Posterior Cranial Vault Distraction Osteogenesis
Richard A. Hopper
Amy Lee
DEFINITION
Posterior cranial vault distraction osteogenesis (PVDO) increases intracranial volume through gradual expansion of a circumferential cranial osteotomy using manually activated buried distraction devices.1
PVDO is indicated in patients with premature fusion of multiple cranial sutures (synostosis) resulting in craniofacial dysmorphology, cephalocranial disproportion, and the risk of increased intracranial pressure.
ANATOMY
The anterior fontanelle is at the junction of the coronal and sagittal sutures.
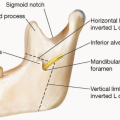
The pterion is an indentation at the anterior portion of the temporal bone corresponding intracranially to the lesser wing of the sphenoid.
The petrous ridge is a focal elevation of the dural adhesion to the skull base at the posterior temporal bone in line with the inferior aspect of the lambdoid suture.
The sagittal venous sinus of the brain is typically located in the upper midline but can be asymmetric in complex cases.
The transverse venous sinuses are usually located in the middle of the posterior cranium but can be inferiorly displaced closer to the skull base in syndromic cases such as Apert and Pfeiffer syndromes.
The confluence of the sagittal and transverse sinuses is the torcula.
PATHOGENESIS
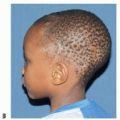
Brachy-turricephaly describes a cranial shape with restricted growth in the anteroposterior direction (brachy = short) with compensatory growth in the superior direction (turri = tower).
The development of brachycephaly typically results from premature fusion of one or more of the posterior cranial sutures (lambdoid and sagittal) in association with fusion of one or more of the anterior coronal sutures.
The associated turricephaly results from compensatory vertical expansion of the developing brain through overexpansion and bone effacement in the squamosal and frontozygomatic sutures as well as the anterior and posterior fontanelles.
Primary skull base anomalies in the pterion and petrous ridges of syndromic cases exacerbate this deformity.
Most PVDO procedures are performed on patients with brachy-turricephaly associated with FGFR2 mutations such as Crouzon, Apert, and Pfeiffer syndromes.
Complex multiple suture synostoses such as the kleeblattschädel deformity or Mercedes pattern (sagittal and bilateral lambdoid) synostosis can also benefit from PVDO.
NATURAL HISTORY
Without surgical treatment through cranial release or expansion, the brachy-turricephaly deformity is progressive in the first years of life.
Eventual closure of the fontanelles and patent sutures prevents continued compensatory growth, and cephalocranial disproportion occurs, resulting in increased intracranial pressure.
Frontal surgeries such as fronto-orbital advancement and monobloc procedures provide less intracranial expansion than does PVDO but can be performed after PVDO if further expansion is required.
PVDO provides more intracranial volume expansion per millimeter advancement than frontal surgeries due to the increased surface area of the transported bone.2,3
The severe thumbprinting of the posterior calvarium seen in patients prior to PVDO will progress without intervention.
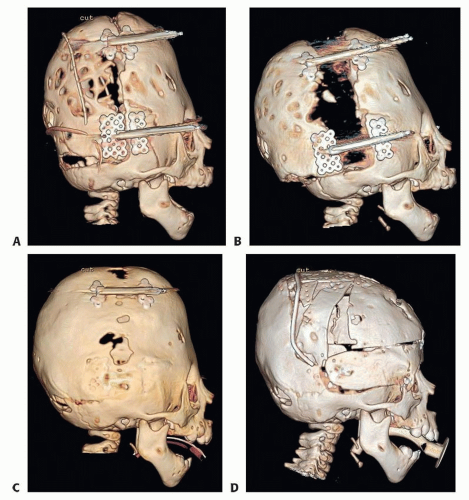
With the improved cephalocranial proportion achieved by PVDO, this thumbprinting often resolves soon after activation is complete (FIG 1).
PATIENT HISTORY AND PHYSICAL FINDINGS
Interdisciplinary assessment of airway, feeding, genetics, and potential associated anomalies must be performed before PVDO.
Neurosurgical assessment is completed for associated conditions such as Chiari malformation or hydrocephalus.
Patients with documented hydrocephalus will require appropriate treatment with a cerebrospinal fluid (CSF) shunt procedure prior to PVDO to prevent progressive cranial deformity and nonhealing of the cranial expansion defects postoperation.
Patients with documented symptomatic Chiari malformations will require treatment before PVDO, but in rare cases, bone decompression of the foramen magnum can be performed simultaneously through the coronal incision.
Asymptomatic Chiari malformations can improve with PVDO or be directly decompressed during the same procedure.4,5
Whenever possible, a full ophthalmologic examination including dilated funduscopy or visual evoked potentials should be performed prior to intracranial surgery.
IMAGING
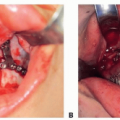
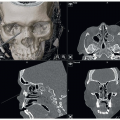
A low-dose three-dimensional CT scan can help in osteotomy marking, device placement, and vector planning.
The thickest bone along the planned osteotomy is optimal for screw fixation of the devices.
Vector planning on the images should optimize volume expansion and avoid shearing of the dura, and step-off deformities (see Technique section).
A contrast CT scan or magnetic resonance angiogram is indicated for syndromic patients to assess the location of the transverse and sagittal sinuses, which can be more inferior and off midline respectively in these patients.
Posterior circular cranial defects on CT scan can be indicative of anomalous intracranial venous drainage to the skin, and disruption of this drainage should be avoided to prevent increased intracranial hypertension6,7 (FIG 2).
Virtual computer planning with or without stereolithographic models, cutting guides, and sinus marking can be beneficial in complex cases.
Stereolithographic models can allow prebending of distraction device footplates to ensure a parallel vector.
Serial lateral plain film cephalograms are effective in following cranial expansion and to ensure devices remain stable on the cranium in cooperative patients.
SURGICAL MANAGEMENT
PVDO treats the posterior volume restriction associated with brachy-turricephaly to permit unrestricted brain growth in infancy.
Without the increased intracranial volume (ICV) achieved from a preceding posterior cranial expansion, turricephaly is often not able to be addressed with a frontal surgery alone due to an insufficient ICV to displace the brain inferiorly.
PVDO is typically performed on patients with multiple suture synostosis in the first year of life to allow frontal surgeries such as fronto-orbital advancement or monobloc to be done at an older age when stability is more reliable and the complication and relapse rate is decreased.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree