fig. 41-15): Characterized by congenital heart block and annular papulosquamous skin lesions on the forehead and cheeks. The skin lesions usually fade by 6 to 7 months of age while the heart block persists. Because this is maternally transmitted, the mother also needs to be evaluated for lupus. Anti-Ro or SSA and anti-La or SSB antibodies may be present in the mother or newborn.
 FIGURE 41-4 ▪ Candidiasis and syphilis. (A and B) Extensive candidiasis. (C) Congenital syphilis with hepatomegaly and splenomegaly. |