Recovery and Reintegration After Burn Injury
Marta Rosenberg
Laura Rosenberg
Walter Meyer III
KEY POINTS
Recovery from a burn injury and its resulting scars can have lifelong psychological consequences.
Perceptions about body image and scarring following burn injury can be impacted by a person’s beliefs, values, family and social support, and experiences.
Most burn survivors adapt well and achieve optimal quality of life; however, some continue to struggle emotionally and physically.
Individuals who survive major burn injuries need to be monitored for difficulties with adjustment, trauma and stress related disorders such as posttraumatic stress disorder, and anxiety and mood disorders.
This chapter provides information about various aspects of recovery, interventions, and relevant research that has been done in burn care. A list of resources is provided to help burn survivors during their lifelong journey to recovery for community, school and work re-entry and social support.
Survivors of burns face adjustment to various physical, health, and psychosocial changes including acceptance of visible and hidden burn scars. Several factors may impact this adjustment including one’s belief system and perception of body image, perceived and actual support systems including family and friends, one’s comfort in diverse social settings, health status, resilience, and preburn and postburn emotional history. This chapter provides a summary of the literature related to the impact of burns (particularly burn scars); relevant aspects related to body image and stigmatization; psychosocial and psychiatric outcomes for burn survivors; the assessment and treatment of itch, neuropathic pain, and posttraumatic stress disorder (PTSD); and postburn social reintegration.
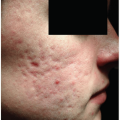
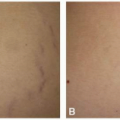
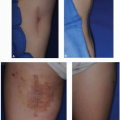
Visible and Hidden Scars
One of the frequent consequences of burns is scarring and contractures, and both surgical and nonsurgical methods have been used to address these issues.1 Reconstructive surgical interventions include, but are not limited to, application of skin grafts and skin flaps, release of contractures, scar reduction, tissue expanders2 (see Chapter 12), and more recently laser treatment (see Chapter 13). Nonsurgical methods include applying pressure on the scars through the use of pressure garments and skin massage, and attendance to daily rehabilitation and exercise programs2,3 (see Chapter 19).
Visible differences created by burn scars can lead to difficulties in physical and psychosocial functioning. Physical difficulties due to loss of function, pain, and itch are frequent and can impact daily functioning at home, work, and school and in diverse social settings. Psychosocial difficulties related to changes in appearance, difficulties accepting these changes, and difficulties with body image and self-concept may lead to social anxiety, depression, and problems with adjustment.4,5,6,7,8 Both visible and hidden scars (scars in areas usually covered by clothing) may impact how a person feels and their comfort in different social situations. They often experience unwanted attention and questions about their burn scars, which may make socializing uncomfortable. They may encounter social situations in which others do not quite know how to behave around them. Some survivors may attempt to cover up their scars to avoid uncomfortable social encounters (see Chapters 20 and 21). Therefore, the availability of social skills-based programs, cognitive-behavior therapy (CBT), and support systems is crucial for assisting survivors with postburn adjustment, acceptance of burn scars, gaining self-confidence, and feeling comfortable in different social settings. Studies are needed to identify which interventions are most effective for individuals with visible differences.8
Body Image and Stigmatization
Body image is an individual’s perception regarding physical appearance.9 This process is influenced by personal views
such as values and beliefs,7 social and cultural experiences,7,10,11 and appearance norms.7 In many countries people are often exposed to information about physical attractiveness from the mass media9,11 including magazines, television, movies, and more recently social media and individuals’ interests in taking selfies. Young children’s perceptions of their body image are influenced by messages they receive from their parents and family members.10,11 School-aged children begin to observe similarities and differences between themselves and their peers, and peer acceptance becomes increasingly important as children transition to adolescence.10,11 Body image concerns may continue throughout adult life.7
such as values and beliefs,7 social and cultural experiences,7,10,11 and appearance norms.7 In many countries people are often exposed to information about physical attractiveness from the mass media9,11 including magazines, television, movies, and more recently social media and individuals’ interests in taking selfies. Young children’s perceptions of their body image are influenced by messages they receive from their parents and family members.10,11 School-aged children begin to observe similarities and differences between themselves and their peers, and peer acceptance becomes increasingly important as children transition to adolescence.10,11 Body image concerns may continue throughout adult life.7
It is often believed burn survivors may experience body image dissatisfaction related to the changes in physical appearance due to scarring.12,13,14 Some studies found a modest relationship between burn scar severity and body image.15,16 Thombs and colleagues17 examined body image dissatisfaction of adult burn survivors at discharge and 6 and 12 months after injury. They found that women with major burns reported greater body image concerns, and that the importance of appearance was strongly associated with body image across time. Lawrence and colleagues18 examined the relationship between burn scar severity and body esteem of adults with burns. They found a strong relationship between scar severity and body-esteem for individuals who strongly valued their appearance. The opposite was true for individuals who rated their appearance as not important. In this study, females reported lower body-esteem with regard to appearance than males; however, males rated themselves as less attractive than others. Fauerbach and colleagues15 studied the impact of body image dissatisfaction on quality of life for adults with major burns. They controlled for burn size, facial injury, and preburn mental and physical quality of life. Results suggested burn survivors who were dissatisfied with their appearance experienced decreased mental and physical quality of life at 2 months postinjury.
