Nutritional and Metabolic Diseases and the Skin
Brian J. Hall MD
Nutrition will always play an important role in the maintenance and protection of the skin. As more is being discovered about the foods we eat and more attention is being paid to different vitamins and minerals, we will undoubtedly find out more important information regarding nutrition and its role in skin maintenance as well as skin disease. Also, problems associated with developing countries are becoming more important as more people continue to migrate to the United States from abroad. Due to the increasing elderly population in the United States, adequate nutritional intake among the elderly will continue to be a very important subject for clinicians to be attentive to. Diet is many times inadequate in elderly populations and does not contain enough variety to provide elderly patients with all of the nutrients that they need. Also, as Americans have enjoyed an excess of food in recent times, one of our biggest problems is obesity and the medical problems it creates for them. The skin is not immune to these problems. We will also discuss how different metabolic diseases can have profound effects on the skin.
Vitamin Deficiencies
Vitamin A Deficiency
Presentation and Characteristics
Vitamin A deficiency is mainly a disease limited to the developing countries. One of the first signs of deficiency is night blindness, and it is the leading cause of blindness in developing countries. The most striking characteristic of the skin associated with vitamin A deficiency is phrynoderma. It is marked by follicular hyperkeratosis with spinous papules at the end of hair follicles. It is symmetrically distributed and often initially located at the extensor surfaces of the thighs and forearms. Many times this hyperkeratosis causes the patient’s skin to appear like toad skin and it sometimes occurs on a background of dry and rough skin that may feel like sandpaper or nutmeg grater. The worst cases often plague children of preschool age. Other signs of deficiency include keratomalacia, pruritis, broken fingernails, and keratinization of mucous membranes. Even mild deficiencies can have a profound effect on a child’s immune system and can increase the child’s chances of dying from other childhood illnesses such as measles.
SAUER’S NOTES
As foreign travel and the global economy expand, vitamin and mineral abnormalities are a group of illnesses in which all specialists need to develop awareness.
Treatment
Skin lesions recover impressively with retin-A cream. Nutritional state can be improved with cod liver oil, palm oil, carrots, sweet potatoes, leafy green vegetables, fruits, and a variety of meats such as liver. Daily oral supplements can be given for vitamin A deficiency and are listed in dosages depending on age: children 3 years or younger—600 µg (2,000 IU); children aged 4 to 8 years—900 µg (3,000 IU); children aged 9 to 13 years—1,700 µg (5,665 IU); children aged 14 to 18 years—2,800 µg (9,335 IU); and all adults—3,000 µg (10,000 IU).
Prevention
Eating a healthy diet with plenty of fruits and vegetables and a variety of other foods is the best prevention for vitamin A deficiency. Besides the foods listed in the previous section, fortified milk, whole milk, chicken, beef, and eggs are also rich in vitamin A.
Vitamin A Excess
Presentation and Characteristics
Hypervitaminosis A presents with dry, coarse, scaly skin, hair loss, seborrhea, yellow discoloration of the skin, peeling of skin, fissures of the lips, pruritis, sore tongue or mouth, increased sensitivity to sunlight, and low-grade fever.
Treatment
Elimination of sources of vitamin A and/or carotenoid in the diet or from supplementation.
Prevention
The liver of certain animals such as polar bear, husky, and seal are unsafe to eat due to their extraordinarily high vitamin A content. This fact has been known to Inuit for centuries and even to European explorers since the middle 16th century. It is also extremely important not to take more than the recommended daily allowance (RDA) of this vitamin because the amount over and above the RDA is one of the narrowest of all vitamins and minerals. Especially with recent emphasis on vitamin A and beta-carotene as anticancer agents, accidental chronic overdose (through oral supplementation) is a possible problem. Excessive ingestion of carotenoids (which can cause carotoderma—discussed in the next section) is nontoxic and does not cause hypervitaminosis A because the conversion of carotene to vitamin A is too slow.
Carotenemia
Presentation and Characteristics
Carotenemia is a benign skin condition most often seen in light-skinned patients who have ingested large amounts of foods rich in vitamin A precursors. Carotenemia commonly occurs in vegetarians and young children. This causes a yellow discoloration of the skin excluding the eyes and oral mucosa (Fig. 49-1). It is important to distinguish this condition from more serious conditions such as jaundice. In darkskinned individuals, the palms and soles may have yellow discoloration, but not the rest of the body. This condition more commonly occurs in children with liver disease, hypothyroidism, or diabetes mellitus. Hypothyroidism, diabetes mellitus, hepatic diseases, anorexia nervosa (AN), and renal diseases may be associated with carotenemia unassociated with the ingestion of carotene. Mothers may induce carotenemia by giving their infants large amounts of carrots in commercial infant food preparations.
Treatment
Since carotenemia is a benign condition, it can be treated with dietary modification alone.
Prevention
A lower or more moderate carotene diet will prevent recurrence.
Vitamin B2 (Riboflavin) Deficiency
Presentation and Characteristics
Riboflavin deficiency is associated with perlèche or angular stomatitis (Fig. 49-2), atrophic glossitis (magneta-colored cobblestone tongue), and inflammation of the oral mucosa. A seborrhea-like follicular keratosis may also be observed. It can be generalized, but the areas of the face, chest, abdominal wall, extremities, and genital areas are most severely and consistently affected. On the face it can resemble shark skin and the genital area can show redness with a fine, powdery desquamation.
Treatment
Treatment consists of taking riboflavin 6 to 30 mg PO q.d. until symptoms resolve.
Prevention
Prevention involves eating foods high in riboflavin, such as milk, cheese, yogurt, meat, and vegetables (especially spinach, asparagus, and broccoli).
Vitamin B3 (Niacin) Deficiency
Presentation and Characteristics
Pellagra is the common term used to refer to niacin deficiency and includes the “three D’s” of dermatitis, diarrhea, and dementia. There is sometimes a fourth D referred to because, if left untreated for an extended period of time, death
can result. The diarrhea and dementia are only found in advanced cases. The dermatitis is a symmetrical photodermatitis, affecting sun-exposed areas, areas of friction, or areas of pressure. The patient may report a burning sensation or pain early on. The initial erythema can also subside and darken to a brown color and become brittle, rough, hyperkeratotic, or scaly over time. Almost all patients will have involvement of the dorsal hands (Fig. 49-3). The rash begins in the neck and appears as a broad symmetric hyperpigmented scaly and erythematous collar that has the appearance of a scarf tied around the neck, which then tapers downward, hence the common name “Cassal’s necklace.” The skin rash heals centrifugally with a line of demarcation remaining actively inflamed after the center of the lesion has desquamated.
can result. The diarrhea and dementia are only found in advanced cases. The dermatitis is a symmetrical photodermatitis, affecting sun-exposed areas, areas of friction, or areas of pressure. The patient may report a burning sensation or pain early on. The initial erythema can also subside and darken to a brown color and become brittle, rough, hyperkeratotic, or scaly over time. Almost all patients will have involvement of the dorsal hands (Fig. 49-3). The rash begins in the neck and appears as a broad symmetric hyperpigmented scaly and erythematous collar that has the appearance of a scarf tied around the neck, which then tapers downward, hence the common name “Cassal’s necklace.” The skin rash heals centrifugally with a line of demarcation remaining actively inflamed after the center of the lesion has desquamated.
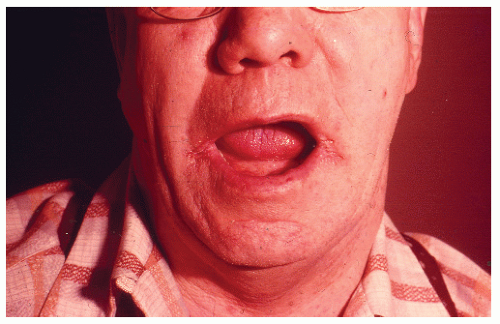 FIGURE 49-2 ▪ Perlèche in any elderly patient such as this one would necessitate a workup for a vitamin B deficiency. |
Treatment
Treatment is supplementation with niacinamide either orally or IV. The usual oral dosage is 0.5 g daily and the usual dosage of an injection is 50 to 100 mg b.i.d. for a period of 3 months. Skin lesions can be covered with emollients, and since sun protection is important during the recovery phase, sunscreen should be applied to all exposed body areas. Since most patients with pellagra also suffer from other vitamin deficiencies, treating the patient with a high-protein diet rich in B-vitamins is also necessary to restore the patient to health. Long-term addition of milk, eggs, and meat is many times necessary to help with recovery. Also, the addition of peanuts, green leafy vegetables, whole or enriched grains, brewer’s dry yeast, and meats can enhance niacin uptake in the acute phase of recovery.
Prevention
Niacin deficiency is rare in Western society. It mainly affects societies whose main dietary intake is maize (which has a low tryptophan content) and millet or sorghum (both of which interfere with tryptophan metabolism due to their high leucine content). Since most of their diet was maize, the Native Americans discovered that they could prevent pellagra by adding lime (an alkali) that makes niacin more available. It is hypothesized that pellagra is caused by not only niacin deficiency but also lack of either tryptophan or one of the vitamin cofactors. However, pellagra does sometimes affect chronic alcoholics, or patients with gastrointestinal disorders or patients with severe psychiatric disturbances in more developed societies like the United States. The main way to prevent pellagra is to have a diet with adequate calories and protein.
Vitamin B6 Deficiency
Presentation and Characteristics
As far as the skin is concerned, a deficiency can paint a similar clinical picture as pellagra since B6 is needed by the body to produce its own B3 vitamin. Although extremely rare, the skin is one of the first organs to show signs of B6 deficiency and can include nails that are uneven (transverse ridging), scaly facial eruptions resembling seborrheic dermatitis, painful, edematous glossitis, angular cheilitis, and generalized stomatitis. Multiple skin disorders including eczema, acne, and seborrheic dermatitis have been associated with B6 deficiency.
Treatment
Pyridoxine 50 to 100 mg PO q.d. is usually sufficient for adults.
Prevention
Vitamin B6 is actually present in most foods, so deficiency is quite rare. As with most vitamin deficiencies, make sure the patient takes in a variety of foods especially poultry, fish, liver, eggs, meat, vegetables, and grains. For patients taking pyroxidine-inactivating drugs such as anticonvulsants, cycloserine, hydralazine, corticosteroids, and penicillamine, the use of pyridoxine in the amount of 50 to 100 mg PO q.d. is recommended. For patients taking isoniazide, a dose of 30 to 50 mg of pyridoxine q.d. is advised.
Vitamin B12 Deficiency
Presentation and Characteristics
Clinically, a patient with a B12 deficiency may present with skin hyperpigmentation (especially over the dorsum of the hands and feet with a concentration over the interphalangeal joints and terminal phalanges), vitiligo, perlèche (angular cheilitis), or glossopyrosis (burning mouth syndrome) that can later result in a focal or diffuse smooth, painful glossitis and hair changes.
Treatment
Treatments can vary but both IM and oral routes are acceptable. IM administration usually involves initial loading doses followed by monthly maintenance doses. One dose of 1,000 µg q.d. × 2 weeks followed by a maintenance dose of 1,000 µg q 1 to 3 months is one example. Oral supplementation is usually 1,000 to 2,000 µg PO q.d. × 2 weeks with a maintenance therapy of 1,000 µg q.d. for life.
