Pigmentary Dermatoses
John C. Hall MD
There are two variants of pigmentation of the skin: hyperpigmentation and hypopigmentation. The predominant skin pigment discussed in this chapter is melanin, but other pigments can be present in the skin. A complete classification of pigmentary disorders appears at the end of this chapter.
The melanin-forming cells and their relationship to the tyrosine-tyrosinase enzyme system are discussed in Chapter 1. The common clinical example of abnormal hyperpigmentation is chloasma, but secondary melanoderma can result from many causes. The most common form of hypopigmentation is vitiligo, but secondary leukoderma does occur.
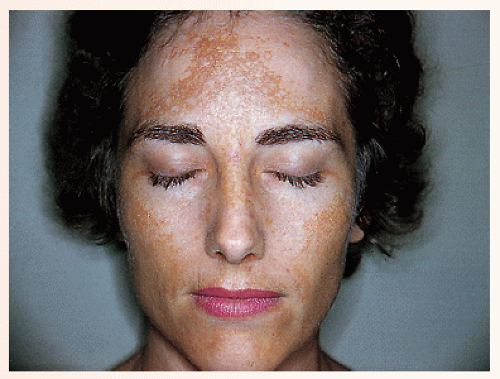
Chloasma (Melasma)
Presentation and Characteristics
Clinical Lesions
An irregular hyperpigmentation of the skin that varies in shades of brown is seen. It is well demarcated and located most often on the face in sun-exposed areas (Fig. 36-1).
Distribution
The lesions usually occur on the sides of the face, forehead, and sides of the neck.
Course
The disorder is slowly progressive, but remissions do occur. It is more obvious in the summer.
Cause
The cause is unknown, but some cases appear during pregnancy (called “mask of pregnancy”) or with chronic illness. There is an increased incidence of chloasma in women taking contraceptives, postmenopausal hormone replacement, or fertility hormones. The melanocyte-stimulating hormone of the pituitary may be excessive and affect the tyrosine-tyrosinase enzyme system.
SAUER’S NOTES
1. Skin pigmentation is the most socially significant skin marker, and care must be taken not to underestimate its importance to the patient even if it is not harmful to the patient’s medical well-being.
2. Change in skin pigmentation can be an important marker for underlying illness.
3. The safest and most beneficial therapy may be camouflage, that is, Lydea O’Leary Covermark or Dermablend.
Differential Diagnosis
The causes of secondary melanoderma should be ruled out (see end of this chapter).
Treatment
1. The patient should not be promised great therapeutic results. Most cases associated with pregnancy slowly fade or disappear completely after delivery. The pigmentation may be prolonged if the patient elects to breast-feed.
2. For a mild case in an unconcerned patient, cosmetic coverage can be adequate. Dermablend or Lydia O’Leary Covermark are two useful products.
3. Sunlight intensifies the pigmentation, so a sunscreen should be added to the routine each morning year-round.
4. Hydroquinone preparations (any of the following): Melanex solution 3%
Lustra cream 4%
Eldopaque Forte cream (tinted)
Solaquin Forte cream (nontinted)
Eldoquin Forte
Lustra AF (sunscreen)
Lustra-Ultra (sunscreen, retinol) 4% Hydroquinone Cream is an inexpensive generic preparation.
Tri-Luma (fluocinolone, tretinoin)
EpiQuin (microsponge)
Glyquin (glycolic acid)
Comment: Tri-Luma contains a retinoid, a class VI corticosteroid, and hydroquinone. This product should show a response within 8 weeks and some authors restrict its use to this time period and then have a rest period because it contains a corticosteroid. They then switch to a sunscreen and hydroquinone combination. There are many variants of these topicals, all with hydroquinone and some with sunscreens, glycolic acid, and retinoids. They all tend to be expensive with the exception of over-the-counter hydroquinone. Insurance considers these products cosmetic and seldom defrays the cost.
Sig: Apply locally b.i.d. Stop if irritation develops.
Comment: The treatment with any of these hydroquinone preparations should be continued for at least 2 to 3 months. Response to therapy is slow. When they are stopped, the disease tends to recur. Prolonged use over many months to years can cause increased pigmentation owing to an acquired ochronosis. This resolves on discontinuing the hydroquinone.
5. Retinoic acid (Retin-A cream [0.025%, 0.05%, 0.1%] or gel, Renova [0.02%]) applied at night can slowly decrease the pigmentation, if tolerated.
6. Kojic acid is advocated by some authors.
7. Surgical procedures used by experienced physicians include microdermabrasion, laser, and chemical peels. Beware of the danger of hypopigmentation.
Vitiligo
Presentation and Characteristics
Clinical Lesions
Irregular areas of depigmented skin are seen with a hyperpigmented border (Fig. 36-2). There is a segmental variety that has pigment loss in a dermatomal (especially trigeminal) distribution.
Distribution
It is estimated to affect 1% to 2% of the population. It is a more severe cosmetic problem in darker skinned patients. Most commonly, the lesions occur on the face and the dorsum of hands and feet, but they can occur on all body areas.
Course
The disease is slowly progressive, but remissions and changes are frequent. It is more obvious during the summer because of the tanning of adjacent normal skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree