Osteochondritis Dissecans
Donald S. Bae
Overview
Osteochondritis dissecans (OCD) of the capitellum is a common cause of pain and functional limitations in adolescent upper extremity weight-bearing or overhead athletes
Patients present with pain, loss of elbow motion, and mechanical symptoms of locking or giving way
Radiographs and advanced imaging—particularly magnetic resonance imaging (MRI)—will confirm the diagnosis and aid in classification
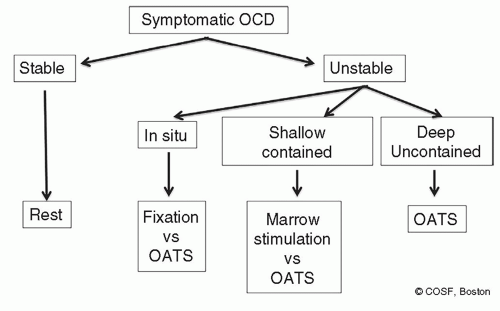
Rest is recommended for stable lesions, although healing rates have been reported to be between 50% and 90% and may take 12 to 15 months
Surgical treatment is typically recommended for unstable OCD lesions, with the goals of preserving articular congruity, restoring healthy subchondral bone, and maintaining radiocapitellar stability
Surgical treatment options are varied, and include the following:
Loose body removal and debridement, typically done arthroscopically
Transarticular or retrograde drilling of OCD lesions to stimulate vascular ingrowth and healing
Microfracture of the donor site to promote formation of fibrocartilage
Internal fixation of unstable in situ lesions to achieve healing
Osteochondral grafting to replace the OCD lesions with healthy hyaline cartilage and subchondral bone
A current treatment algorithm is presented in Figure 11.1
Operative Indications
Surgery is indicated for symptomatic patients with unstable OCD lesions or those with stable lesions that have not demonstrated progressive healing with at least 6 months of rest.
Equipment
Small joint arthroscope (typically 2.9 mm) and appropriate arthroscopic graspers and shavers
Traction boom or positioning device for the operative limb
Microfracture picks, awls, or smooth small-diameter Kirschner wires (K-wires) for microfracture
Bioabsorbable tacks for internal fixation (Smartnails, Conmed, Utica, NY)
Osteochondral grafting instruments (Osteochondral Autologous Transfer System, Arthrex, Naples, FL)
Positioning
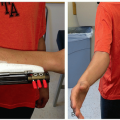
Supine position (Figure 11.2)
Surgical limb supported by small arm board or hand table with nonsterile tourniquet
Ipsilateral lower limb prepped and draped with nonsterile tourniquet for possible osteochondral grafting
Surgical Approach
Arthroscopy
Suspend the limb with the shoulder abducted 90°, elbow flexed 90°, and forearm in neutral rotation
Insufflate the joint with 10 to 20 mL saline via a direct posteriolateral “soft spot” portal
Create anteromedial viewing portal, 2 to 3 cm proximal to the medial epicondyle and just anterior to medial intermuscular septum
Arthroscopic survey to assess the radial head, capitellum, and ulnohumeral joint
With both portals, be aware and protective of ulnar, median and radial nerves as they in close proximity
If loose bodies are encountered, they may be removed through an anterolateral working portal
If desired, posterior compartment may be viewed via a posterolateral portal with establishment of a direct, triceps-splitting posterior working portal for posterior loose body removal
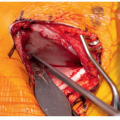
Arthrotomy
The limb is taken out of suspension, and the elbow is hyperflexed
Based upon intraoperative assessment of OCD lesion, decision is made regarding microfracture, fixation, or osteochondral grafting
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree