Angle fractures are the most common among the mandibular fractures. History and physical examination are crucial in guiding time course and specifics of management. Computed tomography (CT) has become the gold standard for diagnosis of mandible fractures, offering advantages for both surgical planning and assessing dental involvement. Currently the use of a single monocortical plate with the Champy technique for osteosynthesis is used preferentially for noncomminuted fractures of the mandibular angle. Other load-sharing options for plating include strut plates, malleable plates, and geometric or 3D plates. Load-bearing options remain viable for comminuted fractures or other complex circumstances.
Key points
- •
For uncomplicated mandibular angle fractures, a single monocortical miniplate on the lateral border of the mandible has the lowest complication rate reported.
- •
Complicated, comminuted fractures or fractures that have bone loss either from atrophy or from tooth loss may require more rigid fixation or load-bearing fixation.
- •
Strut plates and 3D plates may resist torsional forces better, and their use is evolving as a treatment for angle fractures.
Introduction
Angle fractures are the most common fractures of the mandible. Recent reports suggest about 30% of mandible fractures occur at the angle. However, the definition of the mandibular “angle” itself varies. In general, the area where the mandible body and ramus come together is referred to as the angle. The third molars arise in this area, if present, and may be involved in these fractures. Angle fractures occur in a triangular region between the anterior border of the masseter muscle and the posterosuperior insertion of the masseter muscle. The masseter and medial pterygoid muscles attach to the angle of the mandible, and a fracture can cause distraction of the bone fragments.
Presentation of the Patient
Mandibular angle fractures (MAFs) most commonly present in men and are often associated with lateral impact, such as that from a closed fist, as opposed to the anterior impact of a motor vehicle accident. The force required to fracture the mandibular angle should cue providers to look for other injuries. MAF are commonly associated with facial lacerations (32%), orthopedic injuries (20%), neurologic injury (24%), thoracic and abdominal injuries (12%), and cervical spine injuries (2%–10%). ,
If caused by a lateral blow to the jaw, MAFs may commonly be associated with a contralateral fracture including a fracture of the opposite body, opposite condyle, or a parasymphyseal fracture. A fracture through the angle may commonly involve a third molar tooth or tooth socket. In some instances, the third molar itself may be fractured which will have an impact on the strategy of repair.
History and Examination
Substance abuse and interpersonal violence are commonly associated with mandible angle fractures, and this type of historical information should be solicited in the history. Time and date of the fracture should be ascertained to gauge the age of the injury especially because patients who have been intoxicated may not seek care immediately. If the injury was due to a mode of transportation, this information should also be elicited, including the use of seatbelts or airbag deployment, or helmets in the case of bicycles or motorbikes. Past surgical history with special attention to the status of wisdom teeth or cosmetic or functional jaw surgery is also pertinent. The patient should be queried regarding appearance, occlusion, and the presence of sensory nerve deficits.
Physical examination should focus on tenderness, swelling, lip numbness (related to injury of the inferior alveolar nerve), trismus, an intraoral step-off, and the state of the patient’s current dentition. Occlusion is of paramount importance in determining treatment. Evaluating fractures in teeth-bearing regions may identify fractured dentition or may reveal lost or avulsed teeth. A survey of the complete head and neck should be accomplished to be certain that fractures of other facial structures are suspected and identified.
Diagnosis (Imaging)
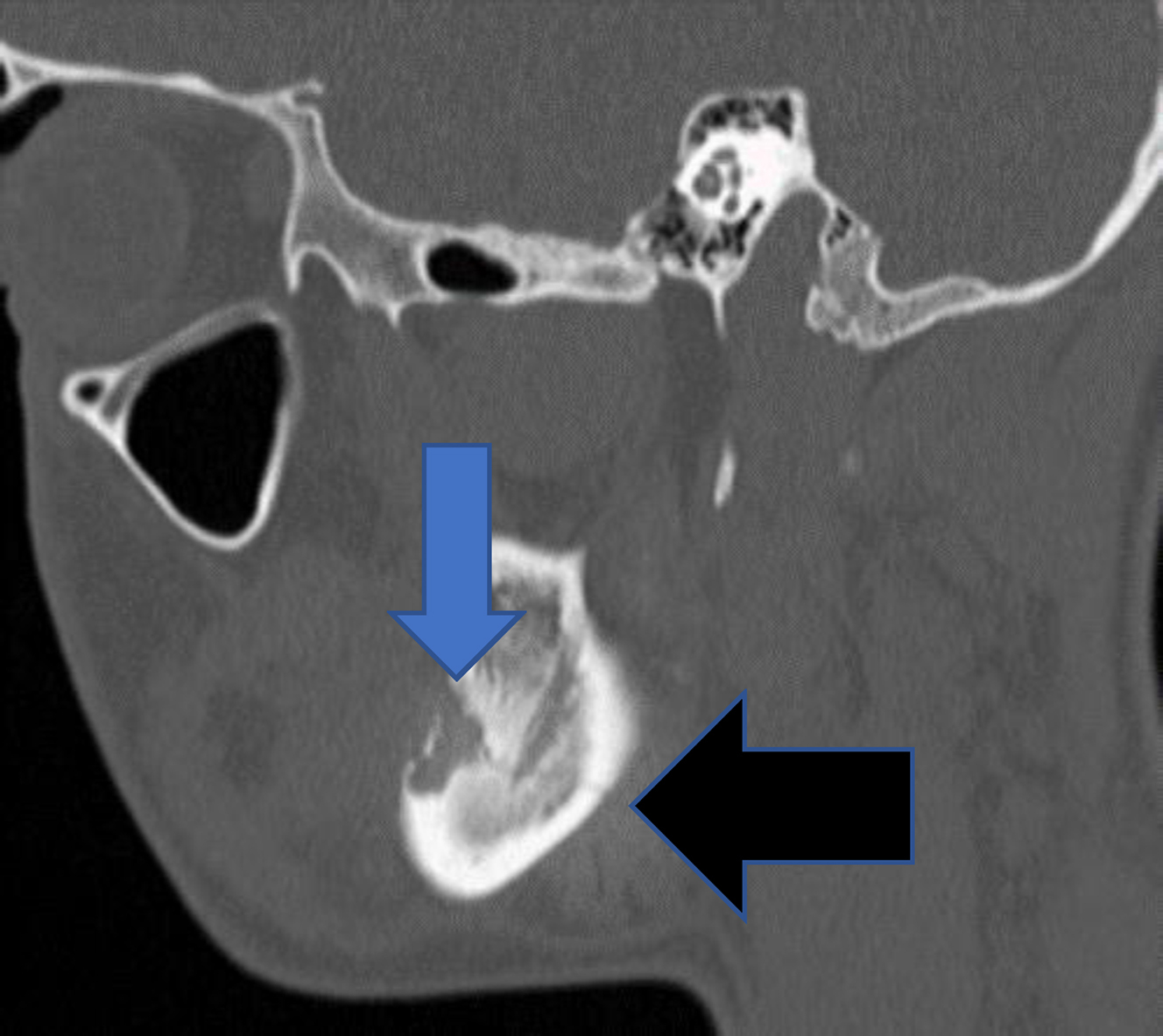
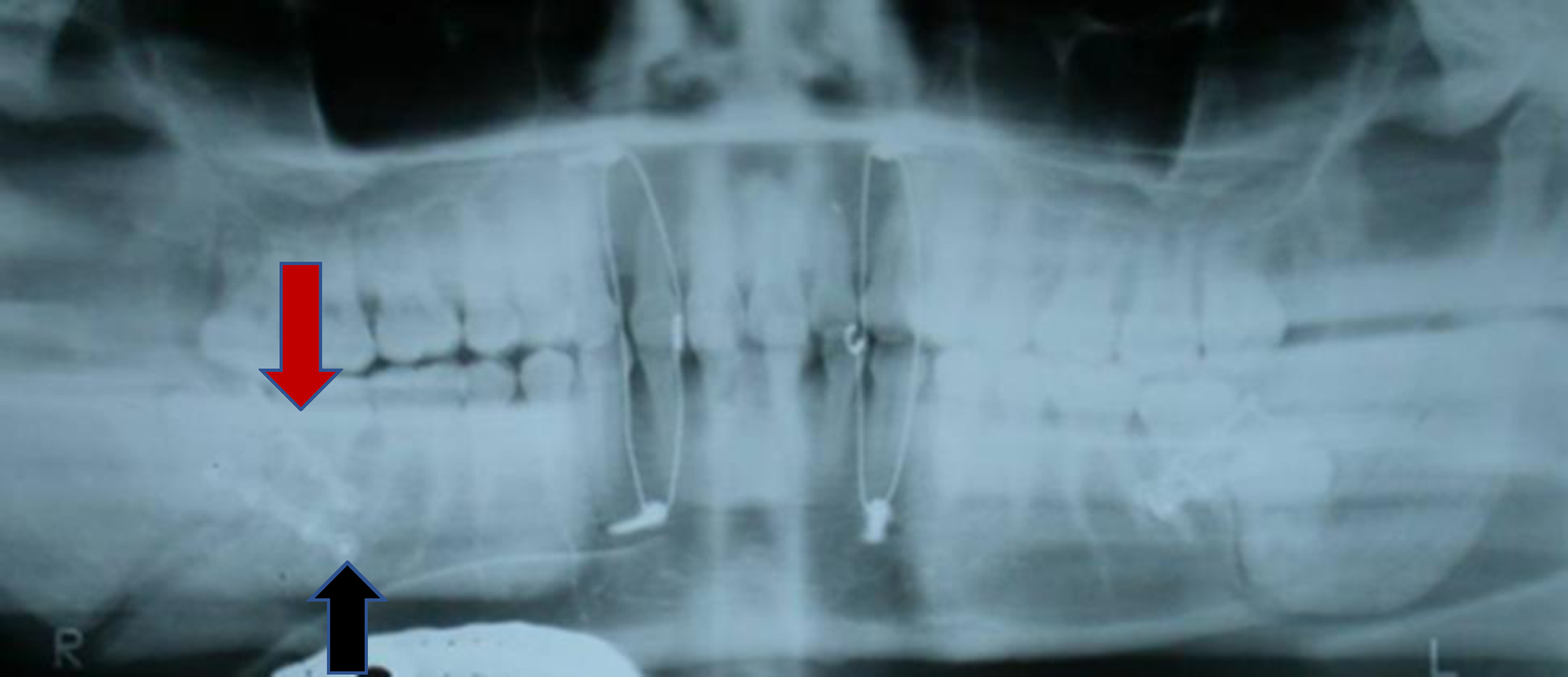
Once a mandible fracture is suspected based on history and physical examination, there are several diagnostic imaging modalities that can be used based on availability. Panorex plain films (orthopantomogram) in combination with a posterior-anterior plain film will provide two views of the mandible which would show an MAF, while a panorex radiograph alone may miss a posterior fracture. However, the equipment to obtain panorex views tends to be of limited availability in the hospital-based emergency room setting, and thus, a mandible series of radiographs or CT have been adopted as the gold standard. A mandible series includes three views: posteroanterior, oblique, and lateral. However, these three views may not clearly visualize the condyles. CT imaging has become the modality of choice and has been shown to have a 100% sensitivity to detect all fractures of the mandible. CT also has the advantage of assessing the involvement of tooth roots in the line of fracture, the presence of severe dental disease, and also screens for other facial fractures. Additionally, CT scans can be used to produce three-dimensional reconstruction which can help with operative planning or the selection of patient-specific plating if necessary.
Treatment
The angle of the mandible has some unique properties. Fractures in this area are less surgically accessible than parasymphyseal or body fractures via a transoral approach. The cross-sectional area of the bone in this area is less than that in more anterior locations, creating less surface contact area to allow stabilization. In addition, fractures in the angle are often posterior to occluding molar teeth, and thus, slight differences in reduction can be tolerated with regard to dental occlusion. Nevertheless, the force generated by the muscles of mastication can reach 60 DN or more at the angle, and any fracture fixation technique must be strong enough to counteract this force.
Antibiotics
Antibiotics given after injury, before surgical repair, have been shown to reduce the rates of infectious complications in facial fractures, including mandibular fractures. However, there does not appear to be evidence in definitive support of postoperative antibiotics once the fractures are reduced. ,
Conservative Treatment
Given the muscular forces on the angle of the mandible, conservative treatment with soft diet or maxillomandibular fixation is often insufficient for treatment of MAFs, even those that are nondisplaced. In addition, the benefit of early function, early mobilization, and rehabilitation is always a goal of operative approaches to mandibular fractures.
Surgical Treatment: Airway Management, Occlusion, Approaches, Surgical Technique
Airway management
Airway management in open reduction, internal fixation of MAFs is often achieved through nasotracheal intubation. This allows the airway to be stabilized without the tube restricting the surgeon’s access. It also allows for the patient to be placed in maxillomandibular fixation (MMF) without issue. If there are concomitant facial fractures limiting access to a nasotracheal intubation, a submental intubation may be considered. In otolaryngology head and neck surgery practices, tracheotomy placement is a familiar technique that controls the airway without risking instrumentation of the nose in circumstances where skull base integrity is in question. Tracheotomy allows unfettered access to the oral cavity and the mandible during surgical repair of facial fractures of all types. Tracheotomy also has the advantage of being useful in the intensive care unit setting and allows for prolonged convalescence. However, a typical isolated mandible fracture without severe concomitant injury seldom requires airway control beyond nasotracheal intubation for the duration of the surgical case. One exception regarding airway control in mandible fractures may be in the circumstance of “bucket handle fractures” of the anterior mandible. This occurs when there are bilateral parasymphyseal fractures that allow collapse of the infraglossal musculature which can cause the base of tongue to relapse with subsequent airway obstruction. This constitutes an airway emergency that will require urgent airway control through intubation or tracheotomy.
Open Reduction, Internal Fixation
Single plate versus two plates
Historically, immobilization of the jaw was the gold standard of care for all mandible fractures. If a fracture was surgically opened, wires were the primary means of fixation. However, the development of plating systems that allow for stabilization of the mandible with or without limited MMF has advantages. Early jaw mobility has been facilitated by internal fixation techniques with subsequent decreased concerns for weight loss, improved patient comfort, less risk of airway compromise, and faster return to active and normal function.
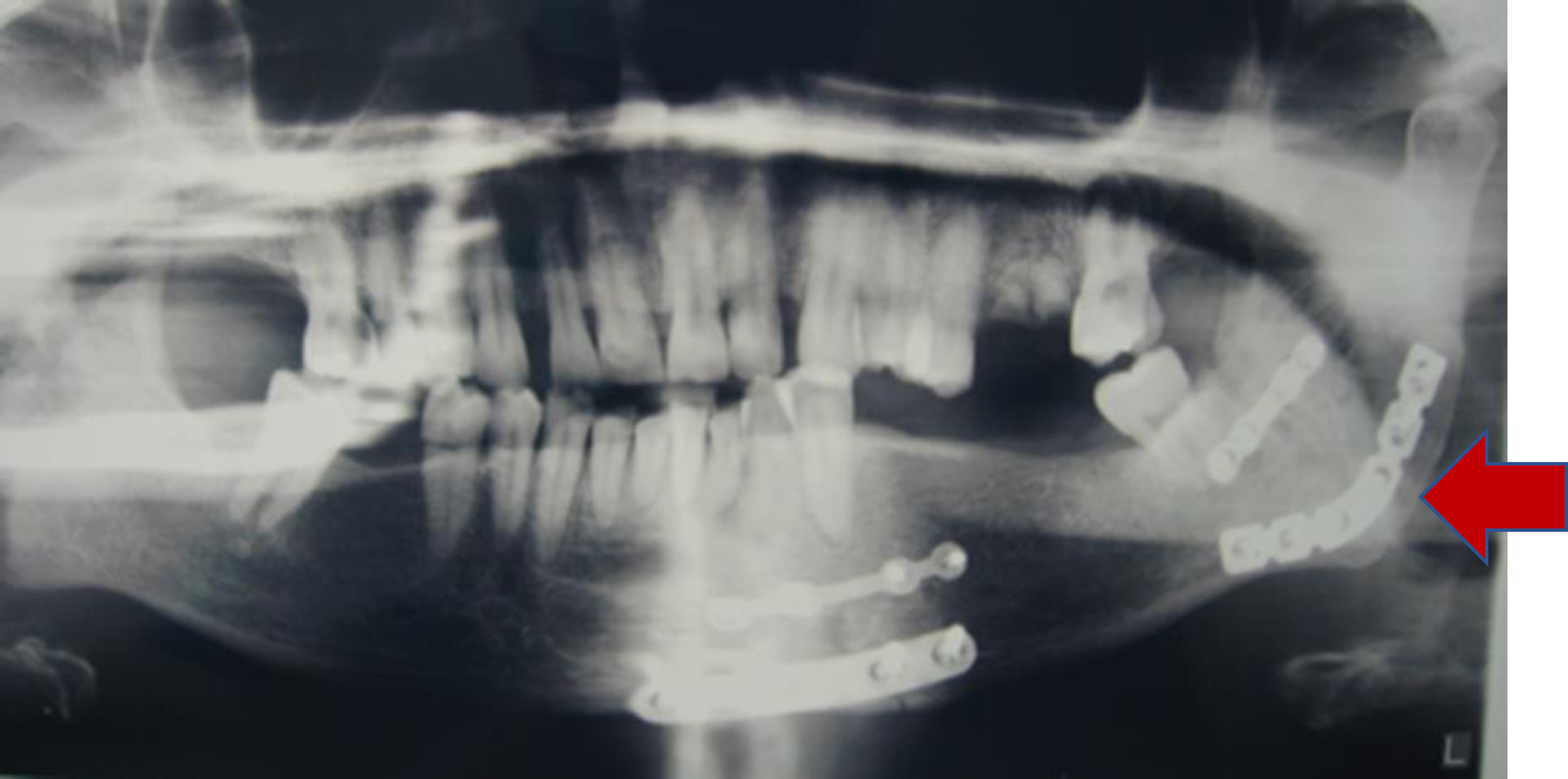
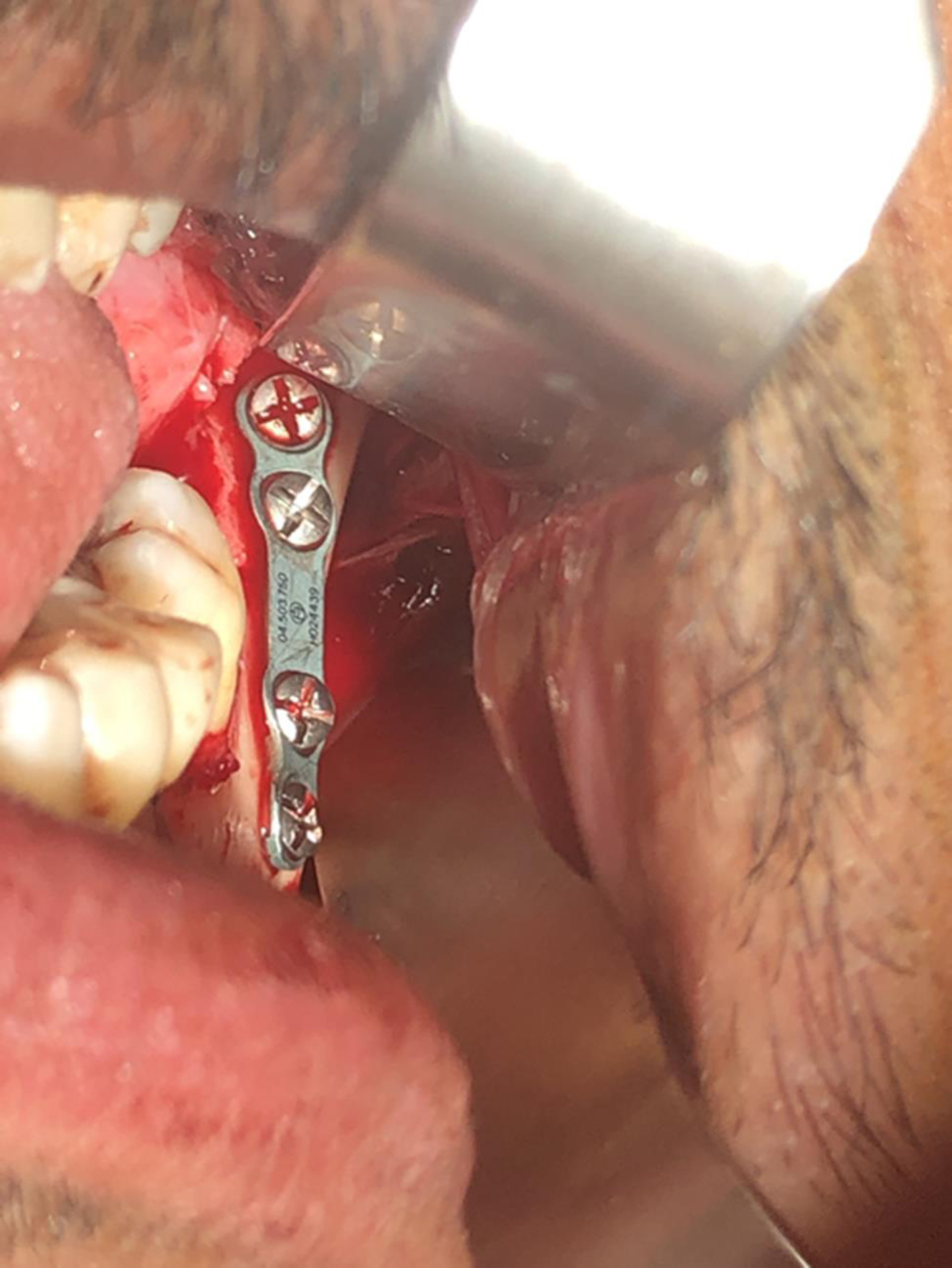
When approaching a MAF, several important factors must be considered. A key determination is the presence or absence of other mandibular fractures. The presence of other fractures may determine the order or technique of the approach. For instance, if there is a nondisplaced contralateral condyle fracture, this circumstance portends the need for guiding elastics, and the use of Erich arch bars will likely be the first step in fracture repair. Angle fractures are usually “retro-occlusal” in that they occur behind the articulated dentition. Therefore, if other fractures are present in the dentate segment of the mandible, it is these “occlusal” fractures that strategically are approached first. Fractures of the mandibular angle are often approached transorally through an incision proximate to the retromolar trigone or through a gingival incision that is described for third molar extraction. In the case of an isolated angle fracture, the fracture is typically completely exposed, and reduction is attempted before placing the patient into maxillomandibular fixation. Yet, maxillomandibular fixation would typically be a prerequisite to plating of the fracture as MMF is typically beneficial to achieving optimal fragment reduction. Temporary MMF techniques include the use of intermaxillary fixation (IMF) titanium screws, the use of Ivy loops, or the use of Ernst ligatures along with several other methodologies including a type of zip tie or embrasure wires. The instrumentation for the transoral approach to the angle uses transbuccal trocars for the plate and screw placement. It is beneficial to use threaded locking plates in the repair because the threaded locking plates can be secured directly to the transbuccal trocar to allow control of the plate while the repair is being secured and for drilling screw holes ( Fig. 1 ). Headlights and surgical magnification using loupes or endoscopes can improve visualization during the repair.

