Introduction
Upper blepharoplasty has evolved significantly since its early descriptions focused on rudimentary techniques of skin excision only . In the 20th century, the first detailed description of internal upper eyelid anatomy emphasizing the presence of distinct fat compartments within the eyelid was published . As, on first glance, aged eyelids appear associated with skin, muscle, and fat excess, the trend in surgery was to aggressively excise variable amounts of these tissue substrates to debulk the eyelid and impart what was considered a less prominent and more aesthetic appearance . This “subtractive” form of surgery was in vogue for many years. The desired and accepted upper blepharoplasty result was one with a “hollower” upper sulcus, a high eyelid crease and a prominent tarsal platform . While immediately after surgery patients noted a “ lighter and less baggy ” eyelid, with time many of these changes simulated normal senescence. In the end, many facial surgeons identified that this type of surgery was more a form of iatrogenic aging than a restoration of youth. As the 21st century approached, a more contemporary understanding of facial aging became apparent and surgeons learned that loss of volume is also an essential component of eyelid aging . In addition, it became clear that when planning surgical cosmetic enhancements of the eyelids, their adjacent structures should also be considered to attain appropriate outcomes. In the upper eyelid this meant paying close attention to the eyebrow and its transition to the upper eyelid . Consideration of the lower eyelid and cheek as an aesthetic unit, with emphasis on adjuncts such as fat transposition and augmentation, quickly became the norm . These concepts have lagged behind in regards to the brow and upper eyelid, but more recently have garnered attention .
In this chapter the authors detail various surgical adjuncts to upper blepharoplasty that can be considered to enhance surgical results. These techniques are quick, minimally invasive, easily incorporated to standard blepharoplasty surgery, generally complication free, allow consideration of the brow and eyelid as a continuum, and promote volume preservation. All, except for one browpexy variant , are performed through the blepharoplasty incision, making them easily incorporated into standard eyelid surgery. The importance of these procedures is that they provide the eyelid surgeon with various simple options to potentially enhance surgical results. Prior to the description of these techniques a brief overview of relevant eyelid and periorbital anatomy and aging changes is reviewed.
Clinical Anatomy (Forehead/Eyebrow/Eyelid)
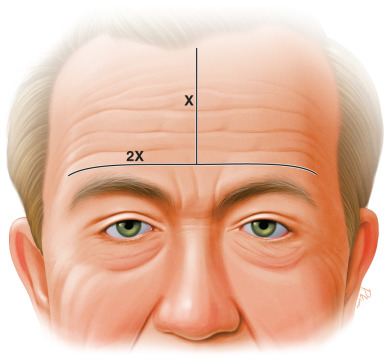
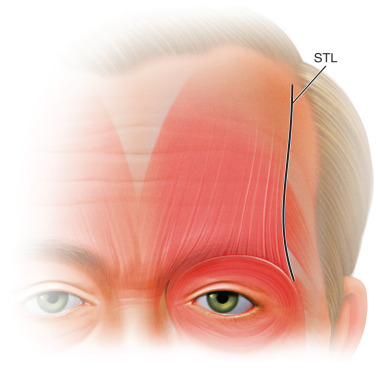
The forehead is a complicated, multilamellar, dynamic structure, which constitutes the upper third of the face. It begins at the hairline and transitions to the upper eyelid at the level of the eyebrow laterally and the glabella and frontonasal groove centrally . Its normal dimensions are a width 2× its height ( Fig. 10.1 ) , and it houses the paired frontalis muscles, which control brow elevation and upper facial animation. The frontalis originates from the galea aponeurotica, which splits and continues above and below the muscle as a superficial and deep layer . The frontalis then inserts into the dermis of the skin above the brow after interdigitating with the orbital orbicularis, corrugator, and procerus muscles . It is innervated by the frontal (temporal) branch of the facial nerve. The lateral extent of the frontalis muscle is the arched superior temporal line at the approximate junction of the body and tail of the eyebrow ( Fig. 10.2 ). Beyond this limit there is no brow elevator, which predisposes this area to normal involutional brow descent . With age, horizontal forehead rhytids develop related to chronic contraction of the frontalis muscle. These rhytids may be effaced with chemo-neuromodulating agents .
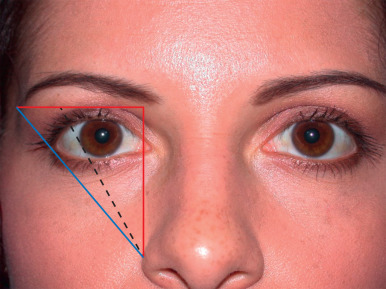
The eyebrow contour, position, and movement are important features of facial expression. The brow cilia are denser and more vertically oriented nasally, and become more horizontal and sparse laterally. Generally speaking, the medial and lateral extent of the brow lie in the same horizontal plane, with the most medial aspect vertically in line with the nasal ala, and the lateral extent in a line drawn obliquely from the nasal ala through the lateral canthus ( Fig. 10.3 ) . There are gender differences in the brow arch and contour, with the male brow being flatter and running over or just below the supraorbital rim, and the female brow arching over the rim with a natural peak in a line drawn tangent to the nasal ala and the pupil or lateral limbus. Below the thick brow skin lies the interdigitation of the frontalis muscle with the brow depressor muscles: the orbital orbicularis oculi throughout and the corrugator and procerus muscle medially. The brow fat pad or retro-orbicularis oculi fat (ROOF) lies below these muscles and above the frontal bone periosteum. The ROOF is encased by the anterior and posterior leafs of the deep layer of the galea aponeurosis . The ROOF fat continues into the eyelid proper as the post orbicular fascial plane in Caucasians and the preseptal fat in Asians . The frontal periosteum merges with the orbital periosteum at the rim, forming the arcus marginalis.
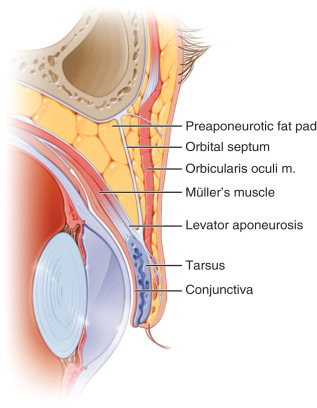
The eyelid skin is thin and intimately adhered to the underlying orbicularis muscle, the protractor of the eyelid. The orbicularis muscle is subdivided into an orbital segment with runs over the orbital rim, and a palpebral segment further subdivided into preseptal and pretarsal divisions named according to their underlying anatomic structures . Like the frontalis muscle, the upper orbicularis oculi muscle is innervated by the frontal branch of the facial nerve. The orbital septum originates at the arcus marginalis periosteum overlying the orbital rim and inserts onto the levator aponeurosis (LA). The septum is an important anatomic landmark as it separates the orbit from the eyelid. It is also an important surgical guide, as when divided eyelid/orbital fat is exposed . This fat lies above the LA. Identifying orbital fat is an important step in blepharoplasty surgery as it defines the location of the aponeurosis, a structure which must be preserved to avoid postoperative eyelid malposition. The levator muscle and aponeurosis function as one of two eyelid retractors, the other being Müller’s muscle. The levator complex originates at the orbital apex with the aponeurosis inserting onto the anterior surface of the tarsus. It is innervated by the upper division of the third cranial nerve. Müller’s muscle (a secondary eyelid retractor), originates from the undersurface of the levator muscle, inserts onto the upper tarsus. It is autonomically driven, and is responsible for eyelid elevation during “fight or flight” responses ( Fig. 10.4 ). Both retractors can be manipulated in ptosis surgery.
Eyebrow/Eyelid Aging
Eyelid and periorbital aging is a complex and multifactorial process involving tissue descent, deflation, and cutaneous changes . As discussed, understanding the role of volume loss with age has been an integral component of contemporary aesthetic eyelid surgery . With age the eyebrow tends towards temporal ptosis, which is both a static and dynamic process ( Fig. 10.5 ). There are lateral brow depressors but no brow elevator beyond the temporal line of the forehead (see anatomy section earlier). As the brow fat pad and its underlying skeleton involute with age, the lateral brow structurally loses support. At the same time, the dynamic action of the brow depressors continues unopposed, predisposing to temporal ptosis. Brow position can be altered by many factors, and certainly there are those whose brows elevate with age , for instance as a result of compensation for true eyelid ptosis. However, as a general rule, the temporal brow tends to drop with age.

The upper eyelids also have characteristic age-related changes. These include true or apparent skin/muscle and fat excess, most obvious temporally (hooding), contour changes with shadowing, central hollows (A-frame changes), and changes in lid height (ptosis; Fig. 10.5 ) . Eyelid ptosis, and its correction, are covered in another chapter. As the temporal brow falls the outer part of the eyelid becomes fuller. For this reason, a temporal brow lift is often a needed adjunct to upper blepharoplasty. The fat pads of the upper lid are different in make-up and clinical appearance, which may lead to some typical age-related eyelid changes . The nasal fat is denser, paler, relatively stem-cell rich, is an extension of deep orbital fat. It is not separated from deeper fat by the LA, and clinically becomes more prominent with age. The central fat is separated from deeper fat by the LA and is thus called preaponeurotic fat. It is less dense, more yellow, relatively stem cell deficient, and tends towards clinical involution with age. The differences in clinical appearance of the fat pads explains why traditional upper blepharoplasty has focused more on nasal than preaponeurotic fat excision .

Indications
All surgical adjuncts reviewed are appropriate additions to standard upper blepharoplasty in patients aware of the potential benefits and limits of each intervention. Standalone blepharoplasty in the presence of brow ptosis can further lower the brow, crowd the upper eyelid, and lead to unnatural results. Browpexy is not a proven brow lifting technique, but rather serves to stabilize the brow position. It is a good option in patients averse to more invasive brow lifting surgery. The external variant, which may rarely be associated with visible scarring , is best suited for men with thicker brow cilia. There are no evidence-based studies proving the utility of nasal fat preservation, and patients should be told that data on surgical outcomes is anecdotal and based on individual surgeon experience. However, the authors are well-versed on these techniques and, with some experience, have found them generally complication free and easy to learn. In addition, the contemporary awareness that fat is a precious commodity within the eyelid should be explained to patients and stimulate surgeon adaptation to these interventions. Lacrimal gland suspension should clearly be discussed with patients who have obvious clinical gland prolapse on preoperative examinations. The decision on suspending a subclinical prolapse (isolated surgical finding) is at the discretion of the operating surgeon. Finally, and probably most controversial, is whether the addition of brow fat-suspension sutures is a warranted addition to blepharoplasty. Again, the authors have significant experience with this technique with only very minor and temporary complications. The authors also feel that brow fat pad suspension does enhance aesthetic outcomes (see discussion).
Surgical Procedures
Internal and External Browpexy
As reviewed, temporal brow ptosis can accentuate temporal eyelid hooding and create a tired and aged appearance. Since this is a common age-related phenomenon, stabilization or elevation of the outer brow has become an essential adjunct to aesthetic upper blepharoplasty . Formal brow lifting procedures are invasive, costly, and carry risks of motor and sensory neurological injury . A browpexy is a minimally invasive method for anchoring the brow tissue (muscle/fat) to the periosteum of the frontal bone . It can provide stabilization or even minimal lift to the temporal brow in conjunction with standard blepharoplasty surgery. In the internal variant, described by McCord and Doxanas , the subbrow tissue is accessed through an upper eyelid crease incision, and the brow fat pad is dissected free of the frontal periosteum. The targeted periosteal suspension location is measured directly and a 4-0 Prolene suture engages the periosteum at this location. The subbrow tissue is then engaged at the inferior aspect of the brow (from the internal wound) with the same suture and tied, anchoring the brow tissue. A total of two or three sutures are placed in this way to secure the brow fat pad to its new position. Modifications of the procedure have been described and include extended preperiosteal dissection, release of deep retaining ligaments of the brow, extirpation of the temporal brow depressor muscle (lateral orbital orbicularis oculi), and the use of anchoring devices screwed into the frontal bone (ENDOTINE; Coapt Systems, Palo Alto, CA, USA; Fig. 10.6 ) . All these procedures have been reported to give good results with few complications. The authors of this chapter rarely perform internal browpexy as they prefer the external variant described later. However, when using this technique they typically extend the dissection and release the deep ligaments. These modifications have improved outcomes. In general, many surgeons feel the internal browpexy does not provide more than short-term results. This can be attributed to surgeon experience, limitation of dissection, weakness of the procedure, or some combination thereof. There is one report in which a central (1.12 mm) and lateral (1.77 mm) brow lift was achieved at 8.5 months’ follow-up .
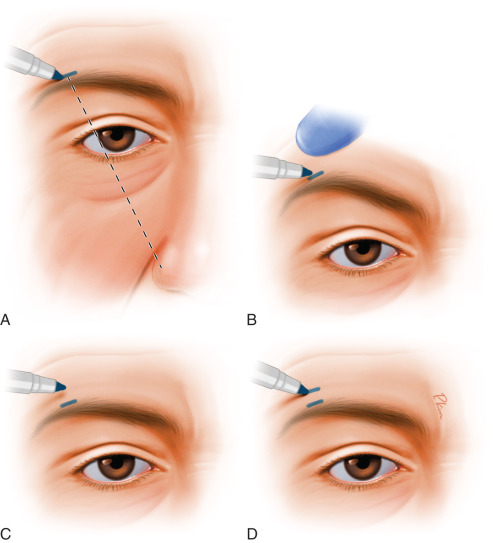
More recently, an external variant of the browpexy procedure has been described, which has been called the “external browpexy” . The idea for this procedure developed from observing patients who had traumatic full-thickness lacerations above the brow, down to the bone. Some of these trauma patients developed a localized elevation and peak in the brow as they healed. Extrapolating from these observations, this technique creates a controlled full-thickness incision to the periosteum with suture anchor of the brow in the area of desired lift. Patient marking is performed in the preoperative area in the sitting position. A 7- to 8-mm mark is made within or along the superior border of the eyebrow cilia, at the junction of the body and tail of the brow. The location should correspond to a line drawn through the nasal ala and lateral limbus, but may be modified depending on patient desires and gender. A finger is then used to elevate this area to the desired brow height. The marking pen is placed at the level of the upper border of the eyebrow at this new height, and the brow is allowed to return to its resting position. Without moving the marking pen down, a second mark is then made on the skin above the brow at this new desired height ( Fig. 10.7 ). The distance between the two marks is the amount of lift to be achieved. The location of elevation (fixation) can be measured as the distance of the second mark from the orbital rim in millimeters. A linear incision is made to the periosteum at the previously marked area just above the eyebrow hairs. While the external incision is small, an internal dissection extends medially and laterally to the periosteum for about 25 mm or 3× the length of the external incision. The internal dissection allows for more raw surface area to form a larger cicatrix to support the brow postoperatively. A 4-0 Prolene suture engages the periosteum at the premarked brow height. This height can be confirmed by measurement from the orbital rim. Interestingly, the authors have found that this height almost always corresponds to the new position of the brow while the patient is supine and after injection of anesthetic agent. The suture is then passed from below, through the brow fat pad/orbicularis muscle and then redirected from above through the orbicularis muscle/brow fat pad and tied. As the knot is tied, elevation and anterior rotation of the brow is achieved. The wound is then closed in layers ( Fig. 10.8 ).