Seborrheic Dermatitis, Acne, and Rosacea
John C. Hall MD
Seborrhea dermatitis, acne, and rosacea all tend to occur in patients with oily skin. They occur in areas where the oil glands are the largest and most plentiful such as the scalp, face, central chest, and upper back. Response to therapy is better with substances that remove oil and are worsened by substances that are oily. Many therapies are beneficial for all three diseases.
Seborrheic Dermatitis
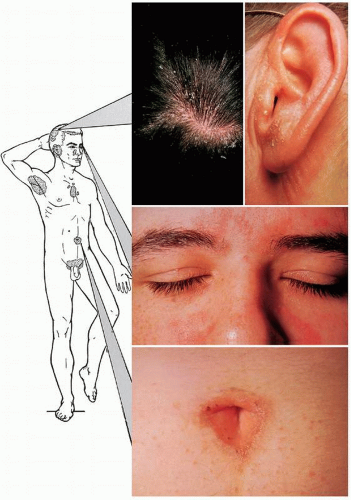
Seborrheic dermatitis, in our opinion, is a synonym for dandruff. The former is the more severe manifestation of this dermatosis. Seborrheic dermatitis is exceedingly common on the scalp, but less common on the other areas of predilection: ears, face, sternal area, axillae, intergluteal area, and pubic area (Figs. 13-1 and 13-2). It occurs as part of the acne seborrhea complex. Dandruff is spoken of as oily or dry, but it is all basically oily. If dandruff scales are pressed between two pieces of tissue paper, an oily residue is expressed, leaving a mark on the tissue.
Certain misconceptions that have arisen concerning this common dermatosis needs to be corrected. Seborrheic dermatitis cannot be cured, but remissions for varying amounts of time do occur naturally or as the result of treatment. Seborrheic dermatitis does not cause permanent hair loss or baldness unless it becomes grossly infected. Seborrheic dermatitis is not contagious. The cause is unknown, but an important etiologic factor is the yeast Pityrosporum ovale.
Seborrheic dermatitis in AIDS patients can be widespread and recalcitrant to therapy. It can be severe and is common in patients with Parkinson’s disease.
Presentation and Characteristics
Primary Lesions
Redness and scaling appear in varying degrees. The scale is of the greasy type (see Fig. 13-1).
Secondary Lesions
Rarely seen are excoriations from severe itching and secondary bacterial infection. Lichen simplex chronicus can follow a chronic itching and scratching habit.
Course
Exacerbations and remissions are common, depending on the season, treatment, and age and general health of the patient. A true cure is impossible.
Seasonal Incidence
This condition is worse in colder weather, presumably due to lack of summer sunlight.
Age Incidence
Seborrhea occurs in infants (called cradle cap), but usually disappears by the age of 6 months (Fig. 13-3). It may recur again at puberty.
Differential Diagnosis
Scalp Lesions
Psoriasis: Sharply defined, silvery-white, dry, scaly patches; typical psoriasis lesions on the elbows, knees, nails, or elsewhere (see Chapter 14).
Lichen simplex chronicus: Usually a single patch on the posterior scalp area or around the ears; intense itching; excoriation; thickening of the skin (see Chapter 8).
Tinea capitis: Usually occurs in a child; broken-off hairs, with or without pustular reaction; some types fluoresce under Wood’s light; positive culture and potassium hydroxide mount (see Chapter 25).
Atopic eczema: Usually occurs in infants (where it spares the diaper area) or children; diffuse dry scaliness; eczema also on face, arms, and legs; atopic personal and family history (see Chapter 8).
Face Lesions
Systemic lupus erythematosus: Faint, reddish, slightly scaly, “butterfly” eruption, aggravated by sunlight, with fever, malaise, arthritis, Raynaud’s and positive antinuclear antibody test (see Chapter 37).
Chronic discoid lupus erythematosus: Sharply defined, red, scaly, atrophic areas with large follicular openings with keratotic plugs, resistant to local therapy, often leaves scars (see Chapter 37).
Body Lesions
Tinea corporis (see Chapter 25)
Psoriasis (see Chapter 14)
Pityriasis rosea (see Chapter 15)
Tinea versicolor (see Chapter 15)
Treatment
Case Example: A young man presents with recurrent red, scaly lesions at the border of the scalp and forehead and diffuse, mild, whitish scaling throughout the scalp.
 FIGURE 13-2 ▪ Seborrheic dermatitis behind the ear and at the border of the scalp. (Courtesy of Smith Kline & French Laboratories.) |
1. Management of cases of dandruff must include explaining the disease and stating that it is not contagious, that there is no true cure, that it does not cause baldness, and that there are seasonal variations. Therapy can be very effective, but only for keeping the dandruff under control.
2. With this information in mind, tell the patient that shampooing offers the best management. There are several shampoos available, and the patient may have to experiment to find the most suitable one. The following types can be suggested: Selenium sulfide 2 ½% suspension (Selsun; Head and Shoulders Intensive Treatment, which is available over the counter; Selseb prescription shampoo, which also contains urea and zinc pyrithione) 120.0.
Sig: Shampoo as frequently as necessary to alleviate itching and scaling. Use no other soap. Refill prescription p.r.n.
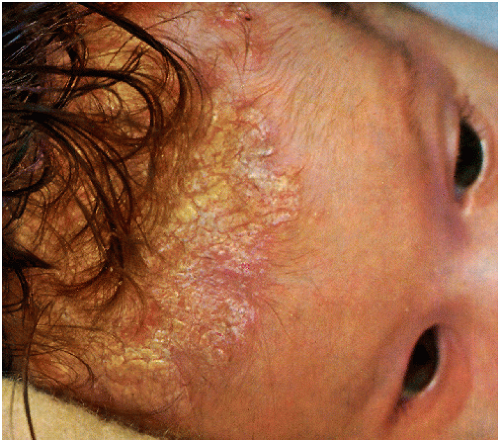 FIGURE 13-3 ▪ Seborrheic dermatitis of infancy. This is one of the causes of “cradle cap.” (Courtesy of Smith Kline & French Laboratories.) |
Additional shampoos:
Tar shampoos, such as Ionil T, Tarsum, Reme-T, Pentrax, X Seb T, T-Gel, and T-Sal (a salicylic acid shampoo).
Zinc pyrithione shampoos, such as Zincon, Head & Shoulders, and DHS Zinc.
Ketoconazole (Nizoral) shampoo (over the counter) and as a higher percentage it is available as a prescription, Loprox shampoo, Capex shampoo (contains fluocinolone, by prescription) or Clobex shampoo (contains clobetasol and should be used Monday, Wednesday, and Friday by prescription).
Sig: Shampoo as frequently as necessary to keep scaling and itching to a minimum.
3. Triamcinolone (Kenalog) spray, 63 mL.
Sig: Apply sparingly to scalp at night. Squirt the spray through a plastic tube that is supplied.
Comment: A spray is less messy on the scalp than a corticosteroid solution, but solutions are available.
4. A low-potency corticosteroid cream 15.0.
Sig: Apply b.i.d. locally to body lesions. A good combination is 1% HC and 2% sulfur in Acid Mantle cream. Generic Vytone cream is another safe therapy.
5. Ketoconazole 2% cream 15.0 (available over the counter).
Sig: Apply b.i.d. on scalp or body lesions.
Comment: This is a corticosteroid-sparing agent.
Ciclopirox (Loprox shampoo) and sodium sulfacetamide (Ovace) wash, used as a shampoo, may also be used.
6. 5% LCD (liquor carbonis detergens), 3% salicylic acid in betamethasone solution is another example to apply twice a day to the scalp.
7. Fluocinolone 0.01% solution is popular because it is mixed in propylene glycol, which kills yeast.
8. Pimecrolimus (Elidel) cream and tacrolimus ointment 0.1% and 0.3% (Protopic) can be used in a thin coat b.i.d. without topical corticosteroid side effects.
9. Foam preparations such as sodium sulfacetamide foam (Ovace), betamethasone valerate (Luxiq) foam, or clobetasol (Olux) foam may be beneficial b.i.d. and after shampooing. Avoid overuse of triamcinolone and especially clobetasol.
SAUER’S NOTES
1. Do not prescribe a fluorinated corticosteroid cream for long-term use on the face or in intertriginous areas.
2. Reiterate that there is no cure for seborrheic dermatitis; long-term management is necessary.
3. Reassure the patient that seborrheic dermatitis does not cause permanent hair loss.
Acne
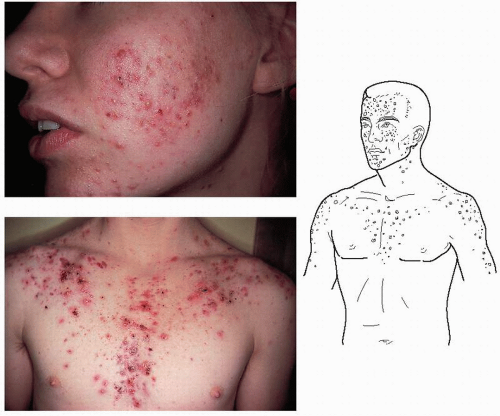
Acne vulgaris is a common skin condition of adolescents and young adults. It is characterized by any combination of comedones (blackheads and whiteheads), pustules, cysts, and scarring of varying severity (Figs. 13-4,13-5,13-6).
Severe cystic acne is called acne conglobata. When accompanied by systemic symptoms such as arthralgia, leukocytosis, and fever, the term acne fulminans is used. Hidradenitis suppurativa, also termed acne inversa, is a debilitating disease of deep undermining cysts and fistulas in the axillary, inguinal, and perirectal areas. Treatment is difficult and includes surgery, antibiotics, and isotretinoin (Accutane).
Dissecting cellulitis of the scalp (perifolliculitis capitis abscedens et suffodiens) is an inflammatory disease of the scalp with undermining cysts and fistulas of the scalp resulting in scarring alopecia. Treatment is difficult but antibiotics, surgery, laser, x-ray, isotretinoin, azathioprine, dapsone, colchicine, methotrexate, and systemic and intralesional corticosteroids may be helpful.
Acne conglobata, hidradenitis suppurativa, and dissecting cellulitis of the scalp have been referred to as the follicular occlusion triad. Pilonidal sinus is added by some authors to make this a tetrad.
Presentation and Characteristics
Primary Lesions
Comedones, papules, pustules, and, in severe cases, cysts occur.