Posterior Cranial Vault Expansion
Alexander Y. Lin
DEFINITION
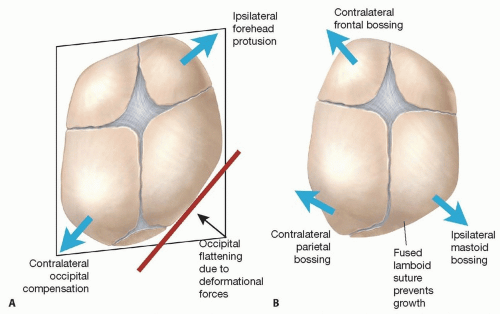
Posterior plagiocephaly, or flattening of the posterior skull, can be the result of deformational (positional) forces or of fused sutures (lambdoid craniosynostosis) (FIGS 1 and 2):
This distinction is critical, as deformational plagiocephaly can be improved nonsurgically with repositioning or orthotics, whereas craniosynostosis requires surgical repair.1
Surgical repair is necessary for craniosynostotic posterior plagiocephaly, which can be corrected with posterior cranial vault expansion.
Posterior cranial vault remodeling is the set of plastic surgery techniques to perform open repair in one stage, by designing full-thickness cranial bone grafts that are neurosurgically elevated and rebuilding the posterior cranial vault with these grafts via fixation (usually resorbable sutures or plates in infants, although nonresorbable hardware can be considered in older patients).
ANATOMY
The normal infant growing skull has five major bones separated by growth sutures: the metopic suture separates the two frontal bones, which posteriorly border the bilateral coronal sutures that adjoin the two parietal bones separated by the sagittal suture at the midline, which forms the lambda where it meets the bilateral lambdoid sutures that posteriorly define the occipital (FIGURE 1).
Craniosynostotic posterior plagiocephaly is usually due to nonsyndromic lambdoid craniosynostosis (unilateral or bilateral) or multisutural syndromic craniosynostosis:
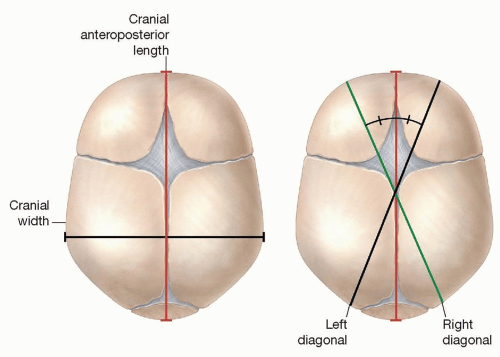
Cranial index (CI) is defined by cranial width divided by cranial anteroposterior length and is a relative index to help categorize scaphocephaly (CI less than 0.76) vs brachycephaly (CI greater than 0.86):
Cranial vault asymmetry (CVA) is the difference of the two diagonals from frontozygomatic suture to contralateral occipital prominence (normal less than 4 mm).
Cranial vault asymmetry index (CVAI) is CVA divided by the longer diagonal (normal less than 3.5).
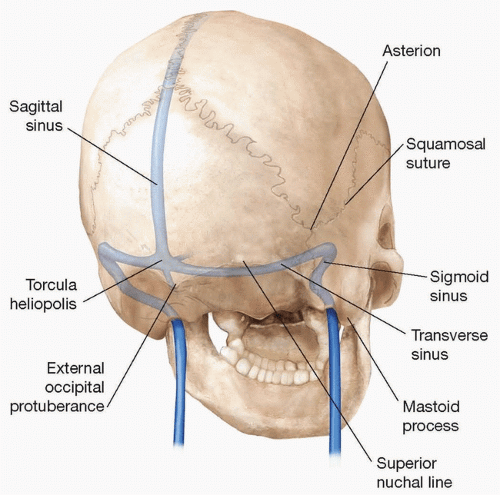
The midline sagittal sinus ends posteriorly at the torcula, located at the occipital protuberance or inion, and then branches laterally along the superior nuchal line to the bilateral transverse sinuses, which emit emissary veins below the asterion and posterior to mastoid process, to become the bilateral sigmoid sinuses:
PATHOGENESIS
Craniosynostosis may be due to genetic or developmental etiologies. Growth of bone is perpendicular from the direction of the suture; therefore, suture fusion prevents perpendicular growth, leading to parallel compensatory growth along the line of the suture:
Consequently, in unilateral lambdoid craniosynostosis, compensatory bossing occurs along the line of the suture, enlarging the ipsilateral mastoid and contralateral parietalregions, resulting in a trapezoidal head shape from bird’s-eye view (see FIG 2B).4
Deformational skull changes occur with a high prevalence because the infant skull is malleable to allow rapid brain growth (FIG 2A):
The “back-to-sleep” supine sleeping campaign has reduced sudden infant death syndrome (SIDS)7 but has resulted in a higher number of infants with deformational plagiocephaly.
In the setting of craniosynostosis, simultaneous deformational forces, from infant sleeping position, may unpredictably affect the craniosynostosis head shape pattern.
NATURAL HISTORY
Craniosynostosis occurs about 1 in 2000 live births.
Sagittal (40%-57%)
Metopic (10%-21.5%)
Coronal (15%-30%)
Lambdoid (1%)
Multisutural (13%)
PATIENT HISTORY AND PHYSICAL FINDINGS
Head shape problems manifest early in infancy; rapid infant brain growth leads to rapid exaggeration of the abnormal vectors of growth.
History should include questions about preferred sleeping position, head tilt related to torticollis, complete closure of eyes when asleep to infer supraorbital rim abnormalities, and neurological symptoms that may suggest elevated intracranial pressure (ICP).7
For posterior plagiocephaly, the physical exam must distinguish the common deformational plagiocephaly, from the rare lambdoid craniosynostosis.
Both can present with unilateral posterior flattening, but deformation causes a parallelogram-shaped head with ipsilateral forehead protrusion and contralateral occipital compensation.
IMAGING
DIFFERENTIAL DIAGNOSIS
Posterior deformational plagiocephaly
Lambdoid craniosynostosis (isolated)
Lambdoid craniosynostosis (multisutural)
SURGICAL MANAGEMENT
The timing of surgery depends on the presenting symptoms but preferably before 12 months of age to take advantage of the osteogenic potential of the dura, which dissipates by about 2 years of age.14 In addition, frontofacial asymmetries are more likely to automatically improve with growth, if craniosynostosis surgery is performed before 12 months of age.15

FIG 5 • Posterior coronal view of 3D CT scan of infant with right unilateral lambdoid craniosynostosis, who also has a right shunt. Note the ipsilateral mastoid and contralateral parietal expansion, in line with the synostosed suture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access