Summary
Laser treatment of vascular and pigmented lesions can be quite challenging. As with other procedures it is important to select optimal techniques and technology to optimize the outcome and minimize the risks. This chapter reviews laser and light sources for the treatment of vascular and pigmented lesions. Device and treatment parameter selection is reviewed as well as desired treatment endpoints and description of tissue effects that might indicate excessive energy and increased risk of complication. Tips on safely maximizing treatment outcomes while avoiding complications are offered as are tips on managing complications.
11 Vascular and Pigment Laser and Light Sources
11.1 Vascular and Pigment Laser and Light Sources
Laser and light treatment of vascular and pigmented lesions has evolved to a level of safety and specificity that enables physicians to treat a variety of lesions and help numerous patients with their areas of concern.
11.1.1 Laser Treatment of Vascular Lesions
Lasers that treat vascular targets include the KTP (532 nm), pulsed dye laser (585 and 595 nm), as well as longer pulsed lasers including alexandrite (755 nm), diode (800–980 nm), and the Nd: YAG (1064 nm) lasers that emit pulses in the millisecond range. Correct choice of laser or light device as well as settings of the device are critical to achieving success in the treatment of vascular lesions.
11.1.2 Choice of Device—Wavelength and Pulse Duration
In the treatment of telangiectasia, size of the vessel is an important factor in device selection. The principle of selective photothermolysis, for these lesions, refers to site-specific, laser-induced heat injury of pigmented or vascular targets in the skin. The utilization of selective photothermolysis requires proper wavelength selection, pulse duration, and energy or fluence. An additional consideration, particularly in the treatment of vascular lesions, is spot size of the laser pulse. Larger spot sizes penetrate deeper so are better suited to deeper and larger blood vessels and small spot sizes penetrate less deeply and are best utilized in the treatment of small, superficially located vessels.
Selection of pulse duration is based on vessel size. Choosing the correct pulse duration is key to both appropriate selective heating and effective destruction of the blood vessel target as well as avoiding side effects and injury. Too short a pulse duration can lead to rupture of the blood vessel due to very rapid heating and side effect of purpura. Think of a water-filled balloon popping. This is a photoacoustic/cavitation reaction, and, in the case of linear blood vessels, repair mechanisms have been shown to lead to recovery and revascularization of the vessels; however, in the treatment of some vascular lesions, such as cherry angiomas and vascular birthmarks, this can be a desired endpoint. Too long a pulse duration can lead to spreading of heat beyond the target to surrounding tissue and can lead to nonspecific heat-induced injury in the surrounding structures—dermis and epidermis. Think of a heating coil turned on to spread heat to melt ice or snow—peripheral injury to the ice and snow. The ideal heating time is long enough to adequately heat the target without violent rupture while still slightly less than the time that allows spread of heat to adjacent tissue. This ideal heating time and confinement of laser-induced heat to the target without transfer or spread to surrounding tissues can be defined by thermal relaxation time or TRT. 1 TRT is the time required for cooling of the laser target to 50% of the temperature achieved immediately after laser impact. The TRT can be estimated by using this calculation: TRT in seconds is approximately equal to the square of the diameter of the target in millimeters—a 0.1-mm blood vessel would be expected to have a TRT of about 10 ms. Larger blood vessels require longer pulse durations and smaller blood vessels are best targeted with shorter pulse durations.
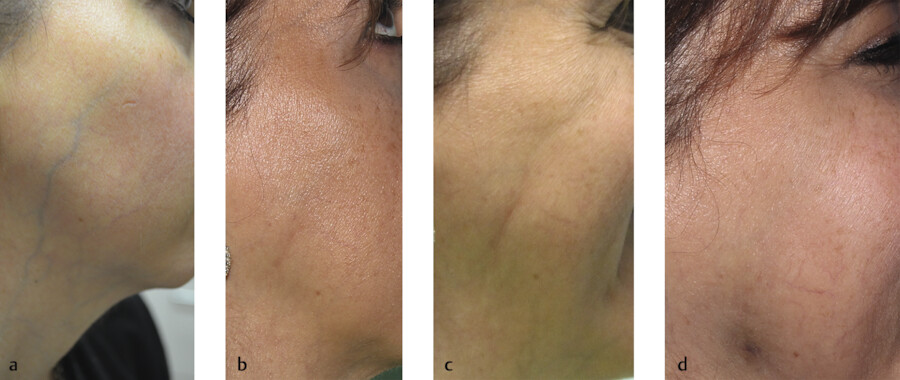
Proper selection of wavelength is also critical to safe and effective treatment of vascular lesions. Both patient skin color and size and depth of the vascular target must be taken into consideration. Superficial lesions are best targeted by shorter wavelengths whereas longer wavelengths penetrate deeper into the skin and are better suited for deeper blood vessels. Caution must be exercised when treating larger blood vessels. As described earlier, the heating of a large vein can act as a conduit of that heat to the surrounding tissue and damage the surrounding tissue. Blisters to frank ulceration can occur over the blood vessel with atrophic scarring—a particularly vulnerable area is the nasal ala (Fig. 11.1a, b). In addition, damage to tissue can appear later as evidenced by atrophy over the treated vein with no obvious immediate injury (blistering or ulceration) at the time of the laser treatment (Fig. 11.2). To avoid this complication, carefully select a pulse duration that most closely matches the vessel size and slowly increase energy while observing for vessel reaction after each laser pulse—vessel darkening or vessel shrinkage. At the same time careful cooling of the skin is critical to protect the skin overlying the blood vessels. We often employ measures above what is offered within the laser device itself (contact or cryogen cooling) by applying handheld ice packs to the area immediately before and after each laser pulse. Forced cool air can be used for additional cooling of the skin but cannot be used during firing of the laser pulse if cryogen cooling is deployed as there is potential for the air to blow the cryogen off target.

11.1.3 Enhancing Outcomes in the Treatment of Vascular Lesions
It is crucial to recognize clinical endpoint in treating vascular lesions. The goal is vascular damage without damage to surrounding structures. When treating linear vessels, the vessel may disappear immediately, or you may see spasm or coagulation of the vessel which is seen clinically as shrinkage of the vessel and darkening of the color of the vessel (Video 11.1). When treating larger blood vessels or larger blue veins, particularly on face or neck areas, careful observation for blood vessel response without too violent or rapid a response and without any skin contraction over the vessel is crucial. This slight retraction of the skin may mean there is too much heat transfer to the skin and potential for skin damage. Rupture of the vessel can be seen also as purpura but this is not always a desired endpoint.
When treating diffuse redness such as seen in rosacea, each laser pulse should generate a fleeting darkening of the treated area, or transient purpura, that does not result in persistent purpura. Typically, test pulses are done at initial treatment settings looking for this fleeting or transient purpura change with several seconds of waiting to be sure the change does not persist to true purpura (Video 11.2, and Fig. 11.3). If no transient purpura is seen, the energy can be increased in small increments until transient but not persistent purpura is observed (Video 11.2). Several methods of enhancing outcomes from laser treatment of vascular targets have been proposed and are commonly utilized by many practitioners particularly when treating conditions that are typically difficult to treat with a laser. These conditions include the erythema associated with rosacea—flushing and the so called “background” erythema or redness which gives a “ground glass” red appearance to the skin that does not seem to blanch with pressure and can be seen almost as a skin color on close exam between every pore or pilosebaceous unit (Fig. 11.4). Several methods can be used to enhance laser outcomes. One is to increase the target by inducing flushing or vessel dilation by heating the skin using heating pads or wraps (we use a microwaveable heating pad called Bed Buddy®) or air-activated hand warmers (Hothands®). 2 Another is to increase blood flow with measures as simple as having the patient rest with head below knees immediately prior to laser treatment. Application of topical niacin to induce vascular flushing/dilation has been shown to increase efficacy of pulsed dye laser in the treatment of vascular flushing and rosacea. 3 , 4 Another method using the 595-nm pulsed dye laser is called pulse stacking and refers to applying closely timed, sub-purpuric consecutive pulses to the target to increase vascular clearance 5 (Video 11.3).


Occasionally, a large vascular lesion or bleb such as a large cherry angioma, nodules within a port wine stain, venous lake, or pyogenic granuloma will require treatment. Pulse stacking with the 595-nm laser can be effective, and the excess heat delivered to the nodular lesion can help shrink or contract the nodule (Fig. 11.5a, b). A long wavelength laser such as 755-nm or 1,064-nm laser can be utilized to treat larger vascular lesions, but caution must be exercised as it is easy to overheat these large targets and damage surrounding skin leading to ulceration, poor wound healing, and scarring. Another option is to compress the vascular bleb with a glass slide and pulse the laser over the slide. Additional cooling may be necessary as the glass slide may block the cooling associated with the laser (cryogen or contact cooling). My preferred treatment protocol is to start with the 595-nm pulsed dye laser with pulse stacking initially and then with glass slide compression if needed and move to a longer wavelength laser only if the 595 nm does not produce the desired endpoint. When using a longer wavelength laser on these larger vascular lesions, always start with a moderate pulse duration (10–30 ms) and lower energy and gradually increase energy until a desired endpoint is achieved. Cool target before and in between pulses and do not rapidly stack or repeat pulses.

Summary of Steps to Success in Laser Treatment of Vascular Lesions
Choose correct laser/wavelength:
Shorter wavelengths for smaller, superficial vessels and diffuse erythema (532 nm KTP, IPL, 585/595 PDL).
Longer wavelengths for larger, deeper vessels (755-nm long-pulsed alexandrite, 800- to 980-nm diode, 1,064-nm long-pulsed Nd:YAG).
Longer wavelengths (1,064 nm) are safer for darker skin types. Caution in darker skin types (Type V, VI) using wavelengths shorter than 1,064.
Match pulse duration to vessel size:
Small veins respond best to shorter pulse durations—typically 6 to 20 ms. Be careful not to completely compress very fine telangiectasia or diffusely red areas as you will lose your target.
Larger veins require longer pulse durations. Blood vessels 0.2 mm up to 1 mm have TRTs of 20 ms up to 300 ms. Caution with larger vessels—it is best to be slightly less than the TRT of the vessel to prevent heat transfer and damage to surrounding structures.
Utilize skin cooling:
Epidermal cooling is critical, particularly when treating larger blood vessels.
Pre- and postcooling can improve safety and provide complication-free outcomes when treating larger vascular targets. Caution if forced cool air is used for additional skin cooling when using cryogen cooling paired with laser pulse.
Recognize treatment endpoints: Key target responses indicate appropriate treatment: transient or flashing purpura, light purpura (a very light purple color), vessel spasm or contraction, immediate disappearance of vessel, evidence of intravascular thrombosis in vein/vessel, or rupture of blood vessel.
Don’t miss warning signs: Be immediately aware of danger signs of excessive heat or transfer of heat: loud “pop” noise with laser impact, graying or whitening of skin, excessive edema or frank blistering, dark purpura (dark gray or black color), or excessive pain.
Exercise caution in vulnerable areas: Reduce laser energy by 10 to 20% on thin or fragile skin areas such as neck, chest, forehead, nose, and ankle areas.
Improve outcomes by enhancing target: Increase blood flow via heat, gravity, or niacin-induced flushing, consider pulse stacking, utilize a glass slide to compress raised lesions.
11.2 Laser Treatment of Pigmented Lesions
A variety of lasers can be utilized for the treatment of pigmented lesions. Melanin and tattoo ink are the common target chromophores when treating pigmented lesions, but the location in the skin (epidermal, dermal, mixed) varies as does the size of the chromophore. In addition, the degree of competing chromophores—skin type and tanning—can play a significant role in laser removal of pigment.
11.2.1 Nanosecond and Picosecond Lasers (1,064 nm, 755 nm, 532 nm)
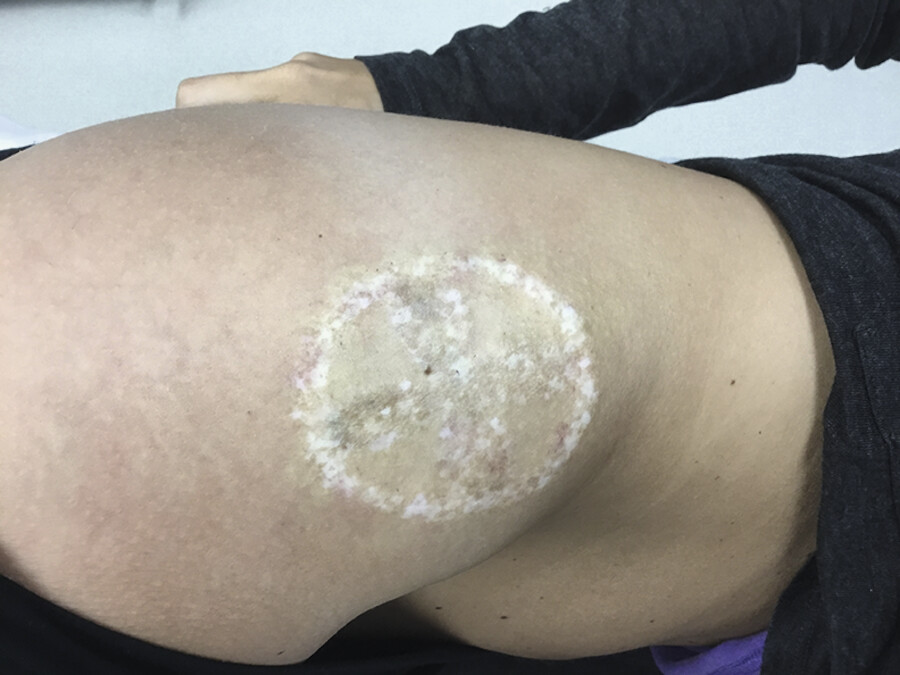
Nanosecond pulse durations such as provided with Q-switched lasers can ideally treat many superficial pigmented lesions such as solar lentigines, ephilides or freckles, and café au macules. Deeper lesions—such as Nevus of Ota and Ito, and tattoos—can also be targeted with the Q-switched lasers but longer wavelengths to reach a deep target are more ideal (755 nm and 1,064 nm). The target chromophore in these lesions is the melanosome whose size appropriately matches the nanosecond pulse duration in Q-switched lasers. 6 Tattoo pigment particles are smaller than melanosomes, and the nanosecond pulse as well as ultrashort picosecond pulse produces a photomechanical or photoacoustic rupture, not selective heating via photothermolysis. When using the Q-switched laser for pigment removal, the visual endpoint of treatment is mild-to-moderate whitening of the skin overlying the target without lifting, blistering, or ablation/splatter of the skin. A mild snapping sound is typically heard on laser impact; however, a loud snap or pop-on laser impact may indicate too high an energy (Video 11.4). Excessive tissue or target reaction or excessive absorption of laser energy in the upper layers of skin can lead to hypopigmentation and scarring (Fig. 11.6). When treating lentigines, a shortcoming of the 532-nm laser might be mild purpura or petechiae as hemoglobin is also a target at this wavelength. In addition, when numerous lentigines are present, treatment with a small spot size, Q-switched laser can be a time-consuming task as each lesion must be treated individually. One technique that has been effective for treatment of certain pigmented lesions including melasma, postinflammatory hyperpigmentation, and café au lait macules is low fluence Q-switched 1,064-nm laser treatments directed over the entire lesion for a series of treatments spaced 2 to 4 weeks apart (Video 11.5). 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