Limited research has examined body image in pediatric burn survivors. Lawrence and colleagues16 compared body esteem of children with burns and an age-matched comparison group. No differences were found between the body esteem scores of men burn survivors and controls. However, women burn survivors reported higher body esteem than the comparison group. The authors speculated that the uniqueness of the sample, acceptance of burn scars, and social support may explain these findings.16 Russell et al.19 studied self-concept in young adults who sustained severe childhood burns. Burn survivors reported more difficulty on several subscales on a self-concept measure in comparison to a normative reference group. Areas of difficulty included: physical function, appearance, sexuality, moral conduct, personal values, academics and work, and identity. They reported that decreased self-concept was related to affective and anxiety disorders. Pope and colleagues20 compared long-term psychosocial outcomes of young burn survivors to a control group of peers from school. Burn survivors, especially men, reported better body image and weight satisfaction than the control group. However, as the size of burn increased there was more dissatisfaction with appearance and lower quality of life. The development of healthy coping strategies and acceptance of burn scars may explain these findings.20
Outcomes
Associated Psychological and Psychiatric Difficulties
The response of the person who suffers from a major burn injury is somewhat age dependent. Children grow up knowing their bodies have scars, so they may not experience a sense of loss. They simply cannot remember looking any different. They may or may not be teased or bullied, but regardless, they will be asked hundreds of times about their scars and appearance. They face questions such as how they got injured, if it hurts, etc. Several studies have explored the nature of related psychological and psychiatric sequelae. A few studies have looked at the long-term prevalence of any psychological and psychiatric problems that might be associated with scarring. In one study of 100 young adults burned as children (14 years earlier, on average), general psychological problems were assessed using the Achenbach scales for young adults.21 This self-report measure identifies behavioral problems such as anxiety/depression, somatic complaints, thought problems, attention problems, and aggressive and delinquent behaviors. These behaviors are further classified as internalizing or externalizing behaviors.22 The men in this study were not different from the reference population, except in the somatic complaints related to itching and pain. These symptoms may be assumed to be related to the scarred skin. However, the women in the same group were found to have an increased number of problems compared to the reference group. They had more withdrawn behavior, thought problems, aggressive behavior, and delinquent behavior.21 Some of this unusual behavior may be explained by the women being more concerned about their disfigurement than men.23
Even more unexpected and concerning is the prevalence of psychiatric disorders in this same group; approximately 50% of young adult survivors of large childhood burns met criteria for a major psychiatric disorder.24 Women had almost twice as many psychiatric disorders (Axis 1, DSM IV) as measured by the Structured Clinical Interview as men.24 This is true for both current and lifetime prevalence of the psychiatric disorders. Anxiety disorders were the most common, followed by affective disorders. The most common anxiety disorders were PTSD and social phobia, with any anxiety disorder being present in 30% to 37% of the young adults.24 Other studies have also reported that the women who suffered from burn scarring often have PTSD associated with their disfiguring injuries.25,26 There is a definite interaction between the symptoms of PTSD and the scars. A common presentation is that the scars are the major focus for many adolescent and adult burn survivors, perhaps because they are obvious and perhaps because they actually feel strange or are painful. The burn scars can be a trigger of the trauma and may complicate the person’s PTSD symptoms. This somatization may also be a symptom of underlying depression. When the pain is addressed as part of the treatment of their depression and anxiety, the outcome tends to be better.27 The medication used for the PTSD is usually a serotonin reuptake inhibitor such as fluoxetine or sertraline, but it may be a tricyclic antidepressant like amitriptyline. Amitriptyline or imipramine can be used to treat both the neuropathic pain28 and the acute stress disorder (ASD)/PTSD.29
Personality disorders are more prevalent in this long-term pediatric burn survivor population, with 49% of patients achieving threshold for diagnosis. Personality disorders were more likely to occur in adults who were burned as young children compared to those burned as teenagers. It appears that the experience of recovering from a major burn injury and growing up with major scars was more likely to shape personality development. The frequency was the same in both men and women. The most common types of personality disorders were paranoid in women and antisocial in men.30
Thomas and colleagues31 found that adolescent burn survivors have a significant amount of anxiety disorders. In that population the usual anxiety disorder was not PTSD, but rather agoraphobia, separation anxiety, and social phobia. In a meta-analysis study, the factors that affected outcome were the location and severity of the burn injury.32
Burn injury of the face and other visible areas can result in long-term psychological problems and psychiatric disorders, especially anxiety disorders. For all age groups, children and adolescents with facial burns had lower scores on psychosocial outcome measures than those without facial burns, whether the ratings were done by the parents or children.33,34 However, variability exists in the perceptions of parents and children following burn injury. Meyer and colleagues35 found that adolescent burn survivors and parents have similar ratings in the areas of physical and emotional health; however, adolescents in this study rated their appearance better than their parents. This may be because the adolescents felt confident about their appearance and had good family support. Robert and colleagues36 found that adolescent survivors of large burns exhibited similar or a higher degree of self-worth as compared to peers; however, they downrated their physical appearance and athletic competence. Similar results are found for hand burns, probably because hands are often noticed more than other parts of the body.37
The importance of diagnosing an associated psychiatric illness cannot be overestimated. Recently, Weichman and colleagues38 recommended some common tools to measure depression and anxiety in burn survivors, though most of these instruments are not specific to burns. The most validated ones are the following: Beck Depression Inventory-II,39 Hospital Anxiety Depression Scale,40 the Brief Symptom Inventory,41 and the Achenbach Child Behavior Checklist.42 However, the Achenbach Child Behavior Checklist is lengthy and more useful in outpatient settings.38,42 These instruments have an associated cost and require a mental health professional to administer. Therefore, Weichman’s group suggested a group of free brief scales for adults and children to screen for psychiatric complications. The Patient Health Questionnaire (PHQ-2 or 9) by Spitzer et al.43 is both free and screens for depression. For childhood depression the Children’s Depression Inventory (CDI) is recommended, even though it is not free.44 For assessment of PTSD in adults, the PTSD Symptom Checklist—Civilian version (PCL-C) is recommended45 and for children the UCLA PTSD Index46 is a reasonable choice38 (see Table 24-1).
Quality of Life
Outcomes research has focused on adjustment to the physical limitations and psychosocial changes resulting from burns for both adult and pediatric burn survivors. There is much variance in the results because of differences in methodology and the outcome measures used. Early investigations primarily used psychometric measures and clinical interviews to infer psychosocial functioning and postburn adjustment, and revealed that many burn survivors adjusted well.47,48,49,50 Later studies used health-related quality of life measures to investigate psychosocial outcomes of burn survivors. Several studies used the Short Form 36 (SF 36), a general health survey, to assess physical and emotional functioning of pediatric burn survivors. These studies found that the majority of survivors of large burns rated their functioning similar to the general population51,52; however, many adult survivors continued to have physical limitations that required additional rehabilitation services51 and continued to experience psychosocial distress.52 Measures that examine specific behaviors have also been used. Rosenberg and colleagues53 used the Quality of Life Questionnaire to assess specific behaviors related to quality of life with young adult pediatric burn survivors, and found that this group rated their overall quality of life slightly lower than the reference group. More recently, Murphy and colleagues54 examined the long-term psychological distress and quality of life of young adults who were burned as children using the World Health Organization Disability Assessment Scale II (WHODAS) and the Burn Specific Health Scale—Brief (BSHS-B), and found that quality of life decreased with increased burn size and that the WHODAS reliably identified individuals with lower quality of life.
Several researchers have specifically looked at health-related quality of life in children. Landolt et al.55 found that quality of life ratings of pediatric burn survivors were generally normal. However, lower quality of life ratings were associated with a diagnosis of PTSD. These authors also found that diminished social functioning was a primary problem,55 which is consistent with previous research done by Blakeney and colleagues.56 Similarly, Pope and colleagues20 found that pediatric burn survivors rated their quality of life higher than age-matched controls, had positive feelings about their appearance, and were coping well with life changes. However, women reported poorer quality of life. Murphy and colleagues54 found similar results when looking at long-term psychological distress and quality of life. They reported that children who were burned prior to school entry and adolescents who had not transitioned to young adulthood reported better quality of life and less disability. However, contrary to Pope’s findings, they found that women reported better quality of life.54 Stubbs and colleagues34 examined the psychosocial impact of childhood facial burns, and found that severe facial burns that required grafts significantly impacted the quality of life ratings of teenagers and their parents.
Other studies have focused on identifying predictors of quality of life. Anzarut and colleagues57 found that for adult survivors of large burns, the strongest predictors of physical functioning included total full thickness injury and hand function; the strongest predictors of emotional functioning included a younger age at time of injury and perceived level of social support. Similarly, Patterson et al.58 found that both psychosocial variables (preburn psychological status and social support) and medical variables (hand burns, amputations, and days in intensive care unit) predicted the outcome for adult burn survivors. Cromes and colleagues59 reported that less emotional distress, less pain, and greater involvement with home and social activities were predictive of better outcome among adult burn
survivors. Leblebici and colleagues60 found that having joint contractures significantly influenced burn survivors’ quality of life, especially their physical functioning, and that burn size affected psychosocial outcome. Pavoni and colleagues61 reported that in adults, quality of life was affected by psychological and physical limitations 1 year postinjury.
survivors. Leblebici and colleagues60 found that having joint contractures significantly influenced burn survivors’ quality of life, especially their physical functioning, and that burn size affected psychosocial outcome. Pavoni and colleagues61 reported that in adults, quality of life was affected by psychological and physical limitations 1 year postinjury.
Research has also focused on the benefits of a comprehensive wellness and exercise program in improving physical and psychosocial functioning following burn injury. Previous work by Suman and colleagues62,63,64 revealed that a comprehensive wellness and exercise program for pediatric survivors of large burns, administered 6 months postburn, significantly improved cardiopulmonary capacity, muscle mass and strength, and pulmonary function. Similarly, De Lateur and colleagues65 reported improvements with physical functioning for adult burn survivors who participated in a structured exercise program. Additionally, Rosenberg and colleagues66 found that parents reported significant improvements with their children’s physical and psychosocial functioning following a wellness and exercise program.
As youngsters transition into adolescence, young adulthood, and adulthood, they begin to question if they can have meaningful relationships with significant others and many have questions about intimacy and sexual activity. Women may question if they can give birth given the restrictions of the burn scars and contractures. Burn survivors need to be able to openly discuss these questions with their support systems including their psychologist, psychiatrist, plastic surgeon, family, and friends. The effects of scarring on sexuality and relationships are a major concern for men and women adult burn survivors. Few studies have examined this, though a group of young adults burned as children reported normal sexual activity.67 Both men and women reported having confidence about having sex and thinking they were sexually attractive. This did not vary much with scarring on the face and neck. However, there were exceptions. In general, women were able to find partners more readily than the men.67 This may be because the men were too self-conscious to ask. In one group session the men stated that they were too self-conscious to approach a woman, and the women said that they did not care what the men looked like, so long as they were nice and had a good job. Men were more likely to report having no sex since the burn injury.67 Bianchi found that men with higher sexual esteem had lower depression; however, there was no relationship between the severity of the burn and sexual esteem, depression, and preoccupation.68
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree