Scar Camouflage
Elizabeth Allen
KEY POINTS
Camouflage can be a simple solution to complex problems.
Topically applied products are long lasting and waterproof.
Camouflage does not affect the skin or its structure, but does temporarily reduce the visual discoloration.
There are various brands and potentially over 300 natural skin colors available to select an acceptable color to match the unaffected skin.
History of Skin Camouflage
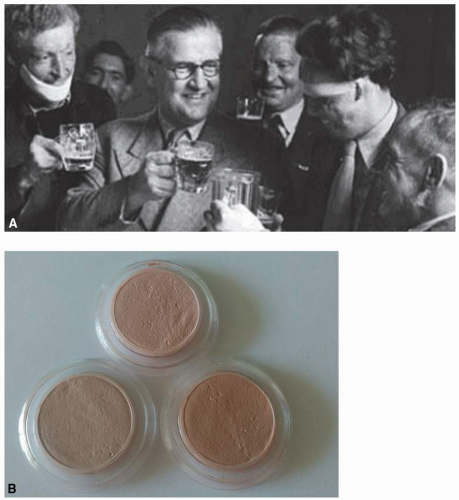
There is evidence to suggest that cosmetic preparations and prostheses have been used to cover scars since antiquity.1 The history of skin camouflage, as we know it today, began during World War II by the innovative plastic surgeon, Sir Archibald McIndoe, at the Queen Victoria Hospital, East Grinstead, West Sussex, England.2 His patients were all Royal Air Force (RAF) aircrew with burn injuries who formed (1941) The Guinea Pigs Club (28 founding members, 649 by the end of the war), which is acknowledged as being the first patient support group founded by patients for patients. McIndoe3 would proudly state, “It has been described as the most exclusive club in the world, but the entrance fee is something most men would not care to pay and the conditions of membership are arduous in the extreme” (see Fig. 20-1A).
McIndoe realized that scars and grafts frequently presented a different color to the surrounding skin—he could reconstruct a face, but this all too frequently resulted in a “patchwork” of skin colors. He wondered whether a topical preparation could be the solution. His first thoughts were toward Hollywood, where the Max Factor Corporation had created military camouflage for the U.S. Marines and waterproof theatrical pancake for use during Technicolor filming. He took these innovations to a colleague, Thomas Blake, and asked if the chemist could create waterproof camouflage crèmes that would mimic natural skin colors. The outcome was Veil Cover, initially with three colors (light, medium, and dark—dark being so called because it was darker than the other two) and all suitable for Fitzpatrick skin types I and II (see Fig. 20-1B).
The British Association of Skin Camouflage (BASC) founder, Joyce Allsworth, was a Women’s Auxiliary Air Force (WAAF) plotter at North Weald RAF Airbase during World War II and became aware of the air crew’s burn injuries at East Grinstead Hospital. She felt something had to be done to improve their well-being; after the war Joyce trained as a make-up artist and returned to McIndoe and his guinea pigs. No dated record exists of the initial interactions between them and Thomas Blake, although we do know that it was her suggestion that Veil increased its color range to include mixing colors such as rose, brown, and yellow (these colors still exist to this day). Over the years, Veil has continued to revise and increase its color range, and BASC is proud to be a part of that advisory process as well as a consultant to other companies that now include skin camouflage within their brand.
Mrs. Allsworth’s work was complemented by providing a comprehensive training program designed to increase the number of graduates in this specialty by training medical professionals (doctors, nurses, pharmacists, occupational therapists, and maxillofacial technicians), make-up artists, and beauty therapists. Her pioneering work has since expanded; BASC is the acknowledged major source of information and educators who train professionals to provide skin camouflage service within hospitals, clinics, and salons. BASC continues to be organized by professionals who volunteer their expertise. Although BASC-trained professionals work independently of the organization, we are proud of the part they play in helping others to face the world, with confidence.
The Desire to Be Accepted
We all have a great desire to be accepted by our community. In previous centuries, the majority of us would have worn the effects of life on our skin with some indifference. It would have been commonplace to see people with scars and pockmarks; given such acceptance, others would not have made disparaging comments. We might even hypothesize that people would be happy to associate with a scarred person because it indicated that, in these preantiseptic days, he or
she was a survivor. Sadly, modern times have changed this all-embracing attitude as we now live in an age that makes an instant judgment based on people’s outward appearance.
she was a survivor. Sadly, modern times have changed this all-embracing attitude as we now live in an age that makes an instant judgment based on people’s outward appearance.
The 21st Century requires us to have flawless (even ageless) skin, especially on our face. Such idealism is constantly fuelled by performing arts when all too frequently a villain is depicted with facial scarring—a premise perhaps based on gangsters such as Al Capone (who when photographed hid the scars on the left side of his face, saying that they were “war wounds” rather than the result of a fight)3—and cartoon characters, such as Batman’s The Joker. Unfortunately, such negative stereotyping4 can only serve to promote greater anxiety in those with scars or who consider their image to be psychosocially unacceptable.
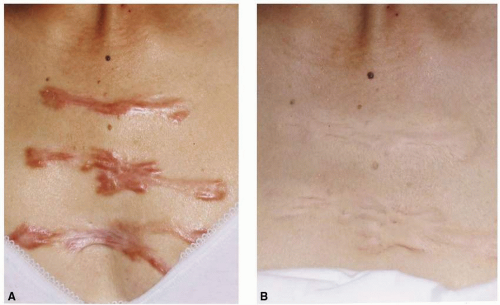
Research into keloid and hypertrophic scarring suggested that those with scar tissue 2 inches (5 cm) in length were particularly concerned, and that psychosocial inhibition was irrespective of the scar being immediately visible or hidden by clothing5 (see Fig. 20-2).
Unfortunately, there is no collective registry to indicate how many people have a scar. Neither has any official record been kept as to the number of people who benefit from using skin camouflage over their scarring. Scars are the result of many and varied causes, including accidents, violence, and disease. We can assume that most people expect their surgical procedure will create a scar, but they may not be aware of additional problems, as when the patient was psychologically adjusted to the scar but was worried by the vascular disturbance (she requested camouflage for the veins and not the scar) (see Fig. 20-3).
It has long been acknowledged that mind and body interact upon each other; it is axiomatic that when people are distressed by some aspect of their appearance, their general health and quality of life can be adversely affected. Although there is no single accepted definition of Health-Related Quality of Life (HRQoL), there are questionnaires available for professionals to measure the impact that skin conditions have on people’s well-being, such as the Dermatology Life Quality Index (DLQI)6 and the Hospital Anxiety and Depression Score, which patients complete themselves. All evidence supports the assertion that people experience higher levels of anxiety, depression, social isolation, difficulties at school, and unemployment than those whose skin is considered to be normal.7,8 Many people with scarring report that, at some point, they have met with rejection, name-calling, unwarranted comments, intrusive questioning, or verbal abuse. Without help, people can withdraw from employment, domestic and social-sporting activities, which may also affect the quality of life for their families. Studies into psychosocial behavior are well documented—all conclusions indicate that low self-esteem is equally devastating to men, women, and children, irrespective of religion, nationality, and skin classification group.9,10,11
 FIGURE 20-3 Camouflage used to reduce the visual effect of the residual vascular malformation following tumor removal. (© BASC member 1022.) |
Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.
—World Health Organization, Mental Health Fact Sheet No. 220, September 2010
BASC challenges the opinions of the few psychologists who consider the use of skin camouflage to be “avoidance of reality” and makes people reliant on this as a single coping strategy.12 We consider that if using skin camouflage helps someone to feel good about him or herself, if it gives them a tool to help their confidence grow, if it helps their return to ecosocial life, then should it not be encouraged? It is also immaterial whether the camouflage is worn occasionally or frequently, for a small scar or more extensive ones (see Fig. 20-4).
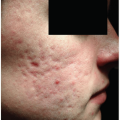
Sadly, some language used by professionals can be negative and alienate the scarred person. Labels, such as “disfigured,” may be a relevant medical description (especially when there is loss of a prominent facial feature, as the nose,
ear, or eye), but it is a word that the scarred person may find difficult to identify with; indeed, it may create further anxiety—perhaps a tipping point that might lead to eating disorders or self-harm? (see Fig. 20-5).
ear, or eye), but it is a word that the scarred person may find difficult to identify with; indeed, it may create further anxiety—perhaps a tipping point that might lead to eating disorders or self-harm? (see Fig. 20-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree