Case 1
Clinical Presentation
A 68-year-old White male had a complicated postoperative course after an osteocutaneous flap harvest from his right hip by another surgical service. He had a significantly large open wound over the right hip, measuring 25 × 10 cm, with exposed pelvic structures ( Fig. 31.1 ). This patient had previous wound debridement and a wound vacuum-assisted closure (VAC) by the primary service. Some granulation tissue had developed within the wound. The primary service used acellular dermal matrix that appeared to be incorporated with the wound bed ( Fig. 31.2 ). The plastic surgery service was asked by our ENT microvascular team to carry out a definitive wound closure.


Operative Plan and Special Considerations for Reconstruction
For this large soft tissue wound with exposed pelvic structures in the lateral hip and pelvis, a distant muscle flap with a relatively large amount of well-vascularized tissue, such as a rectus femoris muscle flap, can be selected to provide a one-stage soft tissue coverage and obliterate the potential space. The flap, which receives a blood supply primarily from the descending branch of the lateral circumflex femoral artery, is a type II muscle flap but is fairly reliable if the patient is free of peripheral vascular disease in the profound artery. It is a large muscle flap that can be used to cover lower abdominal wall or pelvic soft tissue defect. Approximation of the vastus lateralis and vastus medialis after the rectus femoris muscle flap harvest may possibly reduce weakness of the knee extension. An adjacent abdominal skin rotation flap can be added to facilitate the entire wound closure in addition to a skin graft to the muscle flap in this case.
Operative Procedures
Under general anesthesia with the patient in a supine position, the right hip wound was debrided first. All floating acellular dermal matrix was also excised but incorporated acellular dermal matrix was left in place.
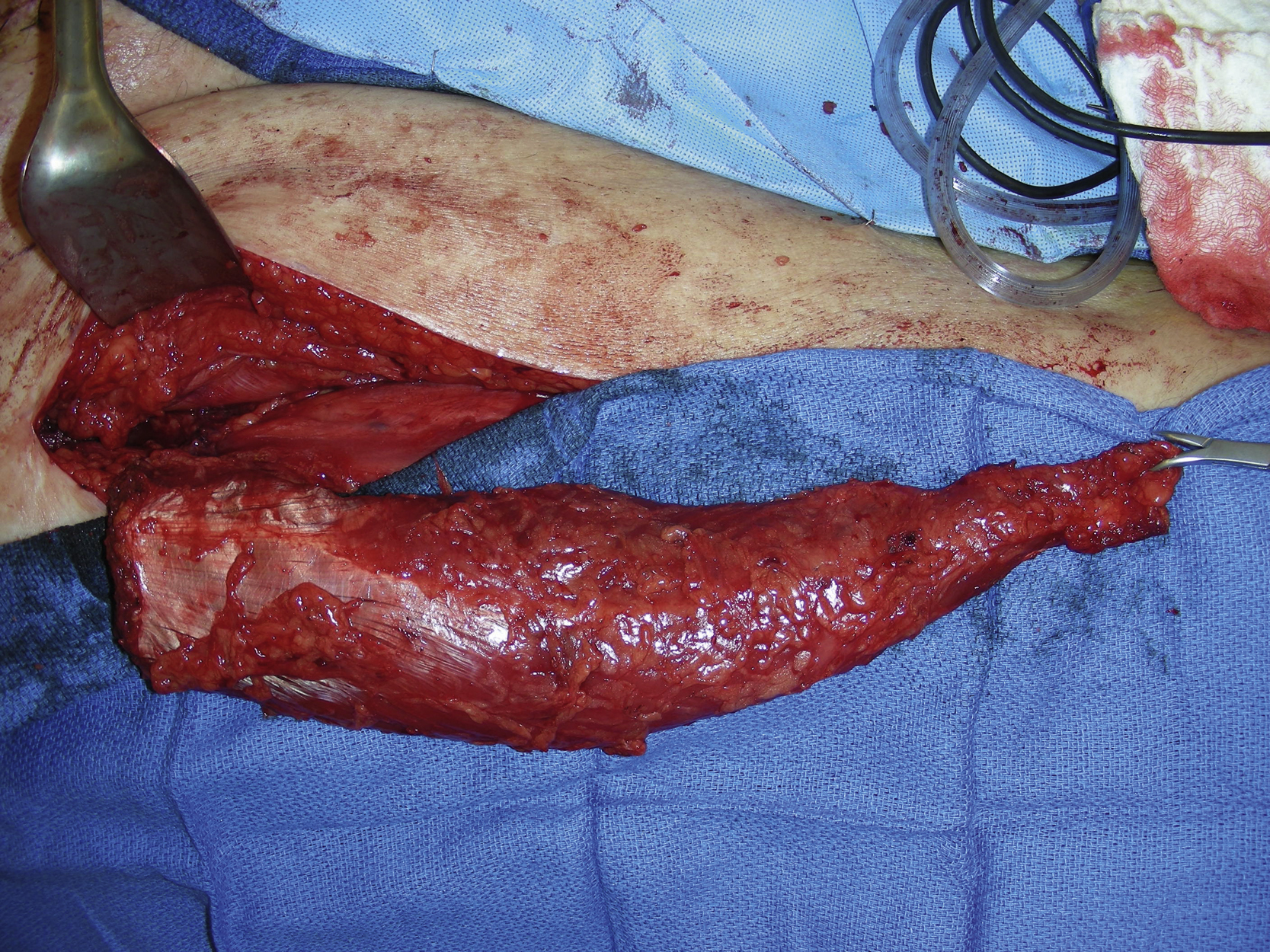
The design for the right rectus femoris muscle flap harvest was marked. The skin incision was made from the anterior iliac spine to the central part of the patella after infiltration with 1% lidocaine with 1:100,000 epinephrine. The skin, subcutaneous tissue, and fascia were incised and the rectus abdominis muscle was identified. The muscle was elevated and a Penrose drain was used to wrap around the muscle. The dissection was done to free its attachment to the vastus lateralis and vastus medialis muscles. The muscle flap was then divided more distally close to the patella. The muscle was elevated and the pedicle vessels were identified. One minor pedicle vessel was temporally clamped first and then divided with hemoclips. Further dissection was made around the major pedicle. ( Fig. 31.3 ). The proximal end of the muscle was divided and the flap was then tunneled to the right hip wound and secured using interrupted 3-0 Monocryl sutures.
Because of the area with the exposed acellular dermal matrix, an adjacent skin rotation flap was also elevated. This flap, measuring 12 × 3 cm, was rotated into the area to cover the exposed acellular dermal matrix. The skin flap donor site was approximated with several interrupted 3-0 Vicryl sutures and the skin closure was done with skin staples. A 10 flat JP was inserted under the muscle flap. The flap was inserted into the right hip wound and secured with multiple 3-0 Monocryl sutures to create a better contour and soft tissue coverage ( Fig. 31.4 ).

A split-thickness skin graft was harvested with a dermatome from the right lateral thigh. It was meshed to 1:1/2 ratio. The skin graft was placed over the muscle and the rest of the granulation wound and secured with multiple skin staples ( Fig. 31.5 ). A VAC dressing was placed over the skin grafted muscle flap and connected to a VAC machine ( Fig. 31.6 ).


The rectus femoris muscle flap donor site was closed after irrigation. A 10 flat JP was inserted into the donor site. Both vastus lateralis and vastus medialis muscles were approximated with interrupted 2-0 Prolene sutures. The deep dermal closure was performed with interrupted 3-0 Monocryl sutures and the skin was closed with skin staples.
Follow-Up Results
The patient did well postoperatively without any issues related to flap reconstruction and donor wound closure. He was discharged from the hospital on postoperative day 7. His right hip and pelvic wound healed uneventfully ( Fig. 31.7 ). He was followed by both the primary service and the plastic surgery service for subsequent care.

Final Outcome
The patient was routinely followed by the primary service for his postsurgical visits. His right hip flap reconstruction site has healed well with no wound breakdown or any other long-term issues related to the soft tissue reconstruction ( Fig. 31.8 ).

Pearls for Success
A large distant muscle flap, such as a rectus femoris muscle flap, can be selected to cover a large soft tissue wound in the hip and pelvic regions. The flap is fairly reliable and its flap dissection can be quickly performed. It can provide adequate vascularized tissue for an optimal wound closure because of its rich blood supply and the size of the muscle. It can also be used to obliterate a deep space in the pelvis as a pedicle flap. Both proximal and distal insertions can be divided to improve the flap’s arch of rotation and filling the potential dead space. If necessary, a sizable skin paddle can be included although the muscle flap alone is used more often because it is large enough. A proper vascular evaluation for the femoral vessels and/or profunda vessels may be necessary if the patient sustains peripheral vascular disease. A split-thickness skin graft is commonly used to place over the muscle flap and the healing can be enhanced with a 5-day VAC therapy. Approximation of the vastus lateralis and vastus medialis muscles may minimize the weakness of the knee extension after the rectus femoris muscle harvest.
Case 2
Clinical Presentation
A 26-year-old White male was involved in a motor vehicle accident and sustained multiple traumas including a left hip soft tissue avulsion with pelvic ring fracture. The fracture was fixed by the orthopedic trauma service, but a 33 × 15 cm large soft tissue wound was left with the exposed pelvic rim, which clearly required soft tissue coverage ( Fig. 31.9 ). The patient also underwent pelvic vessel embolization to control pelvic bleeding by interventional radiology when he was admitted to the hospital after trauma. The plastic surgery service was asked to provide a soft tissue reconstruction with a major flap so that his left hip open pelvic fracture site could be covered. With this complex wound in this location, a free tissue transfer would obviously be required to cover this large soft tissue wound.











