Spirochetal Infections
John C. Hall MD
Two spirochetal diseases are discussed in this chapter: syphilis and Lyme disease.
Syphilis
When Gordon C. Sauer was stationed at the West Virginia State Rapid Treatment Center, from 1946 to 1948, the average for patient admittance was 30 a day. Approximately one third of these patients had infectious syphilis. In 1949, the center was closed because of the patient census. Today, the incidence of reported syphilis has risen again to alarming heights. Many patients with acquired immunodeficiency syndrome (AIDS) also have syphilis. Because of this resurgence, it is imperative that all physicians have a basic understanding of this polymorphous disease.
Cutaneous lesions of syphilis occur in all three stages of the disease. Under what circumstances will the present-day physician be called on to diagnose, evaluate, or manage a patient with syphilis?
1. The cutaneous manifestations, such as a penile lesion or a rash that could be secondary syphilis, may bring a patient into the office.
2. A positive blood test found on a premarital examination or as part of a routine physical examination may be the reason for a patient’s visit to the dermatologist.
3. Syphilis may be seen in conjunction with AIDS. The problem becomes complicated because the serologic test for syphilis (STS) may not be positive in patients with AIDS and routine antibiotic dosage regimens may be ineffective.
4. Cardiac, central nervous system, or other organ disease may be a reason for a patient to consult a physician.
To manage these patients properly, a thorough knowledge of the natural untreated course of the disease is essential.
SAUER’S NOTES
1. To diagnose syphilis, the physician must have a high index of suspicion for it.
2. Syphilis is the great imitator and can mimic many other conditions.
3. Serologic tests for syphilis in AIDS may be falsely (−).
Primary Syphilis
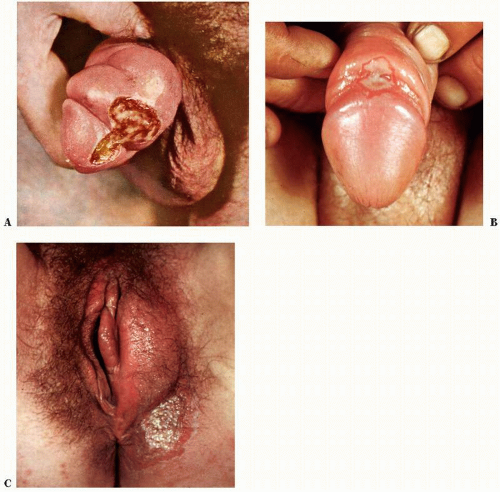
The first stage of acquired syphilis usually develops within 2 to 6 weeks (average 3 weeks) after exposure. The primary chancre most commonly occurs on the genitalia (Figs. 22-1 and 22-2), but extragenital chancres are not rare and are often misdiagnosed. Without treatment the chancre heals within 1 to 4 weeks but is dependent on the location, the amount of secondary infection, and host resistance.
The blood STS may be negative in the early days of the chancre but eventually becomes positive. The spirochete, Treponema pallidum, is readily found with darkfield examination. This test is of limited value since there are few people with the expertise to interpret the test reliably. A cerebrospinal fluid examination by darkfield during the primary stage reveals invasion of the spirochete in approximately 25% of cases.
Clinically, the chancre may vary in appearance from a single small erosion to multiple indurated ulcers of the genitalia. It is usually painless and with an indurated border (“hard chancre”). Primary syphilis commonly goes unnoticed in the female patient due to its intravaginal or rectal location. Men who have sex with men (MSM) may also have hidden rectal chancres. Bilateral or unilateral regional lymphadenopathy is common. Malaise and fever may also be present.
Early Latent Stage
Latency, manifested by positive serologic findings and no other subjective or objective evidence of syphilis, may occur between the primary and secondary stages.
Secondary Syphilis
Early secondary lesions may develop before the primary chancre has healed or after latency of a few weeks (Figs. 22-3,22-4,22-5). Late secondary lesions are more rare and usually are seen after the early secondary lesions have healed. Both types of secondary lesions contain the spirochete T. pallidum, which can be easily seen with the darkfield microscope. The STS is positive (an exception is in some patients with AIDS), and approximately 30% of the cases have abnormal cerebrospinal fluid findings.
Clinically, the early secondary rash can consist of macular, papular, pustular, squamous, or eroded lesions or combinations of any of these lesions. Papulosquamous is most common with oval lesions and fine dry adherent scale. This can easily be confused with pityriasis rosea. Palm and sole involvement is characteristic and there is no herald patch. Secondary syphilis can be generalized or localized to the palms and soles, genital area, or mucous membranes. A “moth-eaten” scalp alopecia may develop in the late secondary stage.
Condylomata lata is the name applied to the flat, moist, warty lesions teeming with spirochetes found in the groin and the axillae (Figs. 22-4 and 22-5). Mucous patches are white elevated verrucous skin lesions usually on the oral mucous membranes.
The late secondary lesions are nodular, squamous, and ulcerative and are distinguished from the tertiary lesions only by the time interval after the onset of the infection and by the finding of the spirochete in superficial smears of serum from the lesions. Annular and semiannular configurations of late secondary lesions are common.
Generalized lymphadenopathy, malaise, fever, and arthralgias occur in many patients with secondary syphilis.
Early Latent Stage
Following the secondary stage, many patients with untreated syphilis have only a positive STS. After 4 years of infection, the patient enters the late latent stage.
Late Latent Stage
This time span of 4 years arbitrarily divides the early infectious stages from the later noninfectious stages, which may or may not develop.
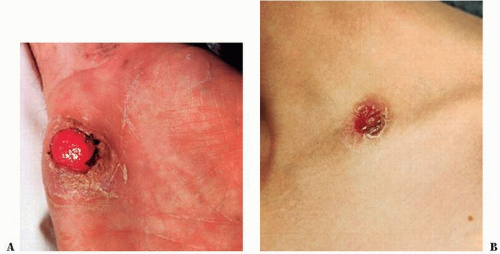
Tertiary Syphilis
This late stage is manifested by subjective or objective involvement of any of the organs of the body, including the skin (Figs. 22-6 and 22-7; see also Fig. 3-1A). Tertiary changes may be precocious but most often develop 5 to 20 years after the onset of the primary stage. Clinically, the skin lesions are characterized by nodular and gummatous ulcerations. Solitary multiple annular and nodular lesions are common. Subjective complaints are rare unless considerable secondary bacterial infection is present in a gumma. Scarring is inevitable in the majority of the tertiary skin lesions. Larger texts should be consulted for the late changes seen in the central nervous system, the cardiovascular system, the bones, the eyes, and the viscera. Approximately 15% of the patients who acquire syphilis and receive no treatment will die of the disease.
Late Latent Stage
Another latent period may occur after natural healing of some types of benign tertiary syphilis.
Congenital Syphilis
Congenital syphilis is acquired in utero from an infectious mother (Fig. 22-8). The STS required of pregnant women by most states has lowered the incidence of this unfortunate disease. Stillbirths are not uncommon from mothers who are untreated. After the birth of a live infected child, the mortality rate depends on the duration of the infection, the natural host resistance, and the rapidity of initiating treatment. Early and late lesions are seen in these children, similar to those found in the adult cases of acquired syphilis. Blistering can occur.
Laboratory Findings
Darkfield Examination
The etiologic agent, T. pallidum, can be found in the serum from the primary or secondary lesions. However, a darkfield microscope is necessary, and very few physicians’ offices or laboratories have this instrument. A considerable amount of experience is necessary to distinguish T. pallidum from other Treponema species.
Serologic Test for Syphilis
The STS is simple, readily available, and has several modifications. The rapid plasma reagin (RPR) test and the Venereal Disease Research Laboratories (VDRL) flocculation test are used most commonly. Treponemal tests such as the fluorescent treponemal antibody absorption (FTA-ABS) test and modifications are more difficult to perform in the laboratory and therefore are used primarily when the RPR and VDRL tests are “reactive.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree