Dermatoses of Pregnancy
J. K. Shornick MD, MHA
The dermatoses of pregnancy can be extremely confusing. Several reported entities have not survived the scrutiny of time. It is doubtful whether perpetuating their inclusion in any current classification scheme serves any useful purpose. In the end, the vast majority of rashes specific to pregnancy can be relegated to one of four categories: pemphigoid gestationis (PG; herpes gestationis), pruritic urticarial papules and plaques of pregnancy (PUPPP), prurigo of pregnancy, and cholestasis of pregnancy.
Needless to say, the pregnant woman is subject to the entire repertoire of the dermatologist’s trade. Often the first challenge is to decide whether pregnancy is relevant to the current condition or not.
Terminology
The generally accepted current classification of skin diseases specific to pregnancy is listed in Table 48-1.
Pemphigoid Gestationis (Herpes Gestationis)
PG is the prototype of rashes specific to pregnancy. It is almost always associated with pregnancy. There are, however, multiple reports of PG in association with choriocarcinoma or trophoblastic tumors in women. There are no reports of a PG-like disease in association with choriocarcinoma in men. Thus, PG appears to be exclusively associated with the presence of placentally derived tissue.
Although the least common pregnancy-related dermatoses (occurring in approximately 1:50,000 pregnancies), PG is the most clearly defined skin condition, and the most important to exclude. It remains idiopathic, although it is invariably associated with pregnancy (or trophoblastic tissue), carries a genetic predisposition, and is immunologically mediated.
SAUER’S NOTE
The chapter author has done an impressive job of summarizing a very complex group of illnesses. Review of this chapter will help all those concerned with care of the pregnant patient.
Presentation and Characteristics
Clinical Appearance
First onset may occur during any pregnancy, generally during the second or third trimester. Explosive onset in the immediate postpartum period can occur in up to 25% of cases.
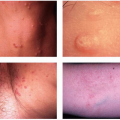
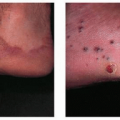
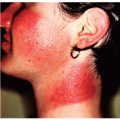
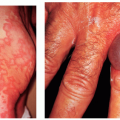
Clinical lesions vary from intensely pruritic urticarial plaques to pemphigoid-like tense blisters (Fig. 48-1). One often sees rapid evolution from the urticarial phase to clustered or arcuate tense blisters. Patients with only urticarial lesions and no progression to blisters have been reported.
Intense, relentless pruritus is invariable.
TABLE 48-1 ▪ Classification of Dermatoses of Pregnancy* | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Distribution
Onset occurs in the periumbilical area in 50% of patients, but may also first appear on the palms, soles, or extremities. Facial involvement is rare and mucosal involvement essentially nonexistent.
Course
Exacerbation at delivery occurs in approximately 75% of patients and may be dramatic.
Generally recurs during subsequent pregnancies, although “skip pregnancies” have been reported. Flares associated with menstruation or oral contraceptives are also reported.
Spontaneous resolution over weeks to months following delivery is the rule, although case reports of protracted disease are available.
There is no increased maternal risk in association with PG.
Newborns may be affected up to 10% of the time, presumably through passive transfer of the PG IgG.
There is an increased risk of premature delivery associated with PG (32% before 38 weeks, 16% before 36 weeks).
Laboratory Findings
Routine laboratory results are normal. Mild peripheral eosinophilia may occur, but is not clearly clinically relevant.
Histopathology classically shows a subepidermal blister with eosinophils. Eosinophils are uncommon in PUPPP and suggest one should at least consider PG in the differential diagnosis.
Direct immunofluorescence showing complement, with or without IgG deposited in a smooth, linear band along the dermal-epidermal junction, is the diagnostic sine qua non, occurring in essentially 100% of cases. Split specimens show staining on the epidermal fragment. Indirect immunofluorescence reveals an IgG1 capable of avid complement activation. Titers of the PG antibody are low and historically do not correlate with the extent or severity of skin involvement. Recent, more sensitive immunoblotting and enzyme-linked immunoassays (NC16a ELISA, now commercially available) may challenge that assessment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree