Case 1
Clinical Presentation
A 35-year-old Hispanic paraplegic female developed a sacral pressure sore when she was in hospital to give birth ( Fig. 33.1 ). This was the first time she had a pressure sore since she became paraplegic as a result of an accident. She was offered a flap reconstruction to close the sacral pressure sore after excision of the entire wound because she was a highly motivated individual with good social support from her husband. She fully understood the potential risks and benefits of the procedure and was willing to follow our postoperative instructions for an optimal flap healing.

Operative Plan and Special Considerations
Adequate surgical debridement for this sacral pressure wound should be performed first. With advance knowledge of perforator flap surgery, a gluteal perforator flap could be planned for the reconstruction. The flap itself can be based on one or two large perforators identified by an intraoperative Doppler finding. It can be raised as a V-to-Y fasciocutaneous advancement flap and the sacral soft tissue defect can be closed without tension. After the perforator has been identified, flap dissection can be done aggressively to elevate the entire skin paddle as an island flap. Such a flap’s advancement can be done freely to close a large sacral wound and the bulkiness of the flap can easily be advanced to fill any dead space of the sacral wound. Obviously, for any paraplegic patient, postoperative care is critical to ensure no tension or sheer force for the flap reconstruction site.
Operative Procedures
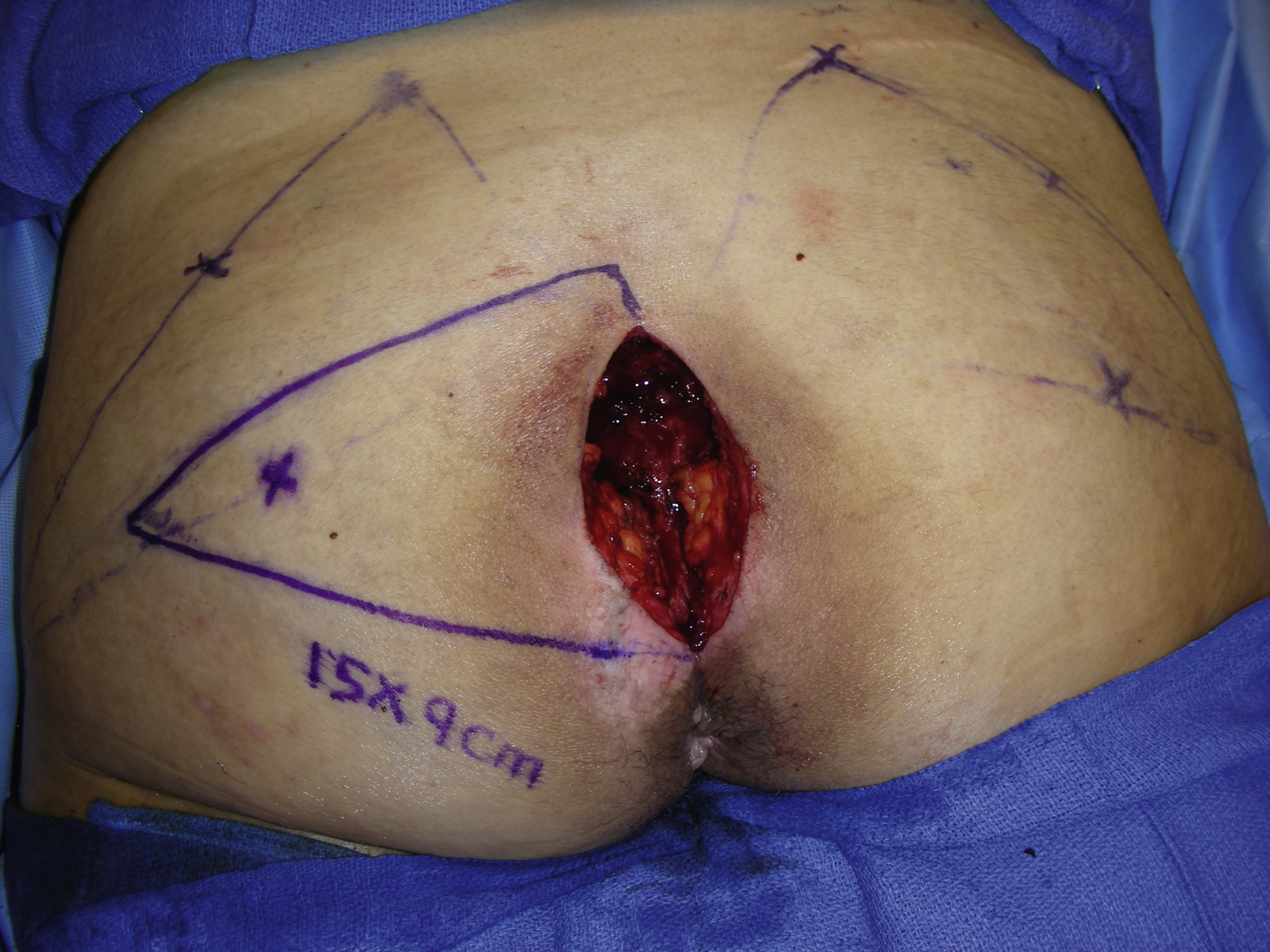
Under general anesthesia with the patient in a prone position, methylene blue was used to stain the entire bursa of the sacral pressure sore. Surgical debridement was first performed to excise the entire pressure sore including the bursa. This was achieved first by using a blade and including some normal skin and then by using electrocautery to remove the entire bursa of the sacral pressure sore. During the procedure, this patient had a significant amount of bleeding from several sizable vessels around the bursa of the pressure sore. All bleeding was controlled with hemoclips, electrocautery, surgicel, and pressure dressing. The wound was then irrigated with antibiotic solution
A 15 × 9 cm triangular, superior gluteal artery perforator flap was designed. Based on a preoperative duplex scan finding, there was a sizable perforator that measured about 2 mm in diameter with an excellent flow. Therefore, this perforator was included for the design of the superior gluteal artery perforator flap ( Fig. 33.2 ).
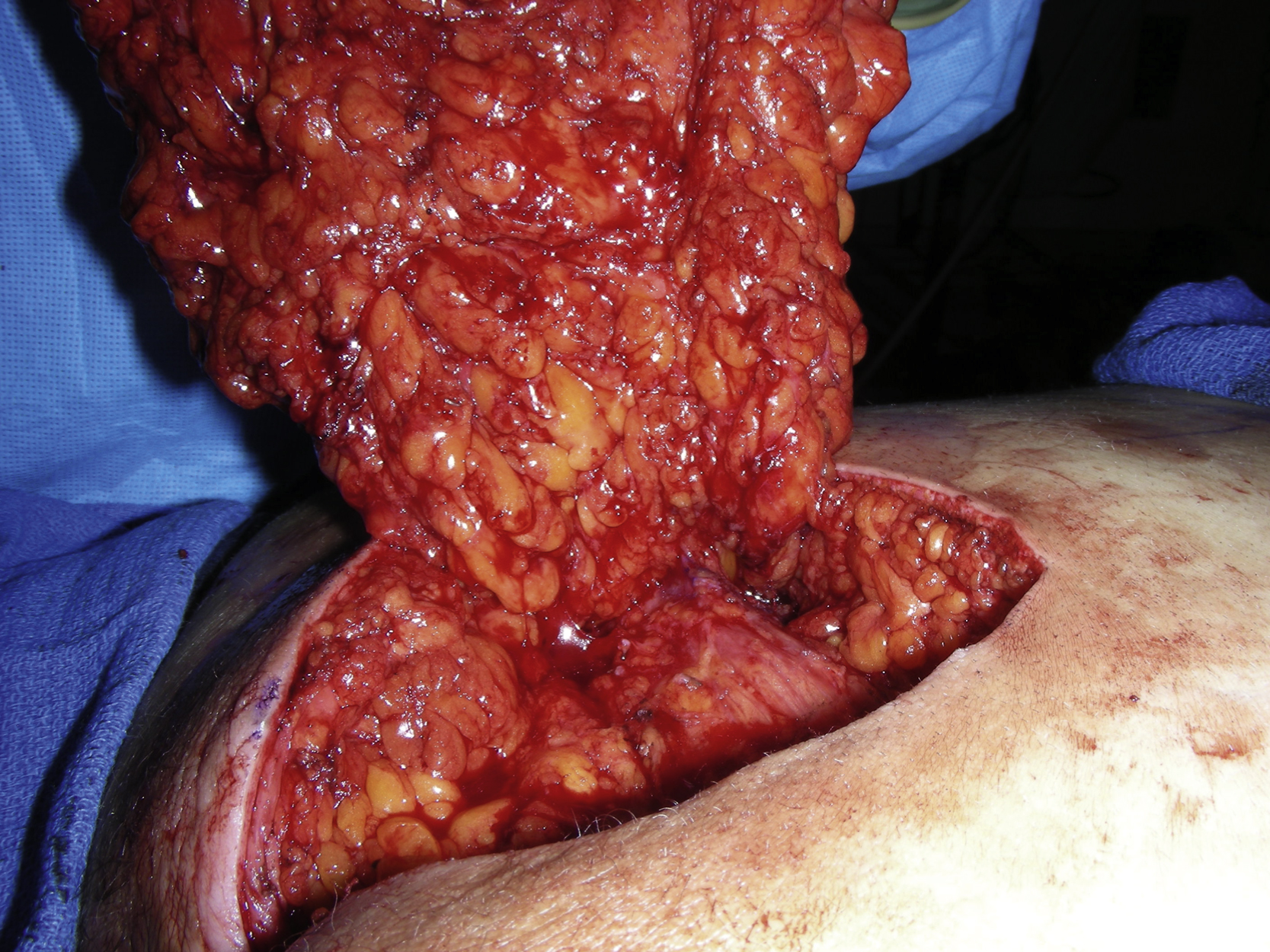
The skin incision was made along the planned triangular fasciocutaneous flap and was followed by subfascial dissection of the flap. Several small perforators were encountered but were divided. The flap’s attachment to the underlying superior gluteus muscle was then dissected freely and the superior gluteal artery perforator was identified ( Fig. 33.3 ). Precise dissection was performed around the perforator so that the flap could be advanced freely.

This single perforator-based superior gluteal artery perforator flap was then advanced into the midline sacral defect in a V-Y fashion without any tension ( Fig. 33.4 ). Some excess of the flap skin was trimmed and the flap was approximated to the contralateral midline without any tension. A 10-mm flat JP was inserted into the wound. The deep layer closure was approximated with several interrupted 2-0 PDS sutures. The deep dermal closure was made with several interrupted 3-0 Monocryl sutures. The skin closure was approximated first with four 3-0 nylons in half-buried horizontal mattress fashion. The rest of the skin closure was made with multiple skin staples ( Fig. 33.5 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