Currently, the Champy technique for osteosynthesis is used preferentially for noncomminuted fractures of the mandibular angle. The Champy technique was popularized by Maxime Champy in the 1970s. Dr. Champy recognized that the angle of the mandible had certain characteristics that were favorable with regard to using a load-sharing engineering concept with regard to mandibular fixation. Load sharing is an engineering technique where forces caused by mandibular function will be counteracted by placing plates with monocortical screws in such a way that tensile or distractive forces are obviated while beneficial compressive forces are strategically promoted. This is in contrast to load-bearing repairs, whereby all forces at play on a functioning mandible will be overcome and neutralized by thick and rigid plates that have absolutely no mobility and use bicortical screw placement. The Champy technique uses optimal plate placement along Champy’s lines using monocortical screws that counteract tensile forces that occur during mandible function while allowing compressive forces to be controlled in the pursuit of bone healing ( Fig. 2 ). By using monocortical miniplates to counteract tensile forces, smaller and thinner plates can be used. Less surgical exposure and periosteum stripping is required, and less bone drilling is necessary. However, the Champy technique is not a rigid technique. It does allow some movement at the fracture site after repair. The Champy technique also relies on bone surface area contact to help stabilize the fracture, and therefore, comminuted fractures are not ideal for the technique ( Fig. 3 ). One other factor makes the angle an opportune place for utilization of this technique: the fact that angle fractures are actually behind the dentate portion of the mandible. Similar to sagittal split osteotomy surgery, the location of the angle fracture in this retro-occlusal zone allows leeway with regard to the precision of the final osteosynthesis as it relates to postoperative occlusion.
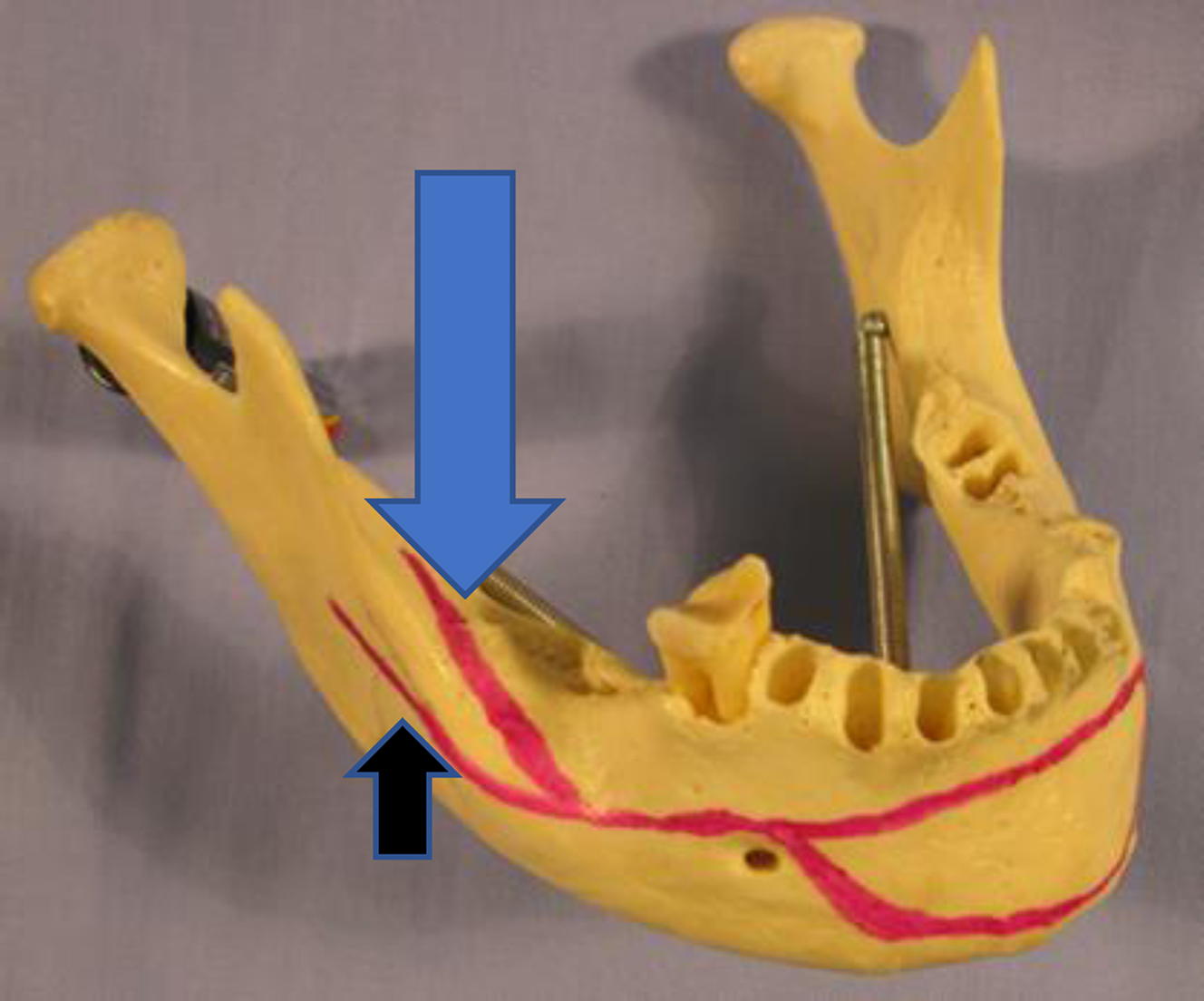
There have been numerous studies investigating the use of one versus two monocortical miniplates in open reduction and internal fixation of MAFs. Historically Michelet and colleagues, and later Champy and colleagues, introduced of the use of a single miniplate on the superior lateral border of the mandibular angle for osteosynthesis in MAFs ( Fig. 4 ). However, given the tensile forces of elevation on the mandibular ramus countered by the depressor forces on the mandibular body, later studies theorized that two miniplates should be placed, one superior and one inferior across the MAF ( Fig. 5 ). This has not been borne out in the literature as studies in which two points of fixation were used had higher complication rates than studies in which one miniplate was used. , A 2014 systematic review and meta-analysis by Al-Moraissi and Ellis found the use of one miniplate to be superior to the use of two, reducing postoperative complications (including dehiscence, infection, nonunion, malunion, malocclusion, and hardware failure). This corroborated randomized control trials of the same topic, showing that the use of two miniplates for MAF gave no additional benefit and increased both procedure time and risk of postoperative complication.
Malleable plates
Malleable fixation plates are a bendable and less rigid version of the classic Champy plate, have a thin profile, and similarly use monocortical screws. The plate must be bent to the contour of the mandibular arch on which it is being placed but is malleable enough to allow final contouring to be formed by the screws as they are tightened and driven home. These plates were initially intended for non-load-bearing areas, such as the mid-face, however; they were adapted for MAFs after studies found one point of fixation to be superior to two for reduction of these fractures. Potter and Ellis were among the first to report on the use of these thin malleable plates with 1.3-mm screws, and while they were found to provide sufficient reduction, there was a high rate of intraoperative failure due to plate fracture upon fixation. In 2011, Esen and colleagues performed a cadaver study on sheep mandibles showing the use of a single thin malleable plate was not sufficient alone to withstand the forces generated by biting. Thus, a single thin malleable plate is not considered the gold standard of treatment for fracture osteosynthesis.
Lateral border
Although not original to Champy’s description, monocortical miniplate placement on the lateral boarder of the angle in a superior position has been shown to have the lowest complication rate in the literature ( Fig. 6 ). Specifically, plate dehiscence has an odds ratio five times lower if the plate is placed on the lateral mandibular surface rather than on the external oblique ridge. The success of this technique may have to do with having more facile operative access through the transoral approach for this position of plate placement. The Champy technique is based on obviating tensile force, and placement of a plate on the lateral boarder can accomplish that task efficiently.

The lateral inferior boarder also can be used for load-bearing rigid fixation using bicortical screws and thick plates designed to bear the complete load of mandibular function. Three holes on each side of the fracture would be considered the minimum optimal engineering necessary to accomplish safe immediate function. The placement of such thick and large hardware in this position is often accomplished through an external skin incision to allow optimal exposure for plate placement and plate contouring. The choice of this technique is made when fractures are comminuted, when the mandible is edentulous and atrophic with loss of alveolar bone stock, or when there is tooth loss which reduces contact surface area. Load-bearing approaches are also preferential in circumstances where infection is present ( Fig. 7 ).