Case 1
Clinical Presentation
A 64-year-old White male with a history of hypertension and two previous coronary artery bypass grafting surgeries underwent uneventful heart transplantation for severe congestive heart failure. During his cardiac transplant surgery, the left femoral artery and vein were cannulated for cardiopulmonary bypass. He was placed on routine immunosuppression protocol for postoperative heart transplant care. Three months after the successful heart transplantation, the patient presented with a large seroma secondary to lymphorrhea in the left groin cannulation site and underwent an incision and drainage of the seroma and placement of a closed drain by the cardiothoracic surgery service. Unfortunately, the patient developed persistent and uncontrollable drainage of lymphatic fluid (300–400 mL/day) from the left groin over the course of the next 2 weeks with no signs of improvement. The bacterial culture from the drain showed Pseudomonas and the patient was given appropriate antibiotics. The plastic surgery service was asked to manage recalcitrant groin lymphorrhea ( Fig. 32.1 ).
Operative Plan and Special Considerations for Reconstruction
Intraoperative lymphatic mapping technique with intradermal injection of blue dye was selected to identify all lymphatic leak sites so that lymphorrhea could be controlled by ligating those afferent lymphatic vessels. A selected local muscle flap, such as sartorius muscle flap, was selected to provide reliable soft tissue coverage to the femoral vessels, eliminate dead space within the groin wound, seal lymphatic leak sites, and eradicate infection by increasing vascularity. In addition, it might act as a conduit for lymphatic drainage in the groin.
Operative Procedures
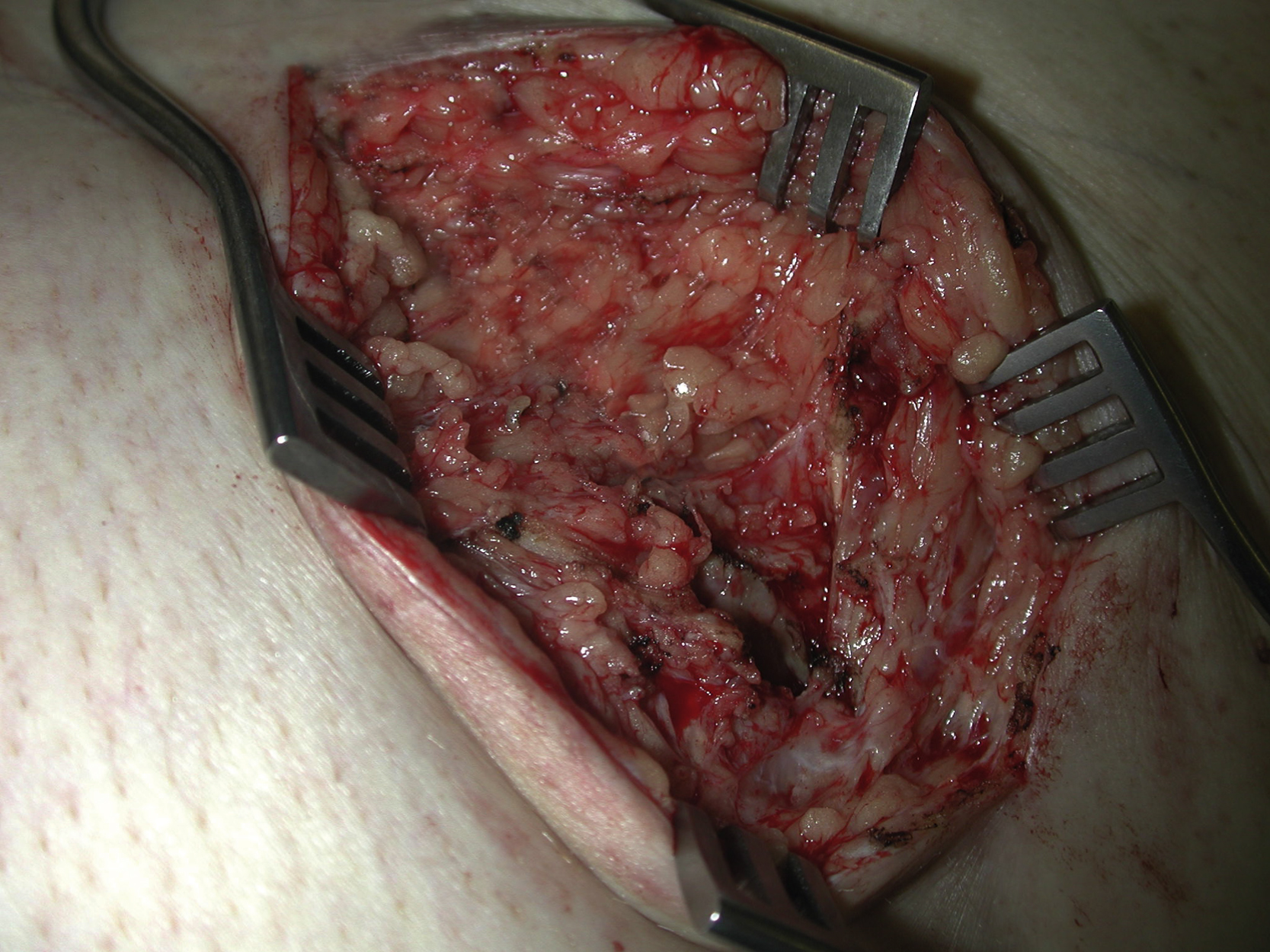
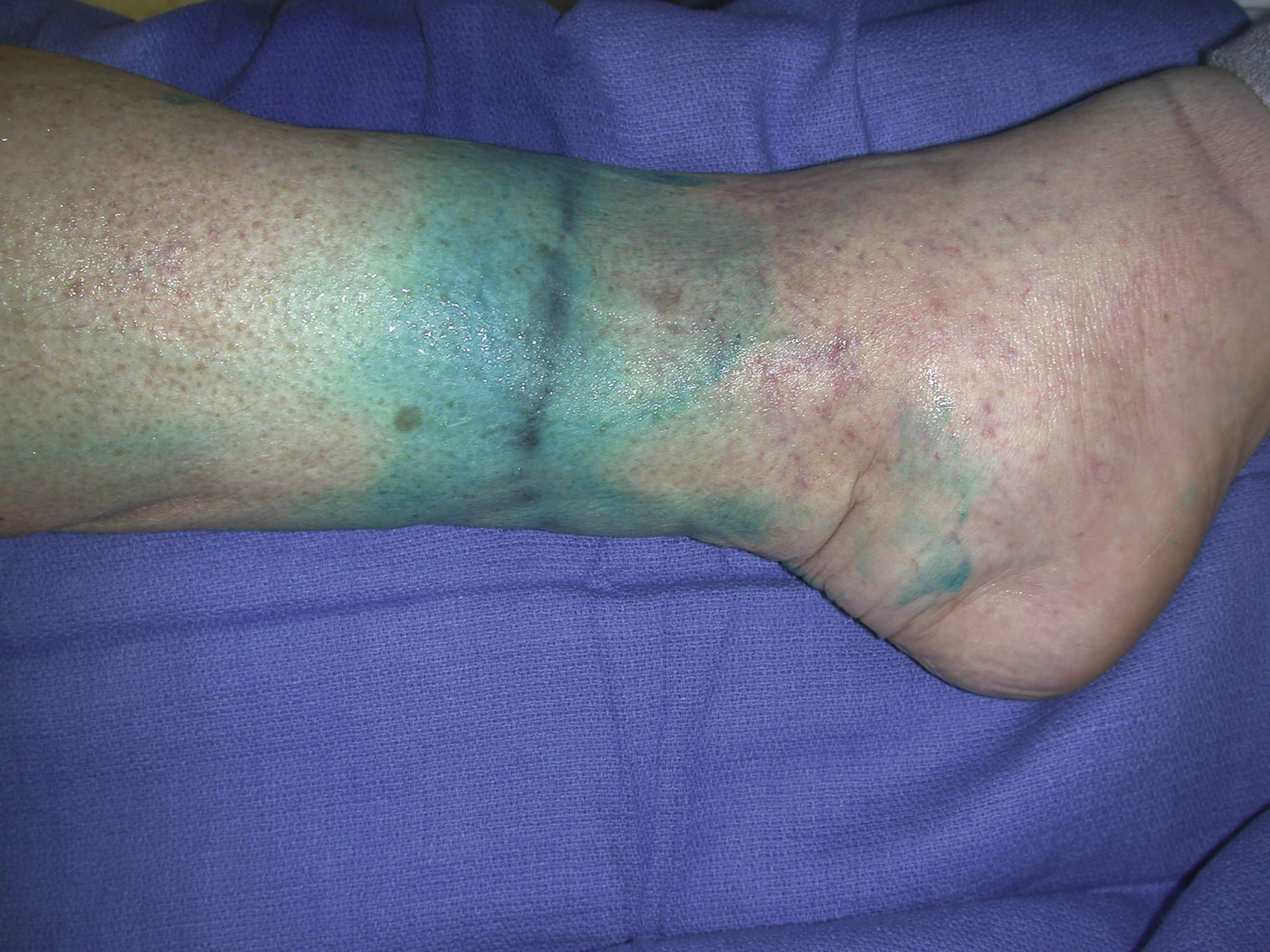
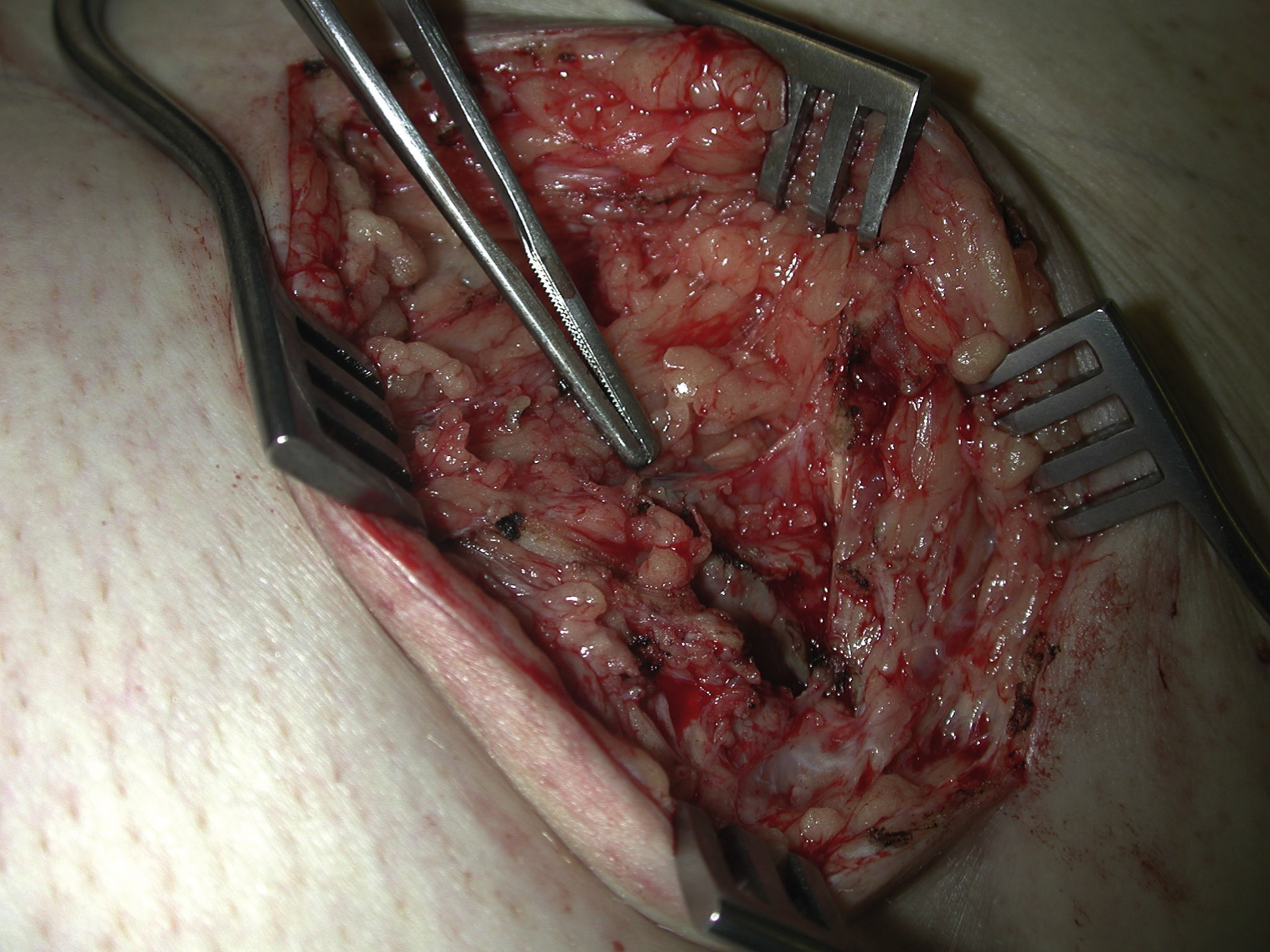
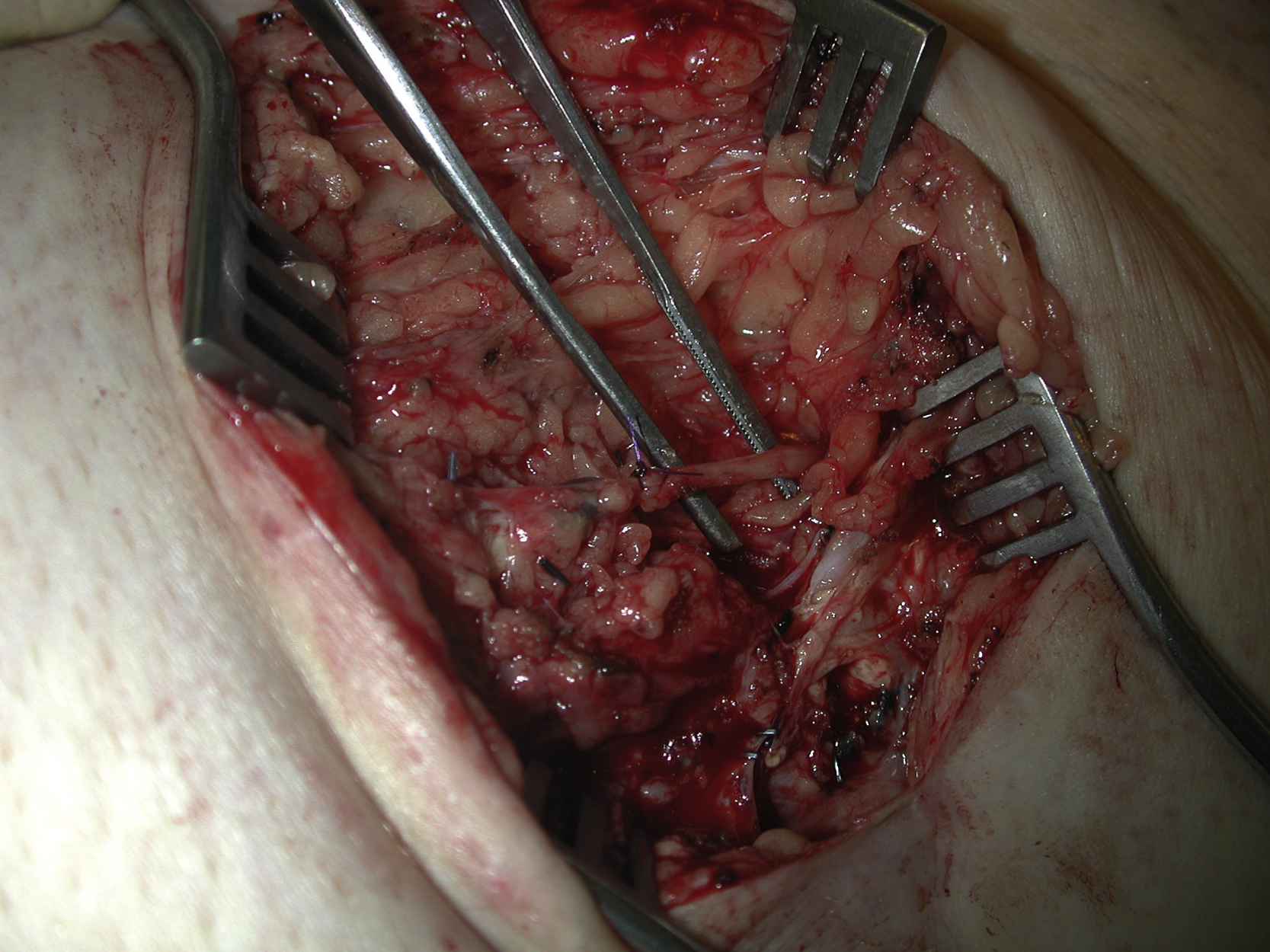
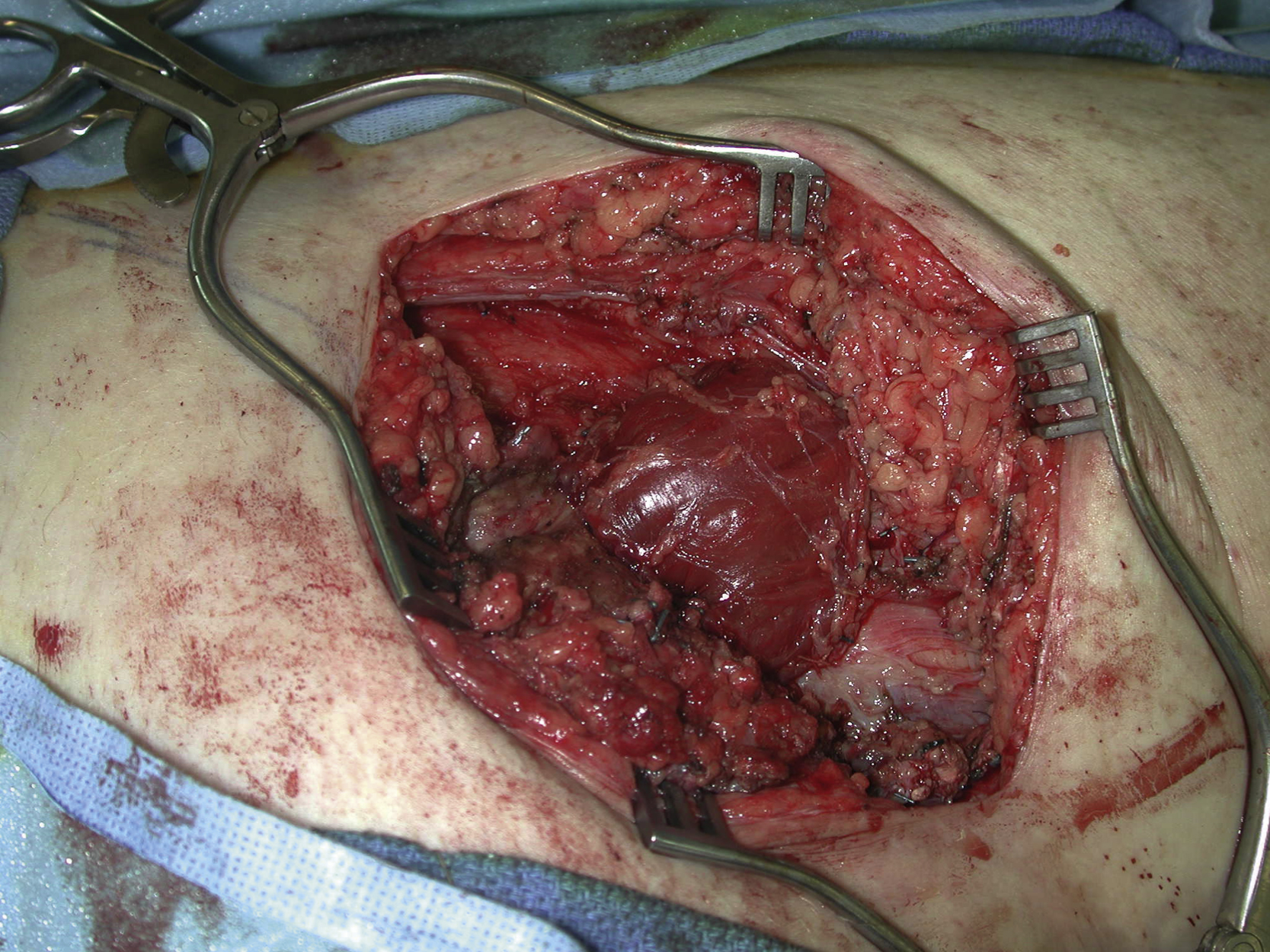
Eight weeks after the initial presentation of the groin seroma, 3 cc of isosulfan blue dye (Lymphazurin) was injected intradermally just proximal to the left ankle under general anesthesia. The injection was done circumferentially in order to incorporate all lymphatic drainage of the lower extremity ( Fig. 32.2 ). The injected area was gently massaged and the leg was elevated to speed migration of the blue dye. The blue dye can usually be seen emerging from the damaged lymphatic vessels after 15 minutes. The previous left groin incision was reopened. Within the left groin wound, several blue-stained lymphatic vessels were identified and directly ligated with metallic surgical clips or PDS sutures ( Fig. 32.3 ). A large sentinel lymph node and its afferent lymphatic vessel were also identified and directly ligated ( Fig. 32.4 ). During gentle surgical dissection of the femoral vessels, more blue-stained lymphatic vessels were identified and they were directly ligated with suture-ligatures or metallic clips. A sizable well-formed capsule was found lateral and superior to the femoral vessels. The capsule was only partially removed because of the amount of dense adhesion to the femoral vessels. After a thorough irrigation and adequate hemostasis, the sartorius muscle was identified and elevated. Once the insertion of the sartorius was divided from the anterior superior iliac spine, the flap was easily transposed medially to cover the femoral vessels after the first perforator to the muscle was divided ( Fig. 32.5 ). A drain was placed within the groin wound. The subcutaneous tissue and deep dermal layers of the incision were closed with interrupted absorbable sutures and the skin incision was closed with skin staples.
Follow-Up Results
The patient did well without any postoperative complications. He was discharged from hospital on postoperative day 5. The left groin incision healed uneventfully and the drain was removed once the drain’s output became minimal. The left groin lymphorrhea subsided and was eventually resolved within 3 weeks after the surgery.
Final Outcome
The patient returned to his active normal lifestyle and has been followed by the cardiothoracic surgery service since then for routine post heart transplant office visits. No local lymphorrhea or wound breakdown of the left groin recurred during the following 2 years ( Fig. 32.6 ).











