Minimally Invasive Techniques for Foot Deformity Correction
Susan T. Mahan
Collin J. May
Insertion of Subtalar Extra-Articular Screw Arthroereisis for Treatment of Flexible Flatfoot in Children
Operative indications: Symptomatic flexible pes planovalgus and ankle pronation in an ambulatory child that has been recalcitrant to conservative methods of treatment (Figure 28.1).
Need dorsiflexion at least past neutral (ideally >20° past neutral when the foot is supinated and knee is extended)
Challenge the child preoperatively to obtain sufficient dorsiflexion using daily stretching and nighttime dorsiflexion boot
If not achieved, then should add Achilles lengthening (typically Vulpius type)
Age range in normal kids is typically 9 to 17 years
Most common age in normal children is 12 years
Ambulatory neuromuscular children with very severe pes planus can be treated as young as 6 years of age (almost always need Vulpius)
Equipment: Synthes 6.5-mm cannulated partially threaded screw (typically 30 mm for about 90% of patients). In very young (<10 years, or very small feet), the 4.5-mm cannulated system can be used. Smooth Kirschner wire (K-wire) (3/32 when using the 6.5-mm cannulated system). Schnitt or snap. Fluoroscopy.
Positioning: Supine with a bump under the hip so the leg sits naturally with patella forward. Tourniquet on involved limb. Sural nerve block.
Surgical Approach: The subtalar extra-articular screw arthroereisis (SESA) screw goes in through a small <1 cm incision just over the sinus tarsi on the anterolateral aspect of the foot. The SESA screw will go vertically in the calcaneus just distal to the isthmus; properly placed, it will impinge on the lateral talar process and lateral talus and prevent the talus from hyperpronation.
Techniques in Steps
If a Vulpius or other type of Achilles lengthening needs to be done, then that should be done first
Leg position during insertion
Very important!
Foot in neutral dorsiflexion and maximum supination (Figure 28.2)
Important to have patella forward (Figure 28.3)
Bump under the ankle/foot
Surgical incision
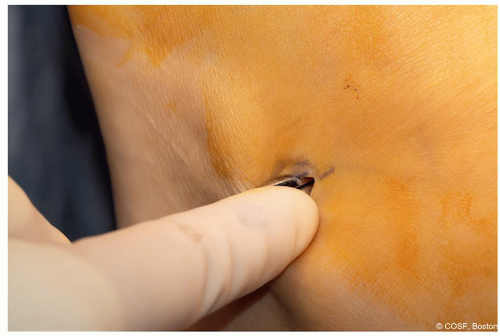
5 to 8 mm lateral foot over sinus tarsi in Langer lines (Figure 28.4)
Spread down with snap or scissors to the sinus tarsi (Figure 28.5). If in correct place, will have 1 in of snap/scissors deep in the space (Figure 28.6)
Screw insertion
Large K-wire (3/32 fits through the 6.5-mm screw) placed first (Figure 28.7)
Starting point
Medial third of the calcaneal cuboid joint—about 1 cm medial from lateral edge of calcaneus
Just distal to the calcaneal isthmus

Figure 28-4 ▪ Surgical incision is 5 to 8 mm in Langer lines on the lateral foot over sinus tarsi. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
Trajectory
Press against the fibula with the wire
Aim a little anteriorly 15° to 20° and slightly medially—this angle is slightly forgiving if not perfect
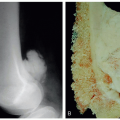
Check fluoroscopy to confirm position of the guide pin (Figures 28.8 and 28.9)
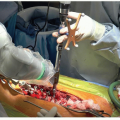
Overdrill—just the near cortex—typically cannulated drill for 6.5-mm system (Figure 28.10)
Screw insertion (Figure 28.11)
Usually, Synthes 6.5-mm cannulated partially threaded screw
Length 3.0 cm in most all feet 90% to 95%
3.5 in bigger feet
2.5 in smaller feet
Confirm position of screw on fluoroscopy—anteroposterior (AP) and lateral (Figures 28.12 and 28.13)
Confirm clinically (Figure 28.14)
Weakest part of the procedure is how deep to put in the screw
Too proud will be undercorrected—needs to tuck under talus
Too deep will also undercorrect
When properly placed, can see screw head just under the skin level
Impinges on lateral talar process (cannot see this directly though)
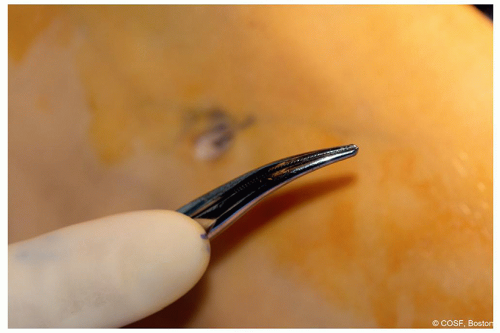
Figure 28-6 ▪ Showing the amount of snap in the incision, a full inch. (Courtesy of Children’s Orthopaedic Surgery Foundation.)

Figure 28-7 ▪ Guide pin entry into the calcaneus—proper position. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
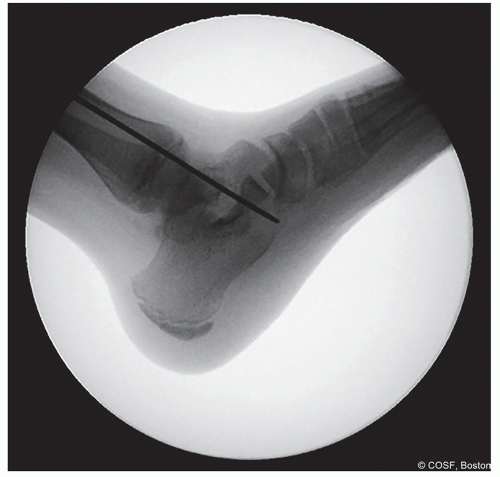
Figure 28-8 ▪ Lateral view fluoroscopy showing the guide pin in the proper location. (Courtesy of Children’s Orthopaedic Surgery Foundation.)

Figure 28-9 ▪ Anteroposterior view fluoroscopy showing the guide pin in the proper location. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
Closure
Deep stitch
Skin
If no Achilles lengthening, then place soft dressing
If Vulpius done, then placed in solid short leg cast and may weight bearing in cast until follow-up
Postoperative Care
If no Vulpius and in soft dressing,
Non-weight bearing 3 days
First day post-op, patients are instructed to do 100 dorsiflexion eversion exercises
Follow-up day 3 to 5 for wound check
Exercises are also started
Skier exercises with feet apart and shift weight from one foot to the other—must have plantargrade stance (Figure 28.15)
Cannot weight bearing until 300 skier exercises

Figure 28-10 ▪ Overdrill the near cortex only, try to keep the pin in place during drill removal, and be careful of the skin! (Courtesy of Children’s Orthopaedic Surgery Foundation.)

Figure 28-11 ▪ Then insert the screw over the guide pin. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
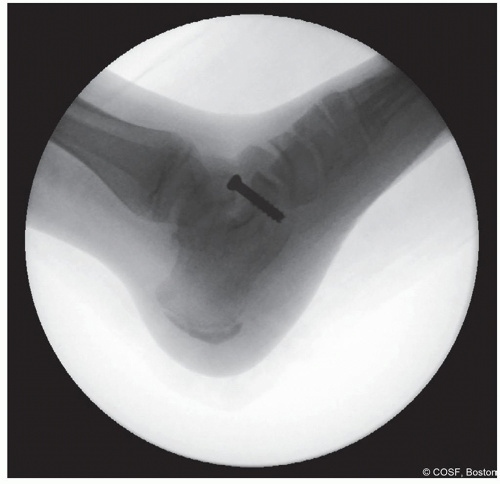
Figure 28-12 ▪ Lateral view fluoroscopy showing the screw in the proper location. (Courtesy of Children’s Orthopaedic Surgery Foundation.)

Figure 28-13 ▪ Anteroposterior view fluoroscopy showing the screw in the proper location. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access