Other Papulosquamous Dermatoses
John C. Hall MD
Papulosquamous eruptions, as indicated by the name, infer elevation and desquamation of the skin. Seborrhea (Chapter 13), the only one of these conditions with a greasy scale, and psoriasis (Chapter 14) are the most common. Most of these conditions are inflammatory, but tinea versicolor is included here due to the similarity of its clinical appearance to the other papulosquamous conditions. Lichen nitidus (see Dictionary-Index) and lichen striatus (see Dictionary-Index) are also considered in the category of papulosquamous skin diseases.
Pityriasis Rosea
Pityriasis rosea is a moderately common papulosquamous eruption, mainly occurring on the trunks of young adults (Figs. 15-1,15-2,15-3). It is mildly pruritic and occurs most often in the spring and fall.
Presentation and Characteristics
Primary Lesions
Papulosquamous, oval erythematous discrete lesions are seen. A larger “herald patch” resembling a patch of “ringworm” may precede the general rash by 2 to 10 days. A collarette of fine scaling is seen around the edge of the lesions. It begins just inside the pink plaque.
Secondary Lesions
Excoriations are rare. Secondary lesions are the effect of overtreatment or contact dermatitis from topical treatment.
Distribution
The lesions appear mainly on the chest and trunk along Langer’s lines of cleavage in the skin. Many cases have the oval lesions in a “Christmas tree branches” pattern over the back. In atypical cases, the lesions are seen in the axillae and the groin only. This is sometimes referred to as inverse pityriasis rosea. Facial lesions are rare in light-skinned adults but are rather commonly seen in children and people of color.
Course
After the development of the herald patch, new generalized lesions continue to appear for 2 to 3 weeks. The entire rash most commonly disappears within 6 to 8 weeks. Recurrences are rare. There are recurrent and long-lasting variants.
Subjective Complaints
Itching varies from none to severe but is usually mild. Hot showers or baths may exacerbate the itching.
Cause
The cause is unknown. Some authors have incriminated human herpesvirus 6 (HHV-6) and human herpesvirus 7 (HHV-7).
Season
Spring and fall “epidemics” are common.
Age Group
Young adults and older children are most often affected.
Contagiousness
The disease is not contagious.
Differential Diagnosis
Tinea versicolor: Lesions are tannish and irregularly shaped; fungi are seen on scraping and fine, dry, adherent scale becomes apparent when the physician scratches the area with the fingernail.
Drug eruption: No herald patch; positive drug history for gold, bismuth, or sulfa (see Chapter 8).
Secondary syphilis: No itching (99% true); history or presence of genital lesions; positive blood serology; palmar lesions present (see Chapter 26).
Psoriasis: Usually on elbows, knees, and scalp; lesions have a thick, adherent, silvery-white scale.
Seborrheic dermatitis: Greasy, irregular, scaly lesions on the sternum, central face, external auditory
canals, scalp, between the buttocks, and on the genitalia (see Chapter 13).
Lichen planus: Lesions are more papular and violaceous; found on the mucous membranes of the mouth and lip; very pruritic and common on flexor wrists.
Parapsoriasis: Rare; chronic form may have fine “cigarette paper” atrophy; can develop into mycosis fungoides (cutaneous T-cell lymphoma [CTCL]).
Treatment
First Visit
1. Reassure the patient that he or she does not have a “blood disease,” that the eruption is not contagious, and that it would be rare to get it again.
2. Colloidal bath
Sig: Add 1 packet of Aveeno oatmeal preparation to the tub containing 6 to 8 in lukewarm water. Bathe for 10 to 15 minutes every day or every other day.
Comment: Avoid soap and hot water as much as possible to reduce any itching.
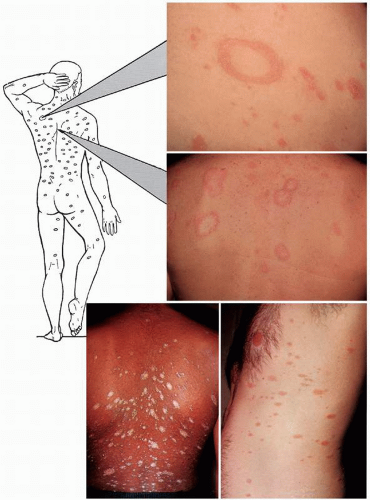 FIGURE 15-2 ▪ Pityriasis rosea. Bottom left photograph is of an African-American patient. (Courtesy of Westwood Pharmaceuticals.) |
3. Use nonalcoholic white shake lotion or Calamine lotion q.s. or any topical with pramoxine (Pramosone lotion, cream, or ointment and, over the counter, Sarna for sensitive skin, among many others)
Sig: Apply b.i.d. locally to affected areas.
4. If there is itching, prescribe an antihistamine. Cyproheptadine (Periactin), 4 mg #60
Sig: Take 1 tablet a.c. and h.s.
5. UVB therapy in increasing suberythema doses once or twice a week may be given. The severity is decreased, but itching and disease duration are probably not altered.
Subsequent Visits
1. If the skin becomes too dry from the colloidal bath and the lotion, stop the lotion or alternate it with Hydrocortisone cream or ointment, 1% q.s. 60.0
Sig: Apply b.i.d. locally to dry areas.
2. Continue the ultraviolet treatments.
Severely Pruritic Cases
1. In addition to the above, add
Prednisone, 5 mg #40











