Phenotypic severity dictates the timing and type of surgical intervention required. Mandibular distraction in children without respiratory and feeding difficulties remains controversial with regard to long-term mandibular growth outcomes and reducing surgical burden. Early mandibular distraction does not obviate secondary orthognathic surgery at skeletal maturity; it provides improved functional, aesthetic, and psychosocial outcomes, at least in the short term. Costochondral rib grafting for Pruzansky type IIB and III mandibles can produce reliable results, especially when combined with subsequent mandibular distraction. Secondary 2-jaw orthognathic surgery plus genioplasty at skeletal maturity benefits from improved bone volume from prior mandibular distraction.
Key points
- •
Phenotypic severity dictates the timing and type of surgical intervention required.
- •
Mandibular distraction in children without respiratory and feeding difficulties remains controversial with regard to long-term mandibular growth outcomes and reducing surgical burden.
- •
Early mandibular distraction does not obviate secondary orthognathic surgery at skeletal maturity; it provides improved functional, aesthetic, and psychosocial outcomes, at least in the short term.
- •
Costochondral rib grafting for Pruzansky type IIB and III mandibles can produce reliable results, especially when combined with subsequent mandibular distraction.
- •
Secondary 2-jaw orthognathic surgery plus genioplasty at skeletal maturity benefits from improved bone volume from prior mandibular distraction.
Surgical history
The historical management of bony and soft tissue hemifacial microsomia (HFM) largely paralleled advances in reconstructive surgery: bone grafts, osteotomies, dermis-fat grafts, locoregional flaps, microvascular free flaps, and autologous fat grafting. Maxillomandibular osteotomies and autologous bone grafts remained the gold standard for mandibular reconstruction during the 1980s. , However, the introduction of distraction osteogenesis represented a paradigm shift in the treatment of mandibular hypoplasia. Initially described by Ilizarov and colleagues for the endochondral bones of the extremities and applied to the craniofacial skeleton by Snyder and colleagues, mandibular distraction osteogenesis (MDO) was popularized in 1992 by McCarthy and colleagues at New York University. Using an external fixator–like device secured to the mandible with transcutaneous pins and a Risdon approach, McCarthy and colleagues showed mandibular bony lengthening of 18 to 24 mm in a series of 4 patients, obviating autologous bone grafts, blood transfusion, and/or maxillomandibular fixation. MDO provided several advantages compared with existing modalities, including a simpler technique, decreased morbidity (eg, infection blood loss, operative time), and ability to lengthen the mandible at a younger age. Compared with bone grafting, successful MDO vertically lengthens the mandible, improves the quality of bone stock, improves soft tissue asymmetry, allows improved vector control of bony regenerate, and may be associated with less relapse.
Treatment algorithm
The reconstructive requirements of patients with HFM relate to anatomic and functional deficiencies in the setting of patient age. The observed composite soft tissue and bony deformities may lead to impaired respiratory, otologic, masticatory, speech, and psychosocial well-being, necessitating early multidisciplinary treatment beyond simple “bone carpentry.” This article focuses on the skeletal deformity of the jaws. However, augmentation of the soft tissue deficiency warrants a brief discussion. At the time of operative skeletal intervention (eg, mandibular distraction, rib grafting, and orthognathic surgery), the authors perform fat grafting ad seriatim, which significantly improves the soft tissues over time and frequently obviates more complex augmentation procedures such as free tissue transfers. The treatment of mandibular hypoplasia, specifically, depends on age and severity. Age can be divided into 3 periods: (1) neonatal, (2) school age, and (3) skeletal maturity. Severity is determined by a dichotomized Pruzansky classification: (1) type I/IIA (mild/moderate) versus (2) type IIB/III (severe).
During the neonatal period, which is defined as the first 28 days after birth, respiratory and feeding concerns dictate early interventions. Obstructive sleep apnea and other respiratory deficiencies secondary to severe mandibular hypoplasia, micrognathia, and glossoptosis may require tracheostomy, although neonatal MDO may obviate this morbid procedure if respiratory insufficiency is limited to a single-level obstruction.
The timing of surgical treatment remains controversial for patients without severe mandibular hypoplasia and consequent respiratory insufficiency beyond the neonatal period. Is early surgical intervention deleterious in the context of craniofacial growth and overall appearance? Does early intervention in the form of MDO, which is associated with decreased operative time and invasiveness compared with major osteotomies, prevent further deformity or impair otherwise normal growth? Poswillo and Obwegeser argued against osteotomies before skeletal maturity because they thought early intervention interfered with the underlying functional matrix and consequently deterred craniofacial growth. Instead, Obwegeser advocated rib graft reconstruction of the temporomandibular joint (TMJ) and zygomatic arch and definitive orthognathic correction consisting of Le Fort 1 and bilateral sagittal split osteotomy (BSSO) with genioplasty during adulthood. Proponents of early intervention include Dingman and Grabb, who reconstructed the hypoplastic ramus using metatarsal bone graft. Converse and colleagues similarly advocated staged, early treatment during mixed dentition in order to avoid difficulties with soft tissue hypoplasia in adulthood and to achieve greater benefit from surgical-orthodontic therapy during periods of growth. Munro and colleagues, Murray and colleagues, and Lauritzen and colleagues similarly recommended childhood osteotomies and costochondral rib grafting with subsequent growth of the rib-mandible constructs. In general, surgical intervention for mild mandibular hypoplasia (ie, Pruzansky type I) can be successfully managed with orthodontics during childhood. Alternatively, more severe Pruzansky type I and IIA phenotypes are associated with occlusal cants and facial asymmetries that have the potential of worsening during the period of mixed dentition and may benefit from early surgical intervention. McCarthy and coworkers’ experience with early MDO during childhood for patients with mild to moderate unilateral HFM (ie, Pruzansky type I and IIA) showed efficacy in achieving satisfactory outcomes through adhering to proper vector selection, overcorrection, and close orthodontic managment. The vector of distraction depends on mandibular morphology, with overall goals to lengthen the deficient ramus, upright the condyle, and create a gonial angle; type IIA mandibles characterized by deficient ramal height benefit from a vertical vector of distraction, whereas type IIB mandibles characterized by vertical and horizontal ramal and body deficiencies benefit from a more oblique vector of distraction. , The authors have adopted a similar philosophy consisting of early MDO for patients with mild to moderate mandibular hypoplasia and facial asymmetry without respiratory insufficiency, which are discussed later in detail.
For patients with severe mandibular hypoplasia (type IIB/III) during childhood, the authors recommend costochondral rib reconstruction with or without subsequent mandibular distraction of the construct. In addition, we recommend conventional maxillomandibular orthognathic surgery in skeletally mature patients with HFM regardless of prior surgical interventions.
Neonatal mandibular distraction
In cases of mild to moderate respiratory insufficiency associated with HFM mandibular hypoplasia, conservative measures that are similarly used for the treatment of Robin sequence, such as prone positioning, supplemental oxygen, nasopharyngeal airways, and continuous positive airway pressure, may provide adequate symptomatic relief. , , In more severe cases of unilateral or bilateral hypoplasia requiring intubation, MDO may prevent progression to tracheostomy. Although neonatal distraction is discussed in detail elsewhere in this issue, this article briefly comments on relevant principles.
Our preferred technique for MDO independent of age involves an osteotomy (vertical or oblique >horizontal vector) of 1 or both sides of the deficient mandible with the application of an internal, semiburied distractor through a Risdon approach. Advantages of internal devices include decreased visibility, cutaneous scarring, and likelihood of trauma and infection. Advantages of external devices include increased ability to mold the regenerate and alter the distraction vector after osteotomy, and precise placement of distracting pins without wide periosteum undermining in the setting of a severely hypoplastic mandible. We typically favor a vector oblique to the maxillary occlusal plane in order to obtain expansion in both the vertical and sagittal dimensions, although the exact vector orientation depends on the underlying mandibular morphology. The semiburied distractor, which is secured with bicortical screws, typically exits the skin near the retroauricular region. A piezoelectric saw is used to perform a near-complete osteotomy distal to the developing tooth roots. While considering the inferior alveolar nerve, a full corticotomy over the buccal surface of the mandible and superior and inferior surfaces of the lingual mandible completes the osteotomy. The distractor device is then activated for several millimeters to ensure advancement without interference. An osteotome may be used to carefully separate adjoining bony edges while preserving the nerve. Once confirming a complete osteotomy, the engaged bony edges are opposed and the incision closed in layers with resorbable suture.
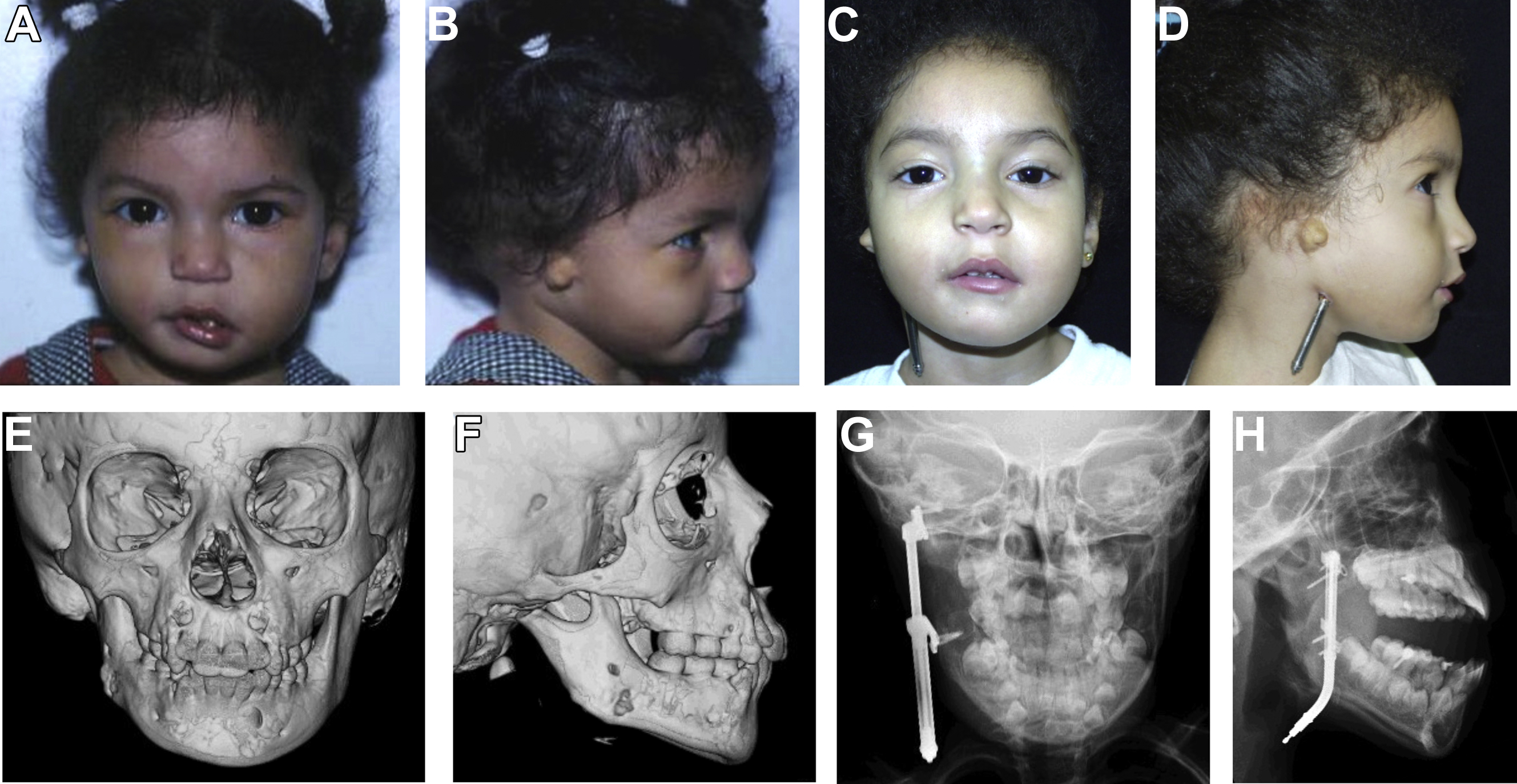
After a latency period of approximately 1 to 2 days in neonates, distraction during the activation phase proceeds at a rate of 1 mm/d (potentially 2 mm/d) to avoid premature consolidation and to reduce the length of endotracheal intubation. Clinical end points for the activation phase in patients with unilateral HFM include (1) overcorrection of the occlusal plane, (2) inferior displacement of the ipsilateral oral commissure, and (3) and movement of the chin point beyond the midline. In neonates with bilateral HFM, activation continues until the mandibular anterior teeth are anterior to the maxillary anterior teeth (ie, class III malocclusion–like appearance). An additional criterion for cessation of distraction in respiratory-compromised neonates includes evidence of improved retroglossal airspace on lateral radiograph or endoscopy. Adherence to these principles has led to successful extubation and improved maxillomandibular relation in 92% to 100% of patients ( Fig. 1 ).
Mild or moderate mandibular hypoplasia
Perhaps the most controversial decision in the surgical management HFM relates to patients with mild or moderate mandibular hypoplasia without functional compromise. Early on, MDO improves facial appearance by lengthening the mandible and expanding the overlying soft tissues; however, the correction may be prone to relapse and require future interventions. , , , Whether the distracted mandible fails to grow or the deformity relapses, the outcome nevertheless results in the need for orthognathic correction at skeletal maturity. Moreover, the potential benefit must be considered in the context of potential complications, including tooth bud injury, facial nerve injury, premature bony consolidation, and hardware failure. ,
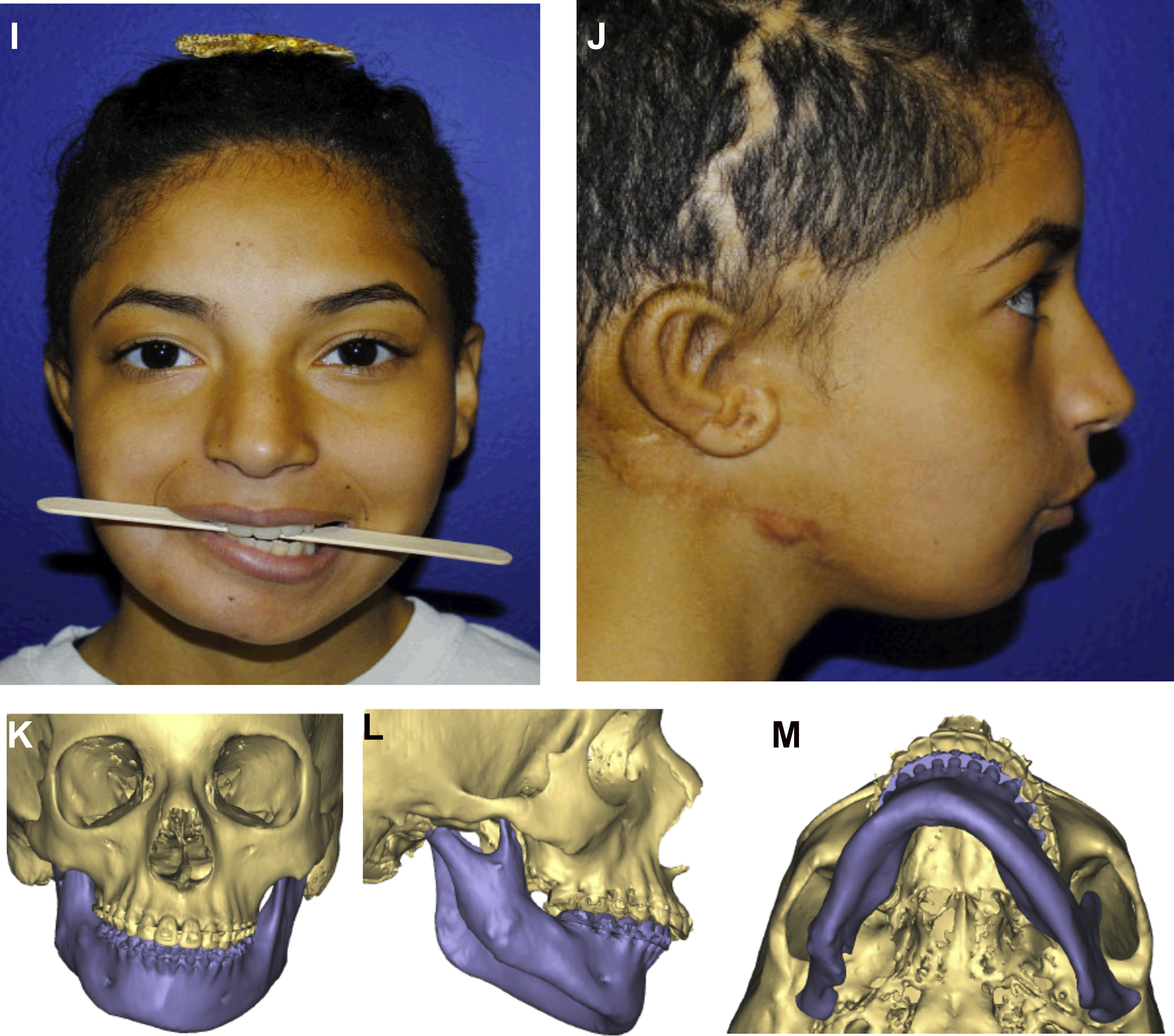
Our preferred technique for early unilateral MDO largely mirrors the technique described for neonatal MDO, but with a few caveats. Our experience with early MDO highlights the importance of comprehensive orthodontic care and orthodontic splint therapy to negate the effects of masseter muscle contraction on the regenerate, control maxillary dentoalveolar elongation, and subsequent preservation of mandibular regenerate length and volume. Predistraction orthodontic management may involve removal of dental compensations, expansion of the maxillary arch width, maintenance of the mandibular lingual arch, and forced eruption of molar tooth buds away from planned mandibular osteotomies. For patients undergoing early MDO, the procedure inherently generates a posterior open bite on the affected side. Intraoperatively, we secure orthodontic bone anchors on the hypoplastic mandible. Intermaxillary guiding elastics can be used during the active phase of distraction to mold the generate and adjust the distraction vector to achieve a planned occlusion. During the activation and consolidation phases, the use of elastics further guides vertical growth of the maxilla. Following removal of the distractor, the patient is fitted with a custom splint to maintain the surgically created open bite. Gradual burring down of the splint allows for selective eruption and growth of the maxillary dentition and alveolar bone closing the open bite and maintaining the mandibular correction. Our anecdotal experience suggests overcorrection can further level the maxillary dental arch and provide an improved functional and aesthetic outcome. These properly positioned orthodontic devices and splints not only preserve regenerate volume but may also promote regenerate and maxillary growth. Judicious care coordination with the orthodontist should not be underemphasized.
In order to lengthen the deficient mandibular ramus, we prefer a more vertical or oblique vector of distraction. When using a more vertical vector (ie, horizontal osteotomy in line with maxillary occlusal plane), the proximal segment distraction force generates counterclockwise rotation about the condyle and TMJ impaction, leading to generalized joint dysmorphology, including flattening, hypertrophy, ankylosis, and/or dislocation. Some investigators even promote coronoidectomy at the time of MDO to prevent these untoward consequences of counterclockwise rotation and superior displacement. There is significant distraction force wasted in rotating the proximal segment cephalad before gaining the desired vertical height of the deficient ramus in the caudal direction. Since 2012, we have been using a check plate attached to the coronoid to engage the zygomatic arch during active distraction in order to focus the vertical/oblique distraction force downward onto the mandibular ramus instead of upward toward the TMJ and cranial base. Our computed tomography (CT) data show improved TMJ morphology when using the check plate. This modification to traditional MDO with a vertical/oblique vector prevents impaction of the TMJ into the cranial base, prevents cephalic rotation of the proximal segment about the TMJ, and optimizes the position of the subsequent regenerate.
McCarthy and colleagues enumerated several critical lessons in their 22-year review of early MDO in patients younger than 10 years of age with Pruzansky type I/IIA mandibles undergoing unilateral MDO. In a subjective photographic assessment of satisfactory versus unsatisfactory outcomes of patients at skeletal maturity with history of MDO before 10 years of age, the investigators found overcorrection from the midline (>44%) and younger age at time of initial distraction (4.7 vs 7.5 years) to significantly correlate with improved outcomes (our own experiences suggest patients undergoing MDO before 3 years of age benefit from spontaneous descent of the ipsilateral maxillary dentoalveolus with distraction). Moreover, the use of comprehensive orthodontia including postoperative splints further aided successful distraction. In a retrospective outcome analysis of vector selection and overcorrection in MDO, the New York group suggested the oblique vector offered an ideal balance between the horizontal and vertical vectors by simultaneously lengthening the ramus and translating the gonion. They concluded that, although a subset of patients who undergo early MDO require secondary surgery (eg, orthognathic correction) at skeletal maturity, they often maintain satisfactory outcomes if initially overcorrected despite a varying degree of relapse, and invariably benefit from improved appearance-related psychosocial development during childhood. Moreover, patients undergoing early MDO benefit from increased bone stock for secondary orthognathic surgery.
Our experience with early MDO largely mirrors these McCarthy and colleagues’ data. Zhang and colleagues compared the need for secondary orthognathic correction in skeletally mature patients with HFM at the Children’s Hospital of Philadelphia who either did or did not undergo early MDO over a 25-year study period. The 2 cohorts were matched according to Pruzansky grade, with patients in both cohorts showing similar hypoplasia grades. The mean age at time of MDO was ∼9 years, older than the recommended age per the McCarthy and colleagues data, although patient age at time of distraction did not ultimately correlate to need for orthognathic correction. Approximately 35% of these patients outgrew their initial corrections and underwent repeat MDO at ∼10.6 years of age. Of the patients who underwent early costochondral rib grafting only, all 3 out of 3 required secondary orthognathic correction, suggesting that rib growth may not mirror the unaffected side, resulting in recurrence of asymmetry. Interestingly, degree of mandibular deformity as determined by Pruzansky grade did not correlate with need for orthognathic correction in patients who did or did not undergo early MDO. Importantly, the incidence of secondary orthognathic surgery at skeletal maturity did not differ between the 2 cohorts, suggesting early MDO provides functional, aesthetic, and psychosocial benefits, but does not obviate later orthognathic correction in every patient to further refine facial asymmetry. In addition, the enhanced body image and psychosocial impact of a developing child with improved facial asymmetry cannot be overstated, although validated quality-of-life studies are lacking.
Despite these long-term data from high-volume centers, there lacks consensus among practitioners regarding the efficacy of early MDO. In a prospective, longitudinal study, Meazzini and colleagues reported a near-100% recurrence rate of mandibular asymmetry occurring 5.8 years after early MDO. In a controversial review of long-term stability after early MDO published in 2009, Mommaerts and coworkers critically evaluated the existing literature and concluded: (1) study designs were poor and failed to stratify results based on Pruzansky type; (2) there was no validation of measurements to determine facial symmetry; (3) 0 of 13 studies showed predictable, long-term stability following early MDO, but instead showed significant relapse; (4) repeated MDO was necessary to improve recurrent facial asymmetry; (5) early MDO did not reduce rates of secondary maxillary deformity; and (6) repeat MDO represents a costlier endeavor than single-stage orthognathic surgery at time of skeletal maturity. , The investigators concluded that, “there is no convincing evidence supporting the effectiveness of early mandible osteodistraction in hemifacial microsomia patients. Patients need to be informed that additional distraction procedures or definitive secondary surgery at maturity most likely will be required.”
Since the publication of Mommaerts and coworkers’ review 11 years ago, long-term outcomes data continue to suggest that most patients with HFM require orthognathic correction at the time of skeletal maturity independent of early intervention performed. Ascenço and colleagues reported a 90% recurrence rate of facial asymmetry following unilateral MDO in 33 patients, who subsequently required a referral for orthognathic correction ∼3.8 years from time of intervention. Suh and colleagues showed relapse and return to baseline asymmetry in 26 patients over an 11-year follow-up period; however, the investigators failed to overcorrect and accepted leveling of the oral commissure as a clinical end point during activation. In a systematic review by Pluijmers and colleagues, the investigators suggested surgical outcomes in HFM to be patient dependent and not treatment specific, although long-term outcomes lacked radiographic data related to relapse, and clinical end points of correction again failed to emulate those suggested by McCarthy and colleagues. Recent multi-institutional data from 3 large European craniofacial centers suggest that patients undergoing surgical interventions targeting the mandible earlier in life undergo significantly more procedures to correct asymmetry later on, independent of Pruzansky type.
Despite these conflicting reports, the authors believe early MDO is a critical tool to generate bone (and to a lesser extent soft tissue) in order to improve facial asymmetry, at least in the short term. Early distraction does not eliminate the need for definitive orthognathic surgery at skeletal maturity or produce a lesser maxillary deformity; instead, we argue that MDO offers an opportunity to generate new bone, lengthen a hypoplastic mandible, and improve facial asymmetry. Clinical end points such as overcorrection of the pogonion beyond the craniofacial midline and inferior displacement of the affected side oral commissure compared with the unaffected side are critical factors leading to lasting results. Comprehensive presurgical and postsurgical treatment with an orthodontist can not only manage maxillary dental eruption but also maintain an open posterior bite using splints to allow for maxillary growth and eventual closure of the posterior gap. When adhering to these principles of early distraction, we believe there may be patients who need orthognathic surgery to a lesser extent at skeletal maturity. The need to perform additional surgery in a growing facial deformity does not represent a failure; instead, secondary orthognathic surgery simply represents an opportunity to further refine form and function in the patients with evolving HFM.
Severe mandibular hypoplasia
The management of severe mandibular hypoplasia characterized by Pruzansky grade IIB and/or III mandibles is more straightforward. Sir Harold Gillies first described the autologous costochondral rib graft for TMJ reconstruction in 1920. The authors believe costochondral rib grafting remains the gold standard treatment in this patient population, although multiple other autologous grafts have been attempted, including the clavicle and sternoclavicular joint, fibula, iliac bone, and metatarsal bone. , , We use costochondral rib graft when there is ramus deficiency and prefer to use the fibula when there is ramus and body deficiency. However, various investigators report unpredictability with costochondral rib grafting for mandibular and TMJ reconstruction, citing graft overgrowth, lack of growth, graft resorption, and ankylosis. We have previously published our technique for rib grafting, which is summarized here.
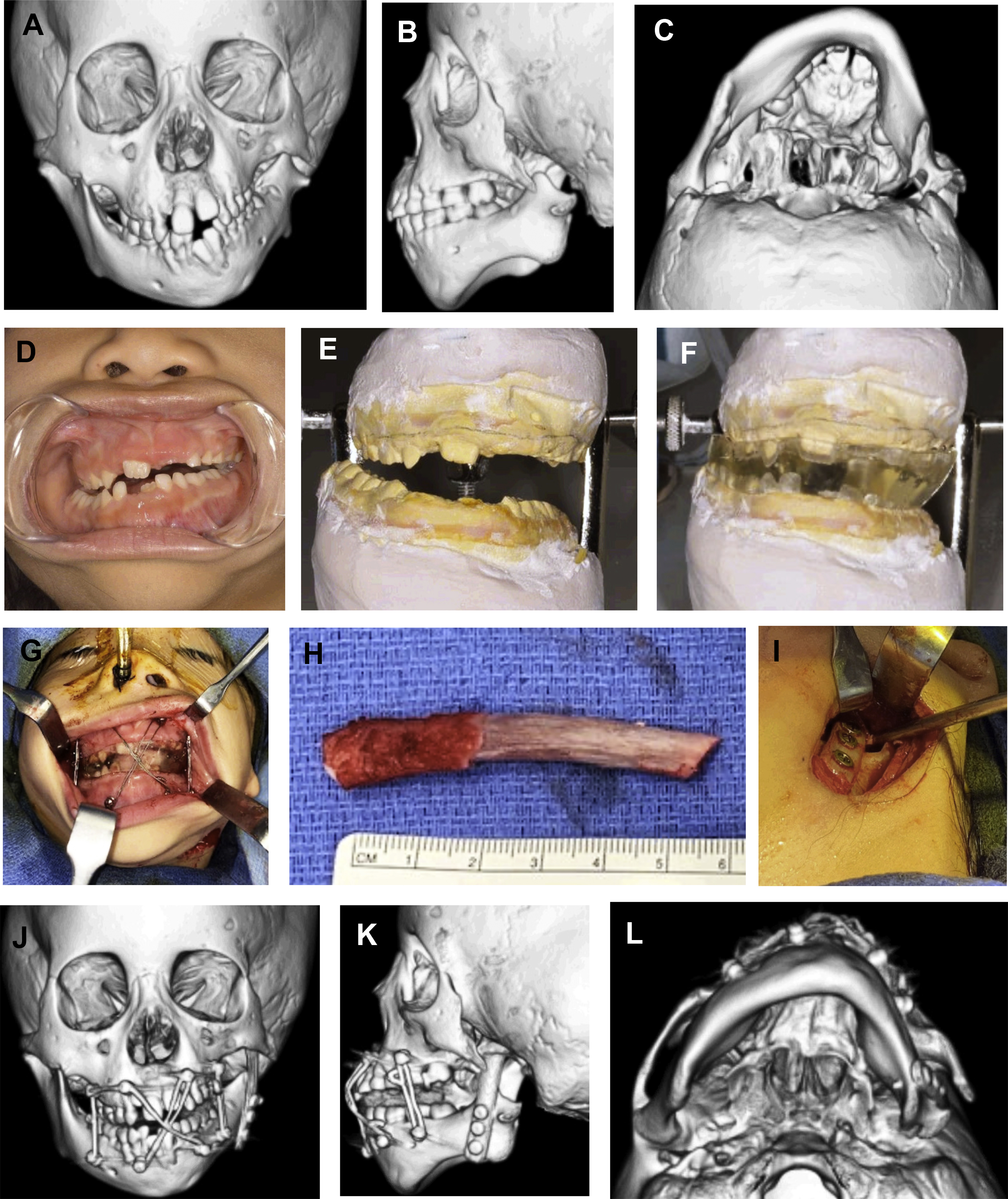
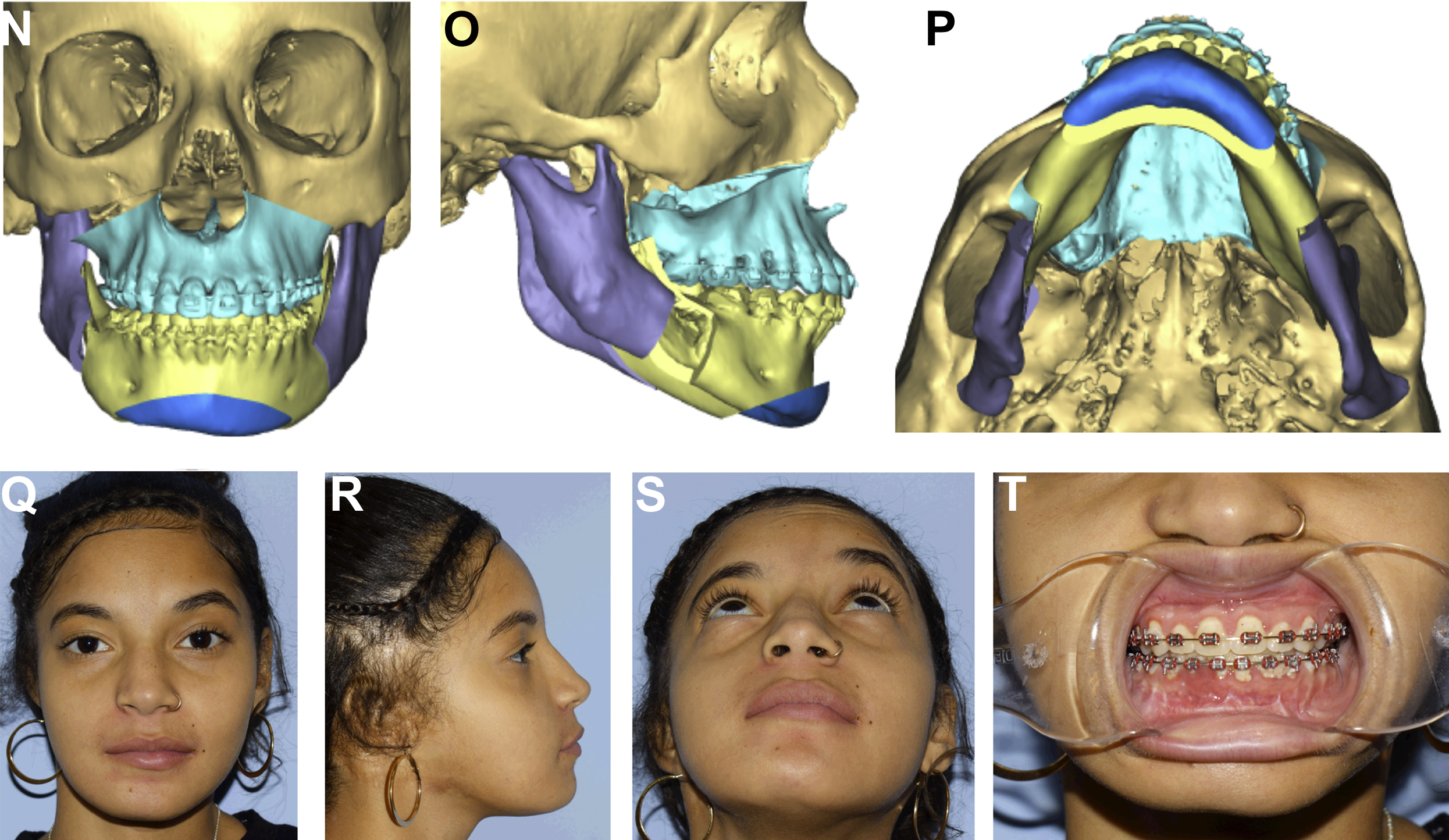
The goals of costochondral grafting for reconstruction in children with Pruzansky type IIB and III mandibles include (1) reconstruction of a new ramus and pseudocondyle; (2) generation of a pseudarthrosis by placing the rib graft in a pocket abutting the cranial base; (3) alignment of the maxillomandibular dental midlines with the midsagittal plane; and (4) correction without overcorrection of the mandibular cant, consequently restoring facial asymmetry with the assumption of ongoing rib growth. Surgical management begins in the orthodontic clinic with preoperative fabrication of an occlusal splint based on predicted final mandibular position and large posterior open bite. Alternatively, the splint may be created intraoperatively using polymethylmethacrylate or virtually planned using three-dimensional CT technology. We have previously described our technique for costochondral rib grafting, which broadly consists of (1) rib harvest, (2) neofossa creation, and (3) postoperative orthodontic splint therapy ( Fig. 2 ).