Cutaneous T-cell Lymphoma
Stephen J. Nervi MD
W. Clark Lambert MD, PhD
Robert A. Schwartz MD, MPH
Introduction
The diagnosis of cutaneous lymphoma mandates consideration of a large and diverse group of malignant B-cell or T-cell lymphocytes in various stages of differentiation. In this chapter we focus on skin, the primary site of cutaneous lymphoma. Historically, primary cutaneous lymphomas were thought to be of T-cell origin; cutaneous B-cell lymphomas (CBCLs) were assumed to be secondary, or a dissemination of a nodal B-cell lymphoma.With the advent of immunohistochemical and molecular genetic modalities, it has become clear that B-cell cutaneous lymphomas are, in fact, a distinct and important group of primary cutaneous lymphomas. The majority are low-grade malignancies that have a good prognosis and slow course. This chapter will focus on primary cutaneous T-cell lymphomas (CTCLs).
CTCLs are the largest group of cutaneous lymphomas, accounting for 65% to 80% of all cases. They are classified by the World Health Organization (WHO)/European Organization for Research and Treatment of Cancer (EORTC) classification (WHO-EORTC classification) as follows:
Mycosis fungoides (MF)
MF variants: Pagetoid reticulosis (localized), follicular, syringotropic, granulomatous, and granulomatous slack skin (GSS) syndrome
Sézary syndrome (SS)
CD30+ T-cell lymphoproliferative disorders of the skin
Lymphomatoid papulosis
Primary cutaneous anaplastic large cell lymphoma
Subcutaneous panniculitis-like T-cell lymphoma (SPTL)
Primary cutaneous peripheral T-cell lymphoma (PTL), unspecified
PTL subtypes:
Primary cutaneous aggressive epidermotropic CD8+ T-cell lymphoma
Cutaneous gamma/delta-positive T-cell lymphoma (CGD-TCL)
Primary cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoma
Extranodal NK/T-cell lymphoma, nasal type
Variant—Hydroa vacciniforme-like lymphoma
Adult T-cell leukemia/lymphoma (ATLL)
Angioimmunoblastic T-cell lymphoma
SAUER’S NOTES
1. Cutaneous lymphoma is the wolf in sheep’s clothing for the dermatologist. Any skin disease that does not respond to normal therapeutic intervention as would be expected, suddenly worsens in intensity or distribution, is unusually chronic, or appears to be following an unexpected course, should be suspect for lymphoma. Protean clinical manifestations of this group of diseases are the rule.
2. Can you ever biopsy the skin too frequently? I think it is very unlikely that the patient, the patient’s family, the patient’s referring physician, or the patient’s attorney will be critical of a biopsy done to confirm benign disease. For better or worse, a biopsy not done and a malignancy missed are a recipe for problems.
CTCL, most commonly evident as MF, is usually a clonal expansion of T-helper cells, less often of T suppressor/killer cells or NK cells, manifesting as a widespread and long-standing cutaneous eruption. MF is characterized by the relatively predictable and often gradual evolution of patches into plaques and tumors composed of skin-targeting malignant T cells. This progression may be gradual and the patient may outlive the disease.
Pagetoid reticulosis is a noteworthy variant of MF characterized by the presence of localized discrete cutaneous patches or plaques with an intraepidermal proliferation of neoplastic T cells. The term pagetoid reticulosis should be restricted to the localized type (Woringer-Kolopp type) and should not be used to describe the disseminated form (Ketron-Goodman type). Generalized cases should probably be classified as aggressive epidermotropic CD8+ CTCL, CGD-TCL, or tumor-stage MF.
GSS syndrome is a rare subtype of CTCL characterized by the development of folds of loose or “slack” skin in the major skin folds and, histologically, by an infiltrate of clonal T cells, with exceptionally large multinucleated giant cells sometimes showing inclusion of fragmented elastic fibers.
SS has been defined historically by the triad of erythroderma, generalized lymphadenopathy, and the presence of
neoplastic T cells (Sézary cells) in skin, lymph nodes, and peripheral blood, respectively. Others assert that the definition of SS should include one or more of the following:
neoplastic T cells (Sézary cells) in skin, lymph nodes, and peripheral blood, respectively. Others assert that the definition of SS should include one or more of the following:
An absolute Sézary cell count of least 1000/μL
Demonstration of immunophenotypical abnormalities (an expanded CD4+ T-cell population resulting in a CD4/CD8 ratio of more than 10:1; loss of any or all of the T-cell antigens CD2, CD3, CD4, CD5; or loss of both CD4 and CD5)
Demonstration of a T-cell clone in the peripheral blood by molecular or cytogenetic methods
ATLL is an aggressive T-cell neoplasm associated with human T-cell leukemia virus 1 (HTLV-1).While an indolent form involving the skin may occur, cutaneous findings are usually a manifestation of widely disseminated disease.
SPTL is a type of T-cell lymphoma characterized by the presence of primarily subcutaneous infiltrates of neoplastic T cells and macrophages, predominantly affecting the legs and often complicated by a hemophagocytic syndrome. There are at least two groups of SPTL with different histologies, phenotypes, and prognoses. Cases with an alpha/beta-positive T-cell phenotype are usually CD8+, are restricted to the subcutaneous tissue (with no dermal or epidermal involvement), and tend to run an indolent course. The SPTL designation is only used for patients with an alpha/beta-positive T-cell phenotype, whereas those with a gamma/delta T-cell phenotype are now categorized as having CGD-TCL.
Extranodal NK/T-cell lymphoma is an Epstein-Barr virus (EBV)-associated lymphoma usually with an NK cell, or, less commonly, a cytotoxic T-cell phenotype. The nasal cavity or nasopharynx is the most common site of involvement, and the skin is the second most common site. Cutaneous involvement may be primary or secondary; however, because both primary and secondary involvement are clinically aggressive and require the same type of treatment, distinction between the two cutaneous forms is largely academic.
Primary cutaneous PTL, type unspecified, encompasses those CTCLs that do not fit into any of the subtypes of CTCLs. These include the provisional entities described later, because primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma, CGD-TCL, and primary cutaneous small/medium CD4+ T-cell lymphoma are sufficiently characteristic that they can be separated as provisional entities:
Primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma, a provisional entity, is characterized by a proliferation of epidermotropic CD8+ cytotoxic T cells and aggressive clinical behavior.
CGD-TCL is composed of a clonal proliferation of mature, activated gamma/delta T cells with a cytotoxic phenotype. It may be a primary or secondary cutaneous lymphoma.
Primary cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoma is the diagnosis used when a predominance of small- to medium-sized CD4+ pleomorphic T cells are present without a history of patches and plaques typical of MF.
Pathophysiology
The primary pathophysiologic mechanisms for the development of CTCL (i.e., MF) have not been elucidated. Genetic, genotraumatic, immunologic, and environmental etiologies have all been considered. Chronic exposure to various irritants has been considered in the pathogenesis of CTCL, but evidence thus far is not conclusive. A persistent antigen that over time leads to an accumulation of mutations in oncogenes, suppressor genes, and signal-transducing genes has been suggested. One of us has proposed the thymus-bypass hypothesis that aberrant differentiation, in which T cells differentiate in the skin (rather than thymus), may be a cause.
Epidemiology
In the United States, the incidence of CTCL is approximately five cases per million people per year. It is assumed that there is a similar worldwide incidence with some possible increases among workers using machine cutting oils. Areas where HTLV-1 is endemic, such as certain Caribbean Islands, parts of South America, Central Africa, and southwest Japan have a higher incidence of ATLL. In Jamaica and selected other Caribbean Islands, childhood-infective dermatitis is viewed a marker of HTLV-1 infection. CTCL is more common in men than women with an approximate ratio of 2:1.Most patients with CTCL are middle aged or elderly. Peak incidence is during the 5th decade, although it may rarely occur in children. Children with CTCL usually have a mild course and excellent prognosis, though extension to tumor stage and death may occur.There also does not seem to be a male predominance in children with one series observing a female predominance.As CTCL in its incipient stage may present as a chronic, poorly defined dermatitis, the average duration from onset to diagnosis of CTCL is 4 to 6 years.Most cases are treated with myriad topical agents preceding biopsy that obscure histologic diagnosis.
History and Staging
Classic MF
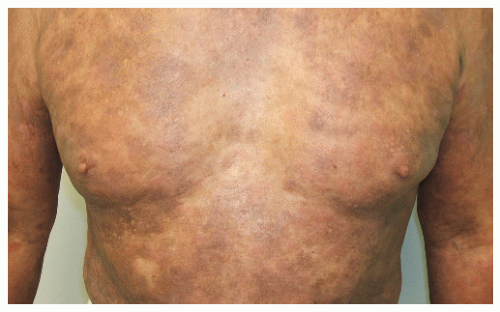
MF is divided into three stages: patch, plaque, and tumor (Figs. 31-1,31-2,31-3). The patch stage may persist for many years and is characterized by a nonspecific dermatitis usually consisting of patches most commonly centrally located on the lower trunk and buttocks. Sometimes, these patches have a thin, wrinkled quality, often with reticulated pigmentation. In this stage, pruritus is usually minimal or absent. Classic MF is usually preceded by a nonspecific indolent inflammatory process, manifesting as atopic dermatitis, nonspecific chronic dermatitis, or parapsoriasis (most commonly
large-plaque parapsoriasis), which may progress over years to decades to early plaque-stage MF. Some authorities regard large-plaque parapsoriasis as patch-stage MF. In many cases, the disease does not progress beyond this stage, and the diagnosis of MF is never confirmed. In other cases, the disease appears from the beginning as rather well-defined superficial plaques that range from 2 cm to more than 20 cm in diameter.
large-plaque parapsoriasis), which may progress over years to decades to early plaque-stage MF. Some authorities regard large-plaque parapsoriasis as patch-stage MF. In many cases, the disease does not progress beyond this stage, and the diagnosis of MF is never confirmed. In other cases, the disease appears from the beginning as rather well-defined superficial plaques that range from 2 cm to more than 20 cm in diameter.
While well-developed plaques that are clinically diagnostic for MF are usually intensely pruritic, less characteristic ones typically are not, and the development of pruritus in such lesions is a sign of progression toward MF. Many cases remain at these stages for many years or decades without further progression.
 FIGURE 31-2 ▪ Patch-stage CTCL with cigarette paper wrinkling atrophy and hyperpigmentation. Some areas are already forming plaques over the left lower back. |
Stages IA and IIA
The stage of disease determines the prognosis for most cases of CTCL, particularly MF and SS. Stage IA consists of patches and/or plaques affecting less than 10% of the total body surface without erythroderma, lymph node, or visceral involvement. Stage IB is defined by involvement of 10% or more of the total body surface.
Stages IIA and IIB
CTCL is stage IIA if there are clinically enlarged lymph nodes that histologically do not show evidence of CTCL tumor cells. If skin tumors of CTCL are present with no visceral involvement or erythroderma, the disease is in stage IIB, regardless of lymph node involvement. Either process usually takes years or even decades to develop. Tumors once formed are prone to ulceration.
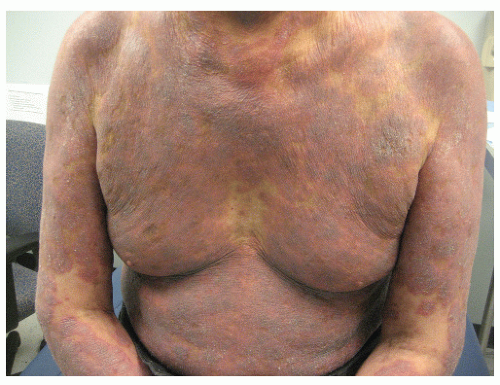
Stages III, IVA, and IVB
The disease is classified as stage III if erythroderma is present but neither circulating lymphoma cells nor, histologically proven involvement of lymph nodes or viscera is present, regardless of whether lymphadenopathy is noted. If lymph nodes are histologically involved with the lymphomatous process, the disease is in stage IVA.Visceral involvement with histologically proven lymphoma denotes stage IVB.
D’emblee MF
MF usually progresses sequentially through its stages. However, rarely the development of apparent MF tumors may occur without preceding patches or plaques.Most, if not all, such cases may represent primary cutaneous CD30+ pleomorphic, medium or large cell T-cell lymphomas.
Transformation of MF
MF in any stage may suddenly accelerate or become much more aggressive, progressing rapidly to more advanced stages. This is associated with the histologic appearance of
large atypical cells. Often, these are CD30+, and the process is termed large cell transformation.
large atypical cells. Often, these are CD30+, and the process is termed large cell transformation.
TABLE 31-1 ▪ Staging of CTCL | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree