and Frank Hölzle2
(1)
Department of Oral and Maxillofacial Surgery, Klinikum rechts der Isar, Technische Universität Munich, Munich, Germany
(2)
Department of Oral and Maxillofacial Surgery, University Hospital of RWTH Aachen University, Aachen, Germany
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-319-53670-5_3) contains supplementary material, which is available to authorized users.
Despite the increasing development of thin perforator flaps and continuous sophistication of flap-raising techniques at nearly any donor site of the body, the RFF remains the most commonly used free flap, mostly raised as a standard fasciocutaneous flap with dissection deep to the forearm fascia [24, 504, 592]. Using this conventional approach, a number of modifications concerning the soft and hard tissue components of the flap and its design, volume, and shape are possible and open a wide range of indications [24, 464]. Nevertheless, the numerous advantages of this flap are limited by a significant incidence of donor-site morbidity, which is the major stimulus to search for alternatives to the RFF. As described above, partial loss of the skin graft, delayed healing, and tendon exposure are the most-reported complications after subfascial flap raising, and many proposals have been made to overcome these problems like oversewing the tendons with musculature [145], primary closure [358], bilobed flaps [233], Z-plasty [238], V-Y advancement flaps [76, 317, 567], and various suturing techniques to reduce the size of the donor defect [374, 504, 589]. According to wide clinical experience and retrospective studies, full-thickness skin grafts seem to have a better functional and esthetic outcome over split-thickness skin grafts [26, 76, 160, 250, 502] and negative pressure wound dressings can further improve the outcome of wound healing at the RFF donor site [12, 21–23].
The suprafascial radial forearm flap was introduced by Webster and Robinson in 1995, who reported a series of 300 cases over 11 years, in which they raised the flap without the deep fascia just as a skin flap. The authors started flap raising by incising the skin around the flap border and then raised the flap in the subcutaneous plane superficial to the forearm fascia, until the flexor carpi radialis tendon and the brachioradialis tendon became visible. At this point, they incised the fascia longitudinally, taking care to preserve the paratenon of the underlying tendon, identified the radial vessels from both sides, and ligated the vessels distally with preservation of the superficial branch of the radial nerve. Finally, they developed the radial vessels on the surface of the flexor hallucis longus and further up to the elbow, thereby leaving intact the septocutaneous vessels within the filmy lateral intermuscular septum. With this technique, a success rate of 98% was obtained [581].
Based on intraoperative observation, Chang and coworkers hypothesized that the RFF can be raised as a septocutaneous flap without including the deep forearm fascia, and they further refined the above technique. In their paper, they described a conjoining of two layers of the deep forearm fascia between the brachioradialis and flexor carpi radialis tendons. They found an investing septum around the radial vessels, formed by the superficial layer of the forearm fascia, containing also all the septocutaneous perforators running to the overlying skin. To obtain a vascularized graft recipient bed over the entire donor site, they preserved the deep layer of the forearm fascia over the underlying flexor tendons. In a series of over 400 patients, they could obtain a more suitable recipient site for skin grafts with this modification [77]. According to their description, the incisions are taken down to the subcutaneous level only, leaving the cephalic vein behind, and the dissection is carried out toward the radial vessels from both sides in a suprafascial plane until the flexor carpi radialis and brachioradialis muscles have been reached. Then, the radial vessels were ligated distally, the superficial layer of the deep fascia was divided on either side of the lateral intermuscular septum, and they elevated the flap mainly from distal to proximal, including the vessels and a strip of the overlying intermuscular septum. In their modification, the dissection plane for the pedicle was immediately beneath its inferior surface, but above the deep fascia between the brachioradialis and flexor carpi radialis tendons. The donor site was usually closed with a thick split-thickness skin graft.
In their first series of 49 patients, which they followed over 18 months, Chang et al. found a 100% skin take and normal tendon excursion. After these encouraging results, prospective studies have been carried out by other groups that supported the hypothesis of a more suitable skin graft recipient site following suprafascial flap raising. These authors point out that the vascularized forearm fascia can also protect the skin graft from the movement of the underlying tendon, leading to an incidence of graft failures of only 4% for full-thickness and 6% for split-thickness skin grafts [21, 326]. Moreover, delayed healing was reduced significantly [21, 25, 326] with the exposure of flexor tendons in only 3% if the flap was raised in the level above the deep fascia compared to 33% when using the conventional technique [78]. In their prospective study, Lutz et al. also analyzed the functional outcome at the donor site and showed that the range of motion and the strength of the hand revealed no significant changes, and the esthetic outcome was rated good or fair in 98% of their cases [325].
Despite the proven advantages, there is still a lack of popularity of the suprafascial flap-harvesting technique, probably due to concerns about the role of the deep fascia and its contribution to flap perfusion. Therefore, an anatomic study using injections of dye and barium sulfate was performed by Schaverien and Saint-Cyr, who compared the vascular territories in radial forearm flaps, raised either with or without the deep fascia [471]. Moreover, they studied the vascularity of the deep forearm fascia by intraarterial injection of red latex. The authors clearly found no significant difference in the areas of the vascular territories of the suprafascial compared with the conventional subfascial flaps. According to the results of microdissection and CT scans, the subfascial vascular plexus was only poorly developed and played no role in flap perfusion, whereas the suprafascial plexus showed a dense network of vessels within the adipose layer, being well protected during suprafascial flap raising. The authors concluded that all vessels relevant for flap perfusion are maintained during suprafascial harvesting of the radial forearm flap (◘ Fig. 3.1).
3.1 Flap Raising
Ulnar Skin Incision
After positioning of the arm and designing the flap, which does not differ from the conventional flap-raising procedure, the skin is first incised along the ulnar flap margin including the thin layer of fatty tissue, but without touching the deep fascia. Through the fascia, the tendon of the flexor carpi ulnaris muscle is visible, but the fascia is not opened (◘ Fig. 3.2).
Defining the Suprafascial Dissection Plane
To make sure you are following the right dissection plane, the forearm fascia is grasped with a forceps, and the fatty layer is gently elevated, opening the correct space for further dissection. Note the dense structure of the fascia, which firmly covers the flexor tendons and muscles (◘ Fig. 3.3).
Distal Skin Incision and Approaching the Septum
Next, the skin is incised distally, the skin flap is lifted up, and a sharp dissection is performed right above the deep fascia, until the flexor carpi radialis tendon becomes visible. When incising distally, care must be taken not to injure the deep fascia, because a fatty layer is almost not existent close to the flexor crease. The fine vascular network which spreads along the subcutaneous tissue is safely included into the flap (◘ Fig. 3.4).
Exposing the Radial Vessels
The distal skin incision is extended across the lateral intermuscular septum, and the radial vessels as well as the superficial branch of the radial nerve are exposed. To approach the vessels, the deep forearm fascia is punctually opened on both sides of the lateral intermuscular septum (◘ Fig. 3.5).
Ligating the Radial Vessels and Identifying the Lateral Intermuscular Septum
The radial vessels are ligated distally, and the proximal skin incision is carried out, again without injuring the deep fascia. The flexor carpi radialis tendon can now be seen, forming the ulnar margin of the lateral intermuscular septum. Note that the deep fascia is covering all the tendons completely. At this point, the dissection ends exactly at the medial rim of the flexor carpi radialis tendon (◘ Figs. 3.5 and 3.6).
Opening the Deep Fascia Medial to the Septum
Without exposing the paratenon, the forearm fascia is sharply incised along the medial rim of the flexor carpi radialis tendon. When doing this, the envelope of the radial vessels, formed by the lateral intermuscular septum, remains untouched. Therefore, this step must be carried out carefully, allowing to separate the septum very gently from the flexor tendon. This is facilitated by bringing the skin flap and fascia a little bit under tension, so that the tissues almost separate spontaneously in the right plane (◘ Figs. 3.7 and 3.8).
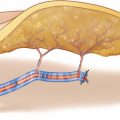
Dissecting the Radial Vessels
With the help of a fine hook, the flexor tendon, which is still completely covered by the deep fascia, is pulled medially, and together with the lateral intermuscular septum the radial vessels are separated from their deep attachment at the flexor pollicis longus muscle. Note that a fine layer of the deep fascia still covers the flexor pollicis longus muscle, and that the radial vessels are firmly attached to the skin flap along its entire length. Moreover, the whole subcutaneous vascular network is included into the flap (◘ Fig. 3.9).
Defining the Radial Flap Margin
Dissection now proceeds at the radial flap margin, above the brachioradialis muscle. The skin is folded back, and the position of the superficial branch of the radial nerve is used to mark the lateral flap border. Often, the nerve can be palpated as it courses underneath the thin skin, which helps to protect it during the incision (◘ Fig. 3.10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree