1 Overview of Facial Tissue Anatomy
Abstract
The key to safety in surgical dissection of the face is an accurate understanding of soft tissue anatomy. While two-dimensional branching patterns of the facial nerve are variable, the plane of the facial nerve is constant within the architecture of the facial soft tissue. Recognition of the plane of surgical dissection and its relationship to the plane of the facial nerve provides the surgeon with the ability to provide safe and consistent outcomes in both aesthetic and reconstructive facial procedures.
The primary focus of this textbook is to assist physicians operating within the face to improve their understanding of the nuances of facial anatomy, increasing both consistency in result and patient safety. Understanding facial soft-tissue anatomy is pertinent to both reconstructive and aesthetic surgery, and a three-dimensional comprehension of the architectural arrangement of facial soft tissue is essential when dissecting facial flaps for reconstructive purposes or performing procedures to expose the craniofacial skeleton, and more specifically when performing aesthetic surgery procedures.
Preventing facial nerve injury is the most important aspect of both safety and preserving function when performing facial procedures. The critical element to avoid motor branch injury is an accurate understanding of the three-dimensional architecture of facial soft tissue.
While much has been written about facial nerve anatomy, many investigations have focused on two-dimensional branching patterns of the facial nerve. Unfortunately, two-dimensional facial nerve anatomy is not particularly relevant when dissecting within the face, as there is a great deal of variation in terms of branching patterns among patients as well as variations in branching patterns between the right and left side of the cheek. The key to avoiding facial nerve injury is to understand the three-dimensional architecture of the soft tissue planes of the face, as well as recognizing the plane of dissection in relation to the plane of the facial nerve. THINK THREE DIMENSIONALLY.
1.1 The Architectural Arrangement of Facial Soft Tissue
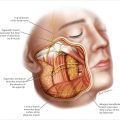
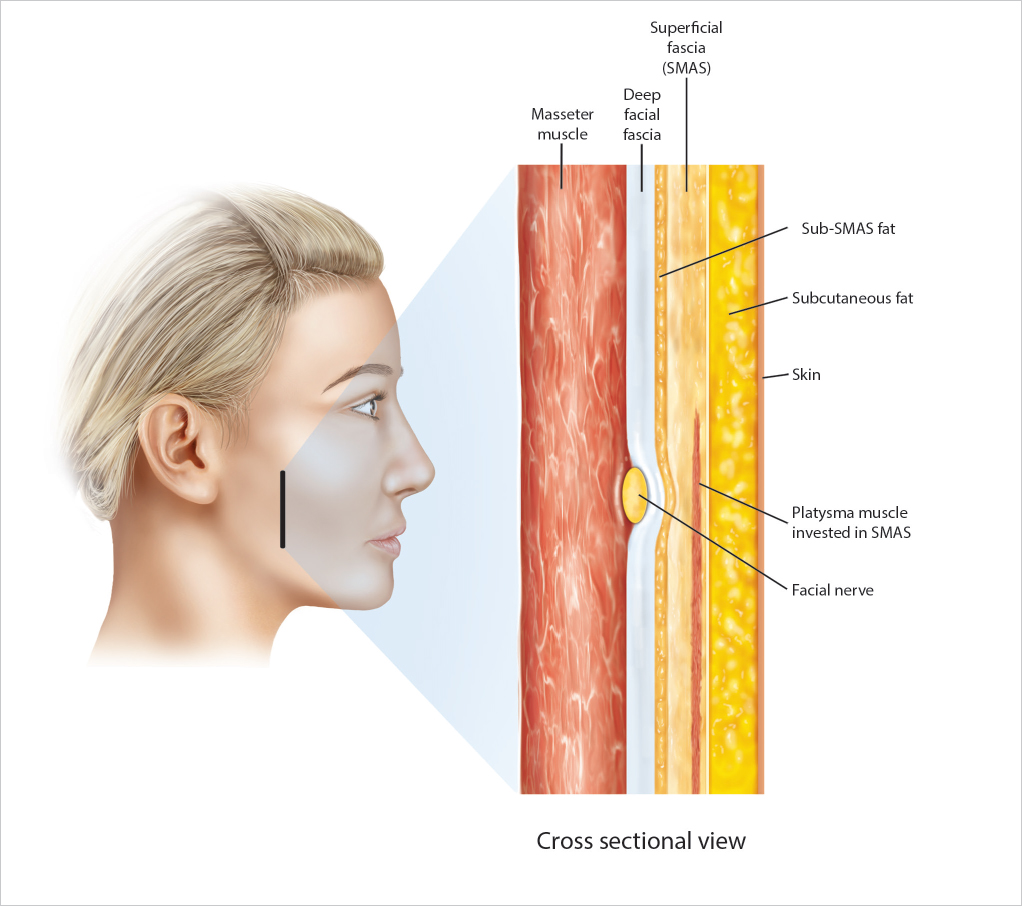
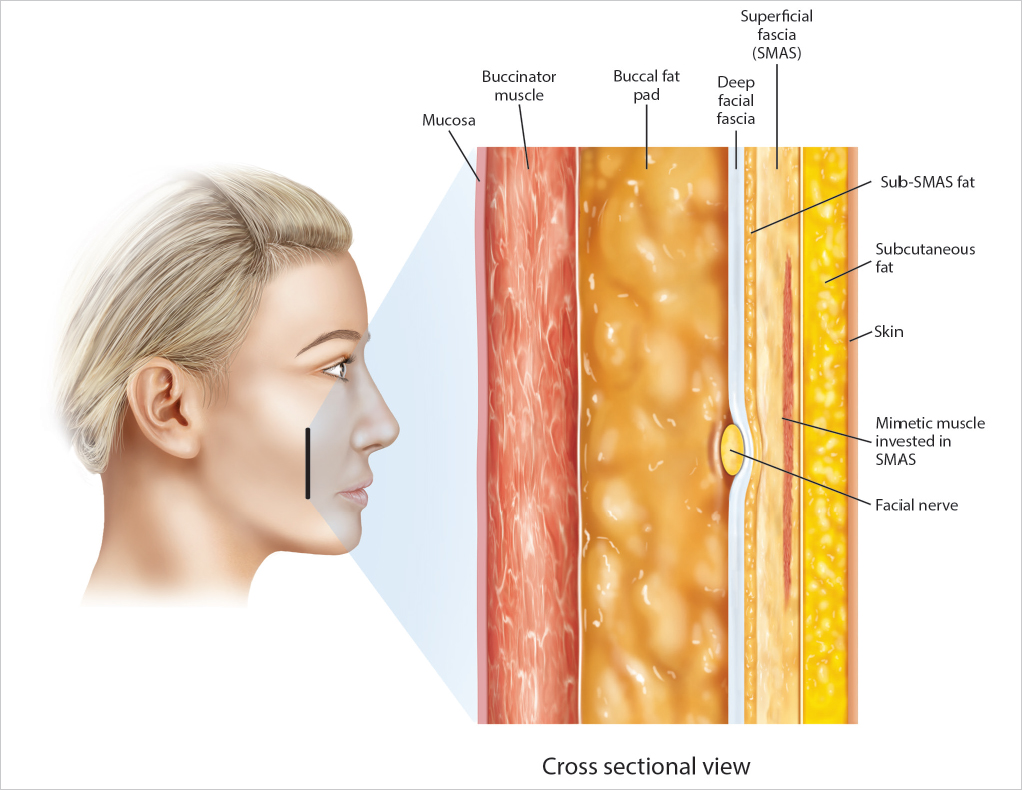
Facial soft tissue is arranged in a series of concentric layers, similar to the concentric layers of an onion.
1.1.1 The Layers of Facial Soft Tissue from Superficial to Deep
Skin
Compartmentalized subcutaneous fat
Superficial facial fascia (also termed SMAS; these terms will be used interchangeably)
Mimetic muscles (superficial muscles invested by the SMAS)
Subsmas fat
Deep facial fascia (also regionally known as parotid capsule, masseteric fascia, or deep temportal fascia)
The plane of the facial nerve, parotid duct, and buccal fat pad (▶ Fig. 1.1a,b ).
1.1.2 The Plane of the Facial Nerve
While there is a good deal of variation in terms of two-dimensional facial nerve branching patterns, the plane of the facial nerve in relation to the other fascia layers of the face is anatomically constant.
The critical step to avoid facial nerve injury is to accurately identify the plane of dissection as it is performed. If dissection is carried out either superficially or deeply to the plane of the facial nerve, motor branch injury will be prevented.
While the plane of the facial nerve is constant from patient to patient, both the thickness and the appearance of each anatomic layer varies significantly, such that the nuance of plane identification becomes the key to safe dissection.
Just as skin thickness varies from patient to patient, so does the thickness of the underlying subcutaneous fat and SMAS. Similarly, the presence or absence of sub-SMAS fat, and the thickness of the underlying glistening deep facial fascia will appear different in many patients.
Typically, these layers are better defined and thicker in younger patients than in in older patients. Similarly, reoperative surgery or reconstructive procedures following trauma can distort the appearance of fascial planes. Nonetheless, the architectural arrangement remains constant and is present in all patients, and the key to safety for the surgeon is to recognize what plane is being dissected when operating within the face. (see Video 1.1).
1.1.3 Layers of Facial Soft Tissue
Skin
The skin’s thickness and vascularity vary from patient to patient.
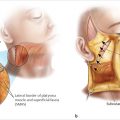
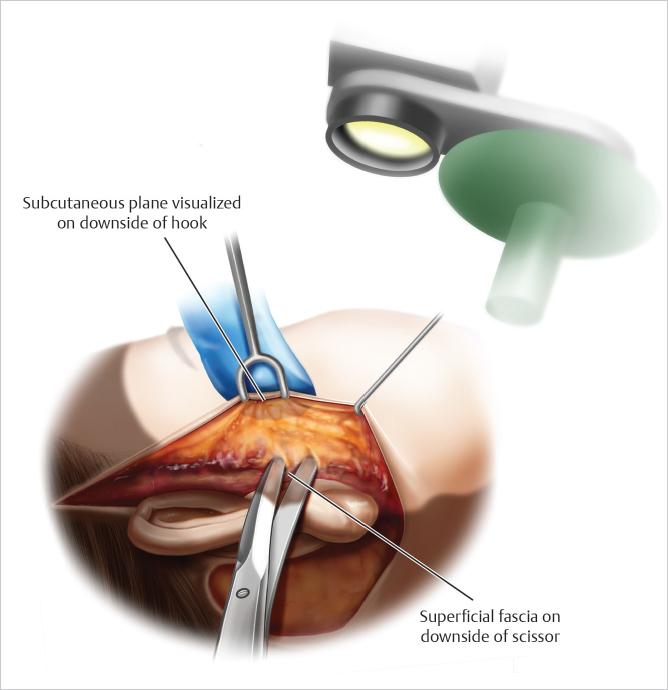
When performing a facelift or raising a cervicofacial flap for facial reconstruction, the key to safety is to perform the dissection within the underlying subcutaneous fat, superficial to the SMAS.
The use of transillumination to define the interface between the subcutaneous fat and the superficial fascia is helpful in defining the correct plane of dissection (▶ Fig. 1.2 , Video 1.2).
Subcutaneous Fat
The plane of the subcutaneous fat is the dissection plane typically utilized in both reconstructive and aesthetic facial procedures and is anatomically situated as an interposition between the skin dissection and the underlying superficial fascia (SMAS).
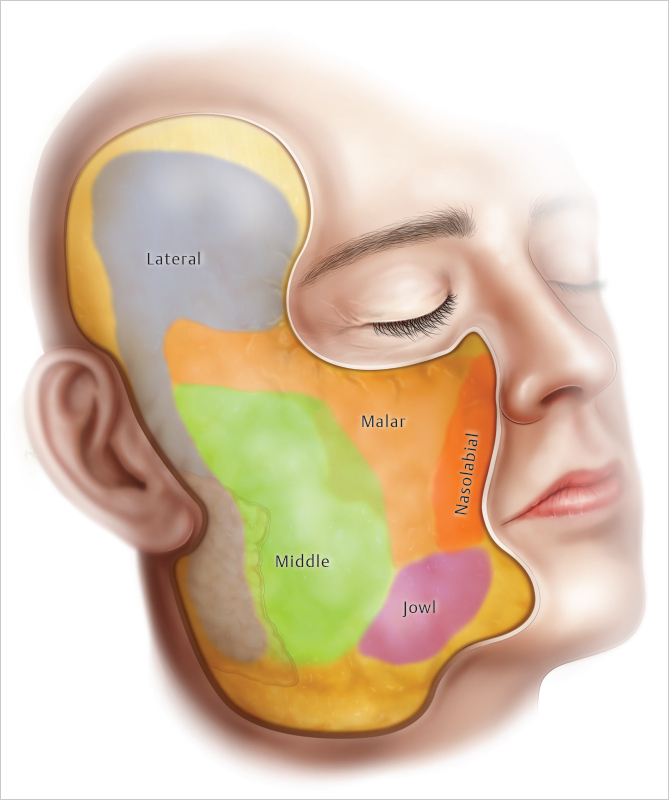
Facial subcutaneous fat is not a homogenous structure, but is separated into a series of separate “facial fat compartments.”
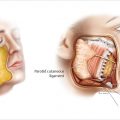
The fibrous septa, which separate the subcutaneous fat into compartments, represent the distal ramifications of the retaining ligaments, which travel from deep fixed structures such as the parotid gland to penetrate the SMAS and inset into the overlying skin.
Vascular perforators similarly transit from deep to superficial adjacent to the retaining ligaments, such that as dissection proceeds from one compartment to an adjoining facial fat compartment, bleeding from these perforators is noted.
Both the thickness and fascial consistency of the fat within each compartment varies as the cheek is dissected, from laterally in the preauricular region more anteriorly toward the nasolabial fold.
The lateral compartment, in the preauricular region, tends to be thin, dense, and vascular, while the fat within the middle compartment tends to be thick, fluffy, avascular, and easy to dissect.
Transiting from the middle to the malar compartment, zygomatic ligaments and perforators from the transverse facial artery are encountered such that dissection along the lateral malar eminence tends to be both fibrous and bloody.
Each facial fat compartment has its own tendency toward deflation, with the lateral compartments showing evidence of deflation in patients in the 40 to 50 year age group, while malar deflation tends to occur a decade later. The anatomic nature of deflation (which is compartment-specific) explains why facial deflation tends to occur regionally, rather than homogenously across the cheek in facial aging (See Chapter 2 on Facial Fat Compartments) (▶ Fig. 1.3 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree