The Asian facelift requires an adaptation of current techniques to achieve a desired aesthetic outcome. Cultural differences and differences in anthropomorphologic features alter a patient’s vision of beauty and youthfulness. Rejuvenation of the aging Asian face mandates a set of strategies, including understanding cultural aspects of Asian patients, anatomy of Asian patients, and appropriate techniques based on these cultural and anatomic considerations. For stable application and results, the surgeon must understand surgical facial anatomy. If performed properly, facelifts can improve facial balance and can yield aesthetically more appealing results. The deep plane facelift technique presented is well suited for Asian patients.
Key points
- •
Specific cultural and anthropomorphologic differences require a different approach to restore facial youthfulness and attractiveness.
- •
Knowledge of anatomic structures of the face and neck is essential to understanding surgical procedures and to achieving better results.
- •
The deep plane facelift technique presented in this article is well suited for face and neck rejuvenation of Asian patients.
Aging signs appear on the face and neck due to the natural aging process, facial expressions in daily life, effects of gravity, and exposure to the sun. As people get older, the appearance and shape of the face are altered, leading to a sagging appearance of the cheeks, excess skin along the jawline and prominent jowls, sagging skin and excess fat in the neck, and decreased skin elasticity and texture. Therefore, a proper rejuvenation procedure can be chosen based on the causes.
Facelift surgery rejuvenates the middle and lower thirds of the face and upper neck. The procedure is individualized to a patient’s needs, and the plastic surgeon tailors techniques accordingly. Various techniques have been introduced for facelifts and neck lifts, and they are differentiated and compared by their different dissection planes. Modern facelift surgery was initiated by Skoog, who elevated a cervicofacial flap deep to the platysma and the superficial fascia of the face. Anatomic descriptions of the superficial musculoaponeurotic system (SMAS), retaining ligaments, and danger zones further enhanced understanding of the intricacies of facial anatomy. The current classification of facelift categories includes the subcutaneous lift, SMAS manipulation, deep plane and composite lift, , short scar and minimal invasive technique, and any combination of these. The 2 most common current facelift techniques are the deep plane rhytidectomy and SMAS manipulation. There are a limited number of studies objectively comparing the 2 techniques.
The deep plane facelift utilizes a plane of dissection below the SMAS and platysma of the face and neck, allowing for the direct lysis of key facial retaining ligaments and the mobilization of superficial soft tissue. , This is important to support the thicker and heavier tissues of the Asian face to create a more rejuvenated appearance and one that will last longer. The deep plane approach also allows access to the buccal fat pads (BFPs) of the cheeks, which are larger in the Asian face, so that they can be reduced.
The Asian face can be quite different from the white face in many respects. Some of the unique characteristics of the Asian face, versus those of white individuals, to consider during an Asian facelift include a wider and flatter face; more prominent malar bone and mandibular angle , ; weaker bone structure, especially in the lower region of the face; thicker and heavier soft tissues that cause more sagging in the lower face; and more prominent, droopy BFPs. Therefore, the chief problem is tissue drooping while having fewer wrinkles on their face. Due to their relatively thick skin, the weight of their tissue is considerably more than in other groups, and performing facelift surgery is more difficult.
Many Western plastic surgeons emphasize the importance of midcheek lifts. Vertical vector deep plane rhytidectomy provides significant long-term augmentation of volume in the midface. For several reasons, the midcheek lift in Asians is less important than for whites. Lifted midcheek tissue tends to come back down because it is difficult to support the thicker and heavier skin of Asians using only suture suspensions. During recovery, patients complain that their cheekbones appear more prominent and swelling lasts longer because of the elevated thick tissue. Lambros described that changes in the volume of cheek fat, either loss or gain, rather than ptosis account for an aged appearance. The craniofacial skeleton undergoes many changes as individuals mature. Retrusion of the lower maxilla has been observed in older patients compared with younger cohorts. Therefore, in Asians, the midcheek region should be approached in a different way from that in whites. If a midcheek lift is required, volume augmentation in this region should be considered rather than a vertical lift. Many surgeons started adopting fat injection as part of their strategy to replace lost volume. Fat grafting can be used successfully to offset the apparent width of the Asian face by placing fat along the anterior jawline and upper cheek to make the lower cheek and outer jawline appear less heavy.
Anatomy
Knowledge of anatomic structures of the face and neck is essential to understanding surgical procedures, achieving better results, and avoiding injury to important structures, including sensory and motor nerves. The soft tissues of the face are arranged concentrically into 5 basic layers that are bound together by a system of facial retaining ligaments : (1) the skin; (2) subcutaneous fat; (3) SMAS; (4) loose areolar tissue that includes retaining ligaments, space, and deep facial fat; and (5) periosteum and deep fascia. The subcutaneous layer has different thicknesses based on the location and patient. The third layer is the SMAS layer, and all of the facial muscle motor nerves are deep to this plane. Layer 4 is the layer that undergoes the most change, consisting of alternating spaces and ligaments.
Superficial Musculoaponeurotic System
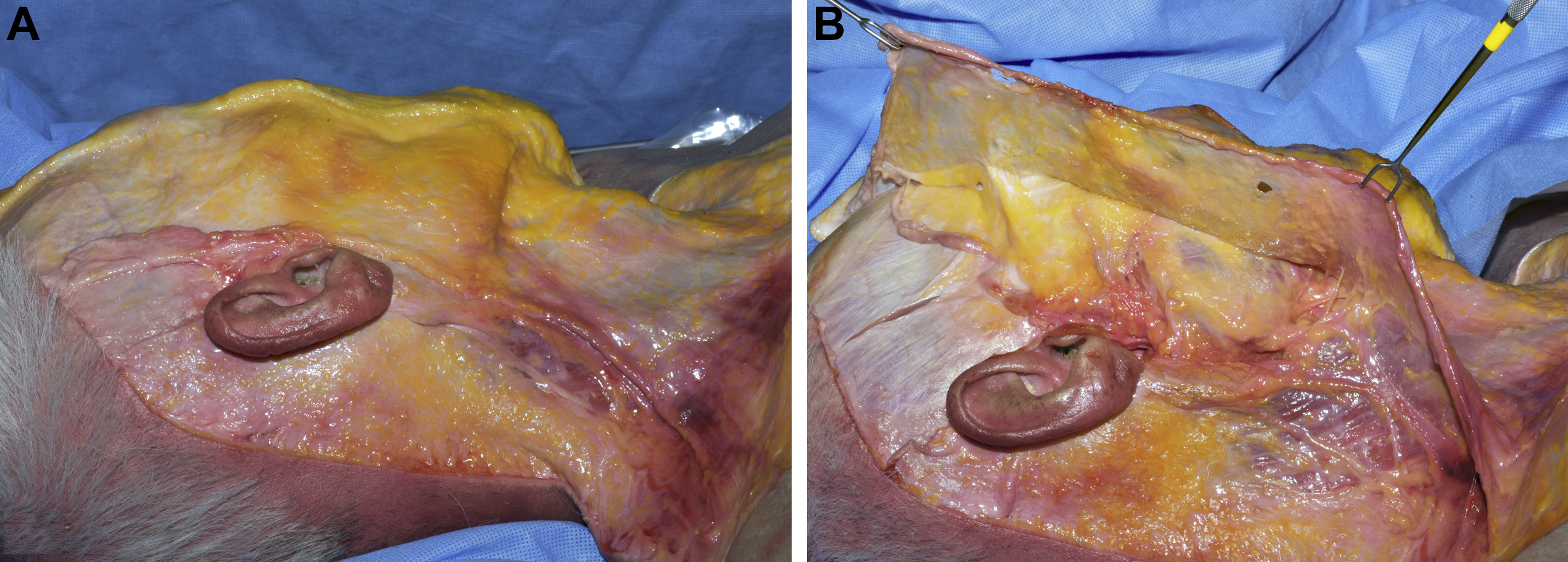
The SMAS is a well-defined portion of the superficial facial fascia that divides the deep and superficial adipose tissue of the face and forms a continuous sheath through the face and neck, and its thickness varies by patient and region of the face. The fibromuscular layer of the SMAS integrates with the superficial temporal fascia and frontalis muscle superiorly and with the platysma muscle inferiorly ( Fig. 1 A). The SMAS acts as a central tendon for the coordinated muscular contraction of the face and provides the functional role of movement for expression. The SMAS plays a vital role in the facelift procedure, and surgical maneuvering and tightening of the SMAS allow for facial rejuvenation (see Fig. 1 B).
Retaining Ligament
The retaining ligaments of the face are important in understanding concepts of facial aging and rejuvenation. These are fibrous attachments that fix the superficial layers of the face to the underlying deeper tissues to support the facial soft tissue in their normal anatomic position, thereby resisting gravitational change. Retaining ligaments of the face serve a dual purpose as they relate to facelift surgery. The ligaments act as the entryway to the midface and also serve a sentinel role with regard to peripheral facial nerve branches.
Furnas was the first to describe the anatomy of the retaining ligaments of the face. Their superficial extensions form subcutaneous septa that separate facial fat compartments. Their main significance relates to their surgical release in order to achieve the desired aesthetic outcome. When performing facial aesthetic surgery, plastic surgeons should choose a plane of dissection, release the appropriate ligaments depending on the desired aesthetic goals, and avoid nerve injury by using the ligaments as anatomic landmarks.
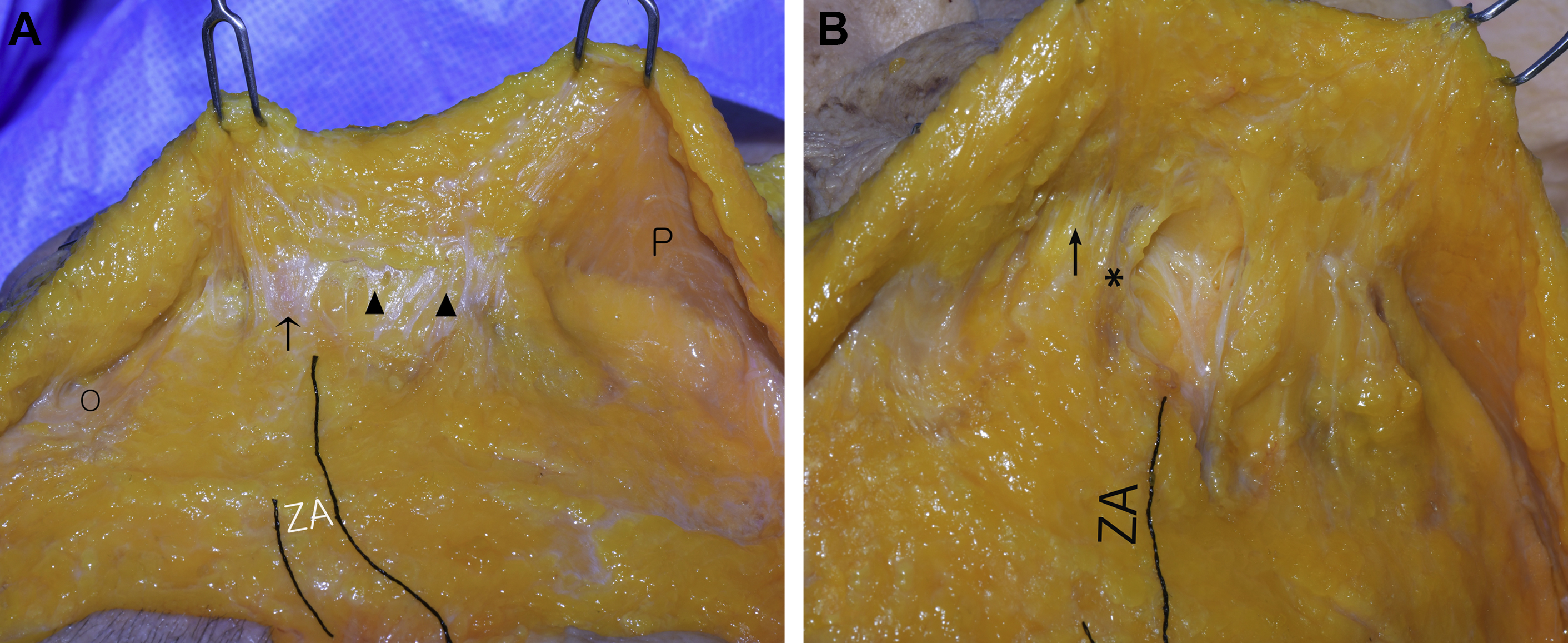
Descriptions of the retaining ligaments are variable in the literature, and different interpretations of anatomy, several classifications, locations, and nomenclature systems have been proposed. Despite the variation in published descriptions, the zygomatic retaining ligament (ZRL) occupies a predictable anatomic location given its relationship to the body and arch of the zygoma ( Fig. 3 A). Furnas described the zygomatic ligaments as stout fibers that originate at or near the inferior border of the anterior zygomatic arch, behind the insertion of the zygomaticus minor muscle, and insert in the skin serving as an anchoring point. In Mendelson and colleagues’ description, zygomatic ligaments start just lateral to the zygomaticus major muscle, where they identified the location of the strongest ligament, and continue medially across the origins of the zygomaticus major and minor and levator labii superioris. Alghoul and colleagues showed the ZRLs originating along the entire length of the zygomatic arch extending onto the malar body. During the release of the major zygomatic ligaments, the zygomatic and buccal rami of the facial nerve are found caudal to the zygomatic ligaments, because it is here that these nerve branches pass from deep fascia to an immediate sub-SMAS plane.
The masseteric retaining ligament (MRL), on the other hand, is less predictable and varied in location given that they are condensations of the deep fascia. The mean vertical distance between the main ZRL and upper MRL was 11 mm ( Fig. 2 ). The MRL arises from the masseteric fascia over the masseter muscle. Their relationship to the muscle is controversial. Although some anatomic studies have shown the ligaments arising along the anterior border of the masseter, others have shown them to arise 1 cm to 2 cm posterior to the anterior border and even from the middle portion of the muscle. The MRL is an important landmark for the zygomatic and buccal facial branches (see Fig. 3 B).

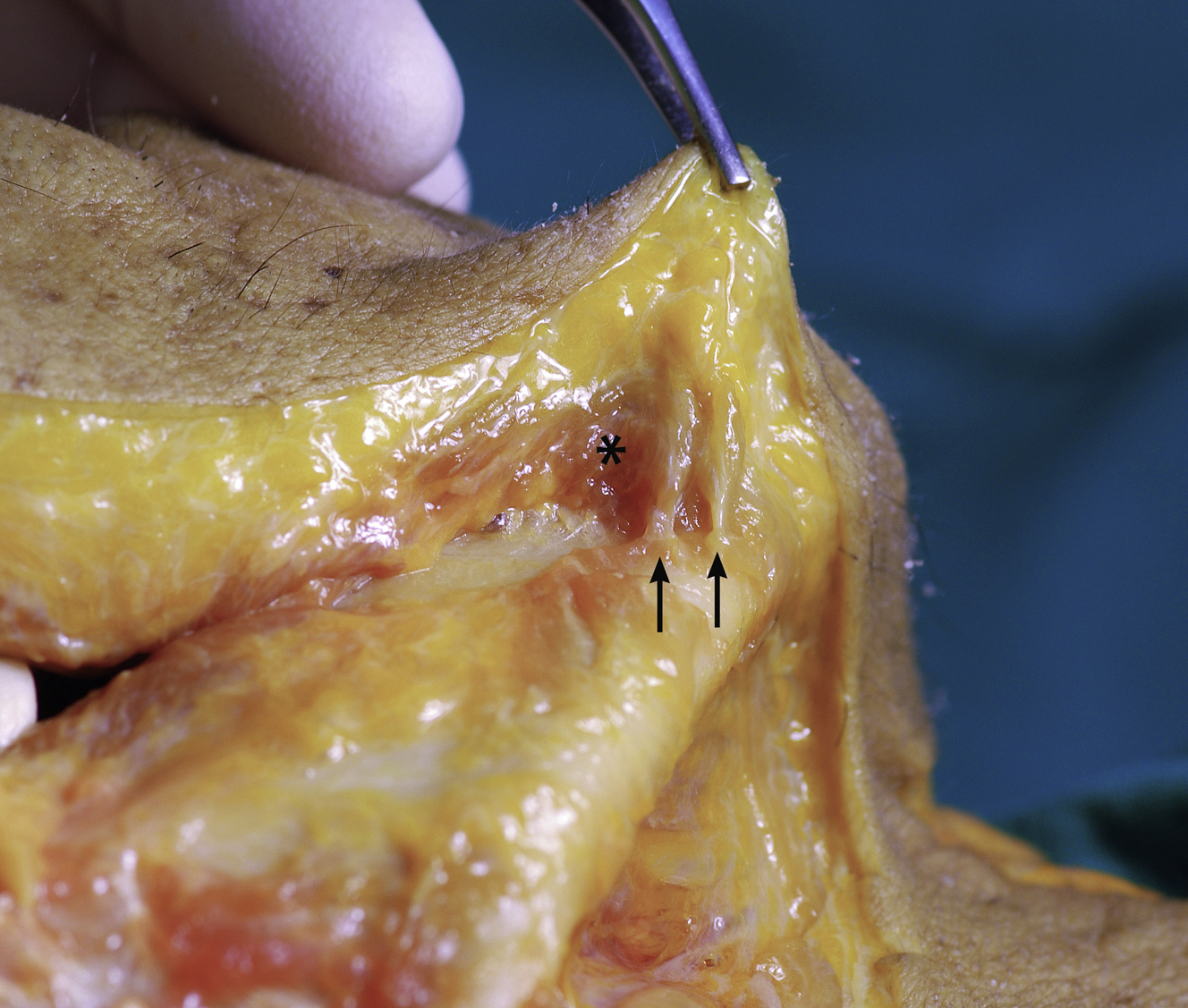
The mandibular osteocutaneous ligaments usually is a very stout band or bands that originate from the periosteum of the mandible inferior to the mental foramen at approximately the lateral border of the origin of the depressor anguli oris muscle ( Fig. 4 ). These ligaments fix this muscle and its investing fascia and continue to the dermis by a condensation of fibrous septae in the superficial fat layer. The terminal branch always is cranial to this ligament, with a distance of approximately 10 mm.
Buccal Fat Pad
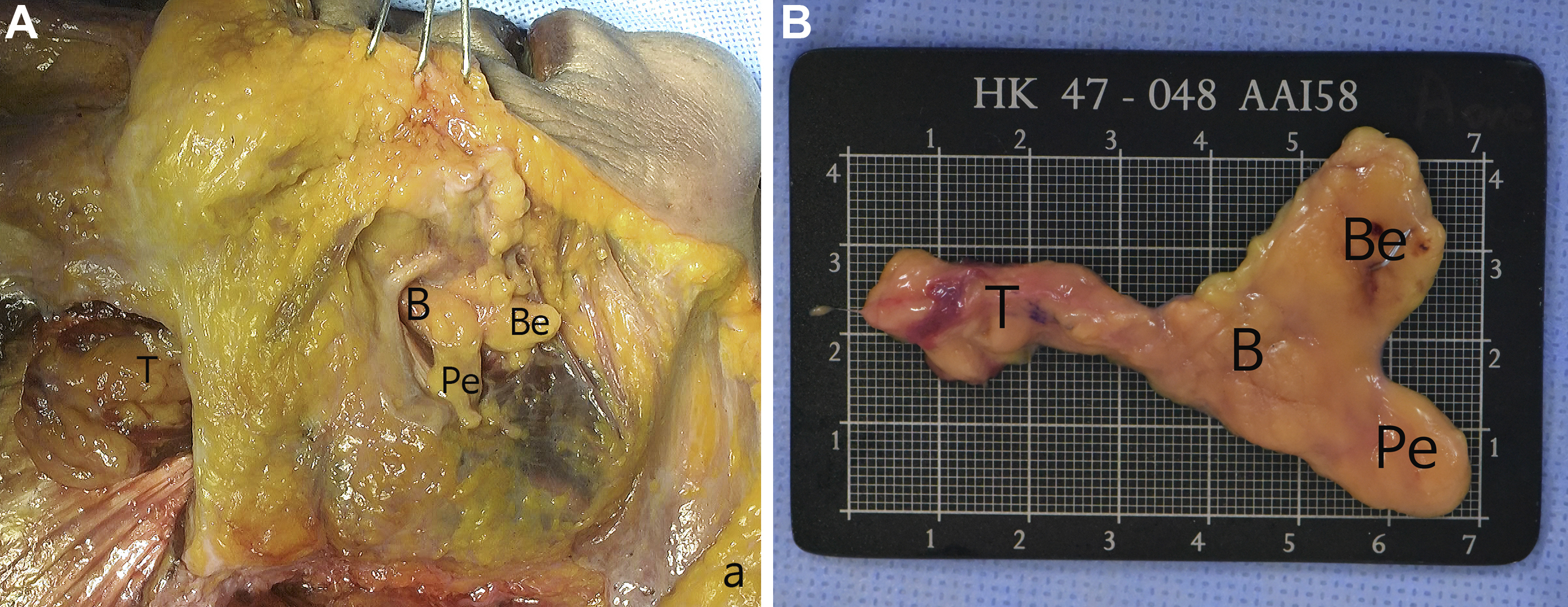
The BFP that Bichat described in 1802 is an important structure that contributes to cheek and facial contour. The BFP consists of a main body and 4 extensions: buccal, pterygoid, superficial, and deep temporal. The buccal extension is the most superficial segment of the fat pad and imparts fullness to the cheek ( Fig. 5 ). More than half of the BFP mass is the body and the buccal extension together. The ptotic lower portion of the buccal extension may contribute to jowl formation. The BFP is an important anatomic structure in relation to the masticatory muscle, facial nerve, and parotid duct. The zygomatic and buccal branches of the facial nerve lie superficial to the buccal extension. The parotid duct passes through the entire lateral surface of the BFP or penetrates it.
Jowls
The jowls and labiomandibular folds are classic signs of aging. These generally are areas of concern for the appearance of many men and women as they age. Correction of the jowls and labiomental folds are 2 of the most essential elements for a successful facelift. The jowl is the combination of the fat compartment in the lower face sliding downwards and weakening of the facial ligaments, including mandibular ligament and septum, causing a loss of definition in the jawline, chin, and neck area ( Fig. 6 ).

Facial Nerve
The facial nerve has a complex pattern, and there is considerable variability among patients. The incidence of injury to the facial nerve during a standard rhytidectomy has been reported in 2% of patients. All terminal branches of the facial nerve run below the SMAS. The protection provided by the SMAS is variable, and the temporal branches are the least protected. The course of the temporal branch has been described in detail in the literature. One of the most widely used clinical estimates for the course of frontotemporal branch of the facial nerve is the Pitanguy line, defined as a line drawn from a point 0.5 cm inferior to the tragus to a point 1.5 cm superior and lateral to the eyebrow. The Pitanguy line is not accurate to estimate the course and depth of the frontal branch, but it is simple to understand the course of the frontal branch and is close to the anterior limit of the danger zone.
Two plastic surgeons’ facial dissections demonstrated that the frontal branch travels within the innominate fascia, a fibrofatty layer deep to the SMAS, as it crosses the zygomatic arch into the temporal region. Agarwal and colleagues showed that the frontal branches are located consistently within the innominate fascia, a fibrofatty layer deep to the SMAS and superficial temporal fascia ( Fig. 7 ). Trussler and colleagues showed that the frontal branch is protected by a deep layer of the parotid temporal fascia, which is separate from the SMAS as it traverses the zygomatic arch. Division of the SMAS above the arch in a high-SMAS facelift is safe when using the technique described in that study.
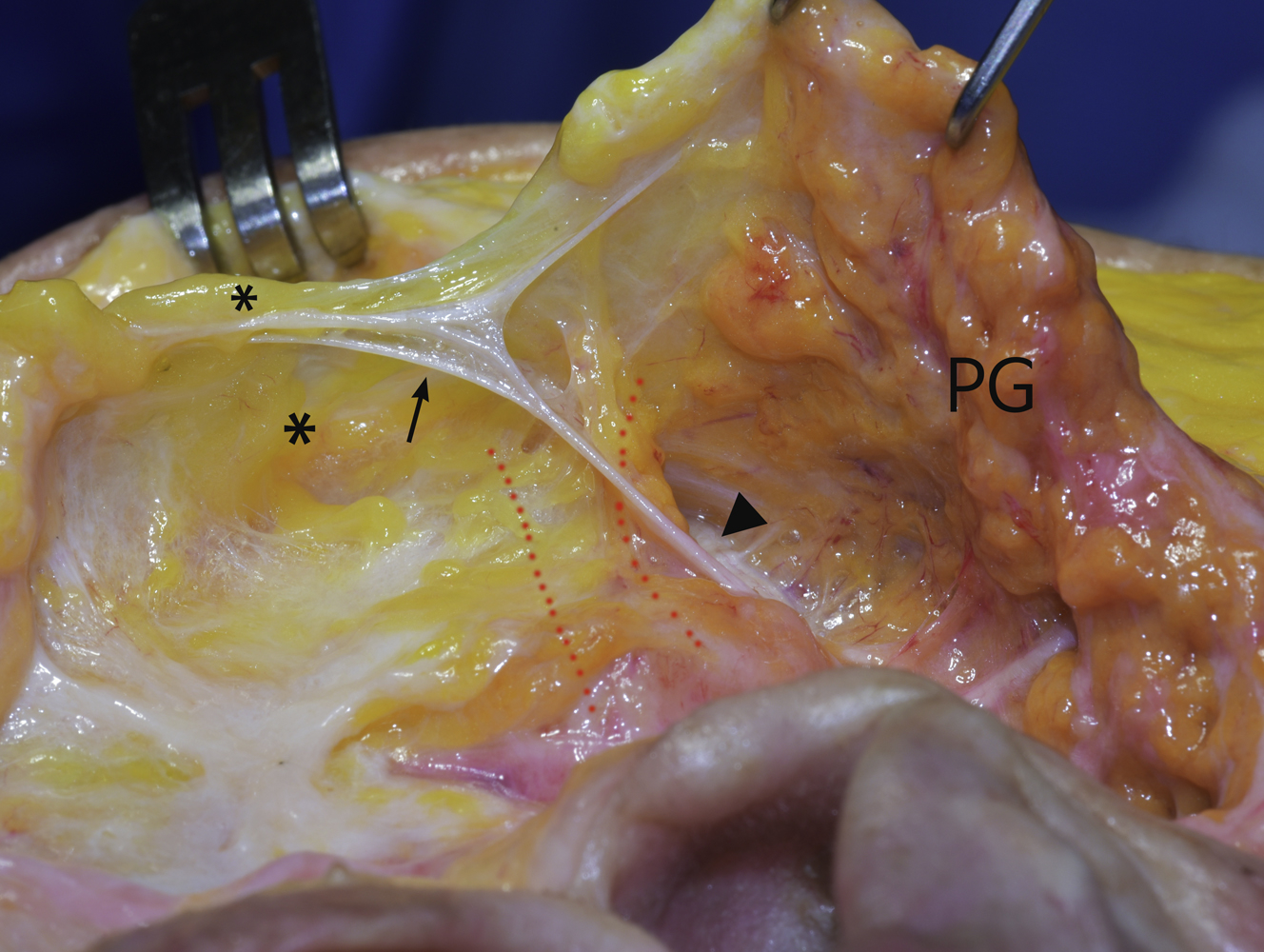
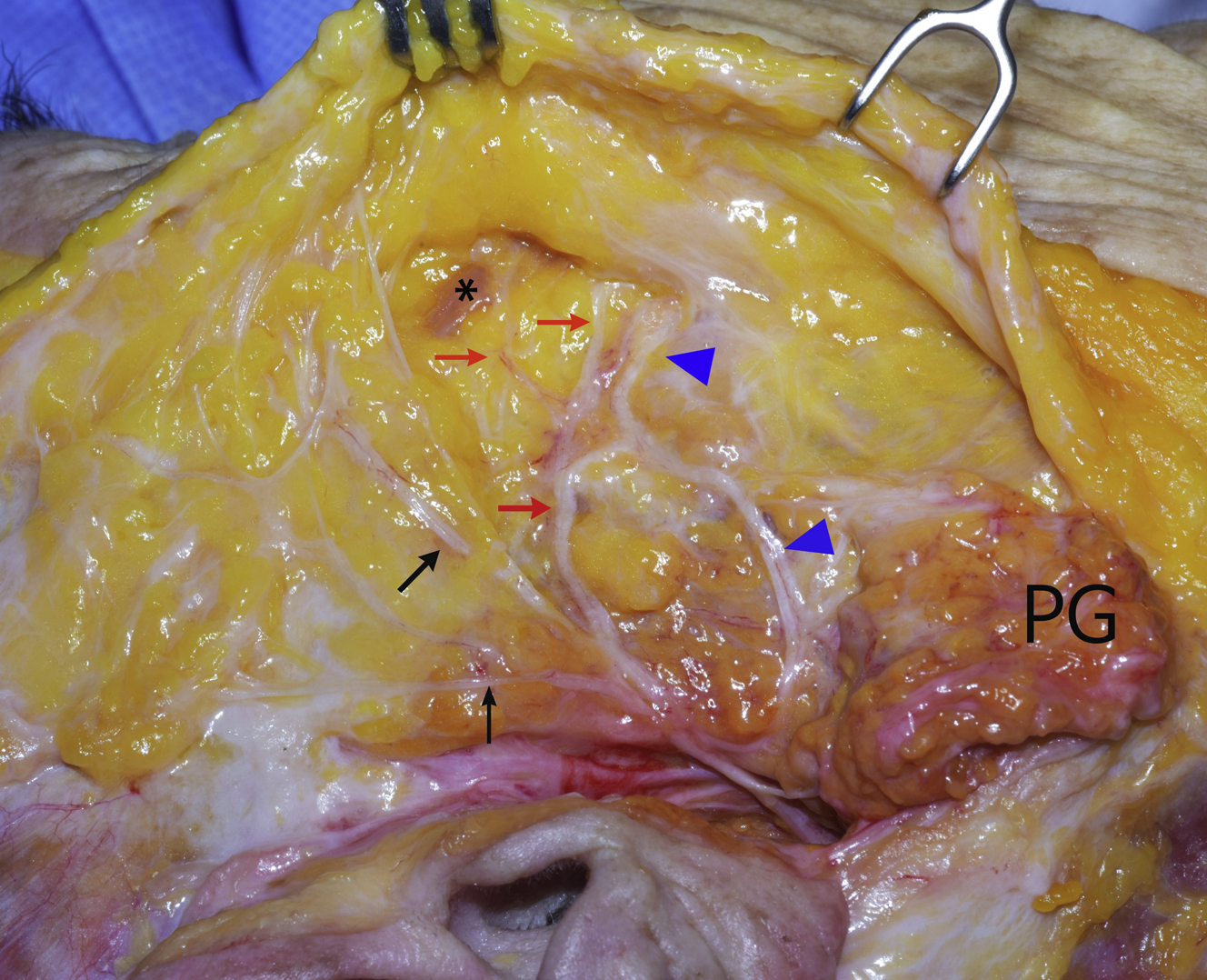
The zygomatic and buccal branches emerge from the parotid gland and run over the masseter muscle under the parotid-masseteric fascia ( Fig. 8 .). The exact point where they pierce the deep fascia is variable but is in the vicinity of the anterior border of the masseter. The ZRL and MRL can aid in identification of these nerve branches. The upper zygomatic subbranch passes between the major zygomatic cutaneous ligament and upper masseteric cutaneous ligament, deep to the deep fascia and under the upper third of the zygomaticus major muscle. The area 1 cm below the zygomaticus major muscle, therefore, has been labeled a “sub-SMAS danger zone.” The lower zygomatic subbranch runs immediately inferior to the upper MRL in a more superficial plane than the upper branch. , , The buccal branch crosses through the lower masseteric ligament. The buccal ramus is thought to be the most commonly injured facial nerve branch during facelift surgery, but the clinical effect seldom is noted owing to rich arborizations and abundant interconnections.