Prevention
Since B12 is present only in animal foods and cannot be synthesized by the body, a proper diet including fish, meat, poultry eggs, milk, and milk products is necessary to prevent deficiency. For vegetarians, fortified cereals help prevent deficiency.
Biotin (Vitamin H) Deficiency
Presentation and Characteristics
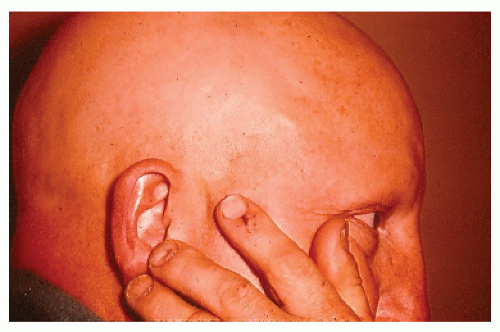
Classically in neonates it presents as a universal alopecia with an extensive bran-like erythematous desquamation that is more pronounced in intertriginous areas. Within 3 to 5 weeks of deficient biotin intake the patient will clinically exhibit seborrheic dermatitis, dry skin, and hair thinning that can progress to total scalp or even universal alopecia (Fig. 49-4) over several months. Other associated signs include: fine and brittle hair without abnormalities of the shaft, fungal infections (especially with Candida albicans), and rashes including periorificial dermatitis with mild, scaly erythema and crusted erosions. Some patients also exhibit keratoconjunctivitis or blepharitis.
Treatment
Treatment with 10 to 20 mg PO q.d. is normally adequate, although quantities up to 40 mg have been used and tolerated by patients.
Prevention
Prevention depends on the cause, and there are a variety of causes for biotin deficiency. Metabolic causes (biotinidase deficiency or holocarboxylase/multiple carboxylase deficiency) cannot be prevented by diet. For deficiencies caused by anticonvulsants a switch to another anticonvulsant medication that does not interfere with absorption must be made or the patients should be supplemented with biotin. For prolonged antibiotic therapy as the cause, the patient should receive biotin supplementation as well if antibiotic therapy must be continued. Otherwise, discontinuation of antibiotic therapy is advised. Patients should also be advised not to consume large amounts of raw eggs as raw egg whites because they both contain avidin. Avidin in large amounts can bind biotin and prevent absorption in the intestine. A dietary deficiency is quite rare, but foods high in biotin include most vegetables, some fruits, chicken, eggs, and milk.
Vitamin C Deficiency (Scurvy)
Presentation and Characteristics
The most distinctive skin finding in scurvy is follicular hyperkeratosis with coiled, corkscrew hairs growing out of the follicles on the upper arms, back, buttocks, and lower extremities. Later patients can get hemorrhagic petichiae in a perifollicular location, ecchymoses, spongy bluish-purple gingivae that may become massively swollen, bleeding of gums, and, in extreme cases, bleeding of all mucous membranes.
Treatment
Treatment is vitamin C 300 to 1000 mg preferably divided into doses of 100 mg throughout the day for at least 1 week and then 400 mg per day until complete recovery.
Prevention
Prevention of scurvy can be accomplished merely by providing a moderate amount of fruits and vegetables in the diet. Foods exceptionally high in vitamin C include bell peppers, brussel sprouts, papaya, broccoli, oranges, strawberries, cantaloupe, kiwifruit, cauliflower, and kale.
Mineral Deficiencies/Excesses
Iron Deficiency
Presentation and Characteristics
Some of the skin signs of iron deficiency include pruritis, brittle nails, nails with vertical stripes, koilonychias (spoonshaped nails), angular stomatitis, a smooth and swollen tongue that can develop a burning sensation, dryness of the throat and mouth, brittle and dry hair, possible increased hair shedding, and pale skin if the patient is anemic.
Treatment
Oral iron therapy is the treatment of choice in most patients; however, the underlying cause of iron deficiency needs to be determined. Iron sulfate 325 mg PO t.i.d. is given for up to 2 months after the anemia has been corrected.