Hemiepiphysiodesis and Epiphysiodesis
Susan T. Mahan
Samantha A. Spencer
Hemiepiphysiodesis With 8-Plates for Angular Deformity of Knees
Operative indications
Abnormal lower extremity alignment such that the mechanical axis deviation is more than 1 cm or past midline of medial compartment (varus) or lateral compartment (valgus). Further indications include a knock-knee (genu valgum) or bow-legged (genu varum) gait that is painful or awkward, presence of medial or lateral thrust, and patellar subluxation in the presence of leg alignment deformity. Success of the operation does require adequate remaining growth to achieve physeal correction, typically a minimum of 1 year of growth remaining. If genu valgum or genu varum is noted bilaterally, and surgery is indicated on both legs, it can be done concomitantly
Equipment
Radiolucent table (can be radiolucent foot extension provided the child is not too tall), 8-plate set, general instrument tray, and tourniquet
Positioning
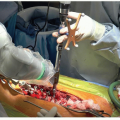
Supine with operative leg bumped up to allow access and good lateral fluoroscopic images (Figure 26.1). For bilateral knees, switch the trochanteric roll and leg bump between sides. Have the fluoroscopic C-arm on the opposite side of table. For the valgus knee, the operative leg is bumped up and the surgeon is on contralateral side
Surgical Approach
Localize and mark physis under fluoroscopy
Direct midaxial 2 to 3 cm incision over physis to be tethered
Dissect down to the physis without violating the periosteum
Provisionally place the plate and confirm fluoroscopically
Place the guide pins and confirm fluoroscopically
Place both screws and obtain final imaging
 Figure 26-1 ▪ Note proper positioning with the patella forward and easy access to the medial distal femur. |
Techniques in Steps
Put up the tourniquet after exsanguination of the limb (Figure 26.2)
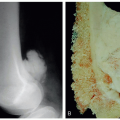
Fluoroscopy is used to identify the medial (genu valgum) or lateral (genu varum) distal femoral or proximal tibial physis (Figure 26.3)
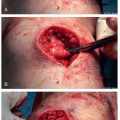
Make a 2- to 3-cm skin incision in the midaxial line (Figure 26.4)
Medial distal femur/valgus knee
Watch for the saphenous nerve/vein is posterior
Incise deep fascia, disturb distal vastus medialis as little as possible
Identify medial distal femoral epiphyseal artery
Plate positioned just anterior to this, distal end at epiphyseal branches
Medial proximal tibia/valgus knee
Palpate pes anserinus, incision proximal and slightly posterior to it
Pes anserinus tendons and infrapatellar branch saphenous nerve pulled posterior
Lateral distal femur/varus knee
Incision anterior to iliotibial band, split deep fascia
Lateral proximal tibia/varus knee, i.e., Blount disease
Incision proximal and anterior to fibular head; watch out for peroneal nerve which should be posterior
Often must elevate a small amount of tibialis anterior origin
Dissection to periosteum (any layer that can be picked up with forceps should be divided) (Figures 26.5 and 26.6)
Sweep freer around area of plate positioning ensuring freedom of overlying fascia/muscle layers
Place central guidewire or Keith needle by free hand in center hole 8-plate (Figure 26.7), check fluoroscopic images and adjust as necessary (Figure 26.8). Also be sure to confirm visually or with freer that no soft tissue is caught under the plate
It is critical to have perfect lateral of the knee prior to assessing the sagittal placement of the plate. Do not use a “figure-4” lateral view, but instead swing the C-arm to a true lateral image

Figure 26-4 ▪ Make a 2- to 3-mm incision directly over the medial physis for correction of genu valgum.

Figure 26-5 ▪ Dissect down to the level of the periosteum using a combination of blunt dissection and cautery.
Once plate optimal placed, drill or hammer tap in the central guidewire or Keith
Then, using the ball-tipped guide, place the proximal and distal guidewires centrally and slightly divergent (Figures 26.9 and 26.10). Avoid eccentricity of the wires or too much divergence as this prevents good screw placement
Check fluoroscopic anteroposterior (AP) (Figures 26.11 and 26.12) and then true lateral views until plate is optimally positioned (Figure 26.13)
Measure screws
Overdrill only the outer cortex using drill guide (Figure 26.14). Listen for high pitch and watch for failure to advance; if this is encountered, then drill is hitting edge of hole due to eccentricity of the drill in the hole. If this occurs, you need to reposition the wire or place drill directly onto the periosteum through plate without the guide under direct visualization
Place screws in tandem (Figure 26.15), halfway each to prevent the plate from flipping up (Figure 26.16)
After tightening screws, check that the plate is flush to periosteum with freer (Figure 26.17). A plate that is sitting off bone with exposed screws can cause pain and screw breakage. Solid screws are only necessary in obese children
Remove the guidewires and obtain a final fluoroscopic AP and lateral image (Figures 26.18 and 26.19). It is good to check the oblique images as well

Figure 26-9 ▪ Once positioning of the plate and central guide pin is confirmed, drill in the distal and proximal guidewires using the ball-tipped guide.
If performing bilateral hemiepiphysiodesis, have the fluoroscopic machine switch sides during closure of the first limb
Closure with deep Vicryl figure-of-8 sutures in muscular fascia, Scarpa fascia, subdermal interrupted buried Monocryl, and running Monocryl subcuticular on skin. Place local anesthetic and a soft dressing
If doing lateral proximal tibia 8-plates, leave deep fascia of elevated tibialis anterior unrepaired to avoid peroneal branch tension
Deflate tourniquet, typically 30 to 40 minutes per side. Circulating RN pushes bump to contralateral leg and then proceed with contralateral limb
Postoperative Care
Patients may be weight-bearing as tolerated with crutches as needed (usually around a week)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree