Fundamentals of Cutaneous Surgery
Frank Custer Koranda MD, MBA
Skin, “the gift wrap of life” is the barrier between us and a hostile environment. Skin is the largest organ of the body. Sooner or later, most physicians will have to deal with a tear, cut, or incision into this barrier that will need to be repaired.
Instrument Selection
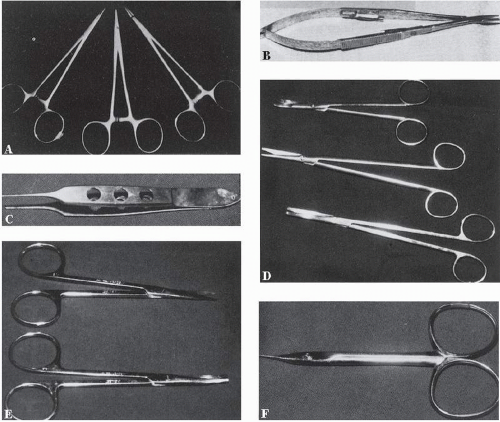
Quality instruments are expensive but are usually worth the price. For most cutaneous surgery, smaller needle holders are best, such as the Webster, Halsey, or smooth-jawed needle holders used in neurosurgery (Fig. 6-1A). Smooth jaws are less traumatic than precise needles and less apt to cut 5-0 or 6-0 sutures than serrated jaws. For very delicate surgery and for very fine sutures such as 7-0, the Castroviejo needle holder may be preferred (Fig. 6-1B). The amount of motion necessary to lock and unlock the Castroviejo is less than that required for the standard type of needle holder.
Skin should be handled as atraumatically as possible. Very gentle handling requires the use of skin hooks such as the single-hook Frazier or the fine double-hook Tyrell. If using pickups to handle tissue, use Adson forceps with fine teeth or Micro-Adson forceps. A finer type of forceps is the Bishop-Harmon with teeth (Fig. 6-1C).
For scissors dissection, a Littler is well designed for most situations (Fig. 6-1E). For finer work, a Stevens scissors is a good choice (Fig. 6-1E).
If larger scissors are desired, the Metzenbaum, Malis, or Ragnell scissors may be used (Fig. 6-1D). For precise cutting of sutures and for suture removal, the Gradle scissors may be used (Fig. 6-1F).
The no. 3 scalpel handle is used with the nos. 10, 11, and 15 blades. For precise incisions, the 15C blade is best. This blade was originally designed for periodontal surgery.
A basic cutaneous surgical pack may include the following:
Webster or neurosurgery smooth-jawed needle holder
Adson delicate forceps with teeth or Micro-Adson forceps with teeth
No. 3 scalpel handle
Littler scissors
Fine suture scissors
Utility sutures for cutting dressings
Mosquito hemostats (two)
Towel clips, 31/2 in
Gauze sponges, 4 × 4 in (ten)
Several round toothpicks for skin marking (toothpicks dipped in methylene blue) make a finer line than the standard marking pens and are less expensive
Cotton-tipped applicators as an option for point control of bleeding
Suture Selection
The two general groups of suture are absorbable and nonabsorbable. The common absorbable sutures are:
Plain gut
Chromic gut
Polyglactin 910 (Vicryl)
Polyglycolic acid (Dexon)
Polydioxanone (PDS)
Polyglyconate (Maxon)
Poliglecaprone (Monocryl)
Gut suture is made from the submucosal layer of the small intestine of sheep and the serosal layer of cattle and undergoes degradation by phagocytosis, creating a foreign body response in the patient. Plain gut gradually looses its tensile strength over 2 weeks. Chromic gut suture is coated with chromic salts to delay degradation. It has a slightly prolonged tensile strength over plain gut.
Fast-absorbing plain gut is a modification of plain gut that is designed to break down in 4 to 7 days and is used as a skin stitch. It comes in 6-0 and 5-0 sizes. The 6-0 fast-absorbing plain gut usually does break down in 6 to 7 days, but the 5-0 often persists for 10 to 15 days. The 6-0 fast-absorbing suture can usually be wiped out of the incision with a moistened Q-tip or with antibiotic ointment on the Q-tip. The disadvantage is that there may be more of an inflammatory reaction to this material than to nylon.
Synthetic absorbable sutures undergo degradation by hydrolysis. Synthetic sutures usually produce less of an
inflammatory response in the subcutaneous tissue than do the gut sutures. Vicryl and Dexon are similar, but Vicryl has a better tensile strength profile, maintaining 75% at 2 weeks and 50% at 3 weeks. The hydrolysis and absorption of Vicryl is also significantly faster than that of Dexon. PDS and Maxon maintain their tensile strength longer—70% at 3 weeks, 50% at 4 weeks, and 25% at 6 weeks. Hydrolysis occurs between 180 and 210 days.
inflammatory response in the subcutaneous tissue than do the gut sutures. Vicryl and Dexon are similar, but Vicryl has a better tensile strength profile, maintaining 75% at 2 weeks and 50% at 3 weeks. The hydrolysis and absorption of Vicryl is also significantly faster than that of Dexon. PDS and Maxon maintain their tensile strength longer—70% at 3 weeks, 50% at 4 weeks, and 25% at 6 weeks. Hydrolysis occurs between 180 and 210 days.
Monocryl maintains 50% to 60% of its tensile strength at 1 week and 20% to 30% at 2 weeks. It is a good choice for a facial subcutaneous suture since it produces less of an inflammatory response than Vicryl or Dexon. Monocryl usually requires five to six throws on the knot or there may be slippage.
The major nonabsorbable sutures are silk, nylon, and polypropylene. Silk suture is frequently used on the eyelids and lips since it is soft and not irritatingly sharp.
Monofilament nylon suture such as Ethilon is a generalpurpose skin suture. Polypropylene or Prolene is a monofilament suture with an increased memory and high tensile strength. It requires six throws to a knot.
For subcutaneous sutures on the face, usually a 4-0 or 5-0 size suture is used. For skin sutures on the face, usually a 5-0 or 6-0 size suture is used. For more delicate work, 7-0 size may be indicated.
For skin and fascia, use a reverse cutting needle. With the reverse cutting needle, the cutting edge is on the outside of the curve. For facial surgery or for other fine cutaneous surgery, precision point needles are best. There is reduced tissue drag and trauma with these supersmooth, highly honed needles. In the Ethicon product line, these needles have the code prefix P, PS, or PC (for plastic or plastic surgery or plastic cosmetic) and in the Davis & Geck line, PR or PRE (for plastic reconstructive). The number after the prefix indicates the size of the curvature. The P3 needle has good utility for the face. For general cutaneous surgery, an FS (for skin) reverse cutting needle may be used, but there is considerable drag and tissue resistance compared with the precision needle.
Types of Stitches
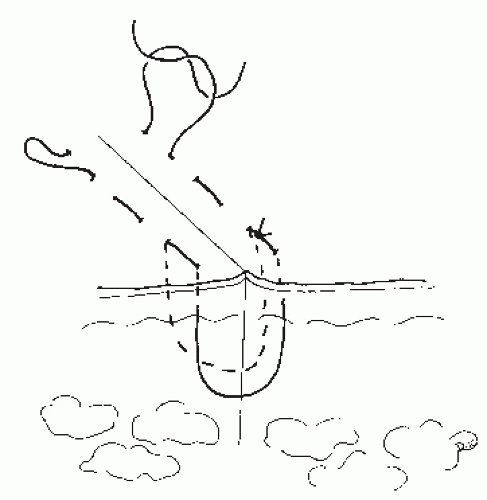
Buried Subcutaneous Stitch
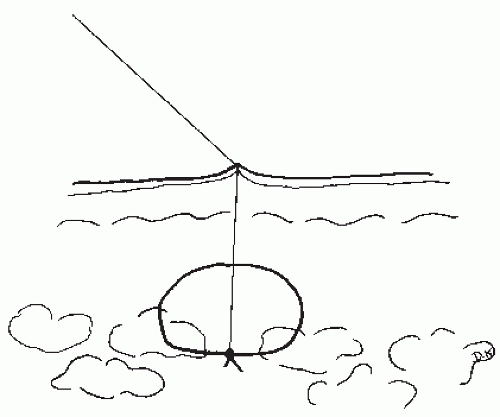
The buried subcutaneous stitch is used to close the dead space to prevent hematoma and a nidus for infection (Fig. 6-2). It also reduces the tension on the skin. Burying the knot deep in the tissue decreases the amount of tissue reaction in the
more superficial part of the wound so that the major inflammatory response is away from the surface of the incision and less apt to disrupt it.
more superficial part of the wound so that the major inflammatory response is away from the surface of the incision and less apt to disrupt it.
To bury the knot, the needle first enters through the deep portion of the wound and exits more superficially on the same side. It then enters superficially on the other side of the wound and exits through the deeper tissue on that side of the wound. This is usually an absorbable suture.
Many texts recommend that interrupted subcutaneous sutures be used in case a suture breaks. However, multiple buried sutures, each with a knot, will place a greater mass of foreign body in the tissue and produce a greater inflammatory response. Running a subcutaneous suture poses no difficulty even if the suture should break since the friction on the suture and the edema of the tissue secure it.
Simple Skin Stitch
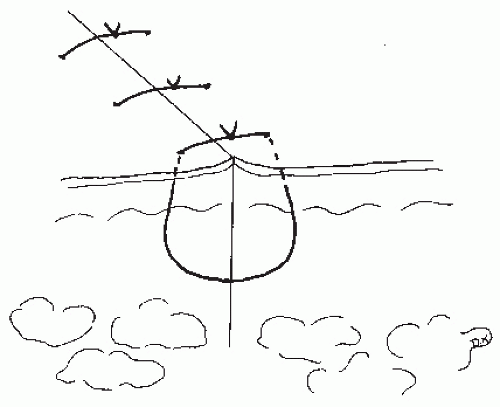
With the simple skin stitch, the suture is passed through the epidermis and dermis from one side to the other (Fig. 6-3). The exit and entry points are usually 2 to 3 mm from the incision edge. A greater “bite” of tissue should be taken more deeply than superficially to help evert the wound edges.
The simple skin stitch functions to approximate and evert the wound edges and to adjust the height of the wound edges so that they are even. If one side of a wound is lower than the other side, a slightly deeper bite should be taken on the lower side for the initial wound height adjustment. The knot is then placed on the lower side of the wound to further finely adjust the height of the wound edges.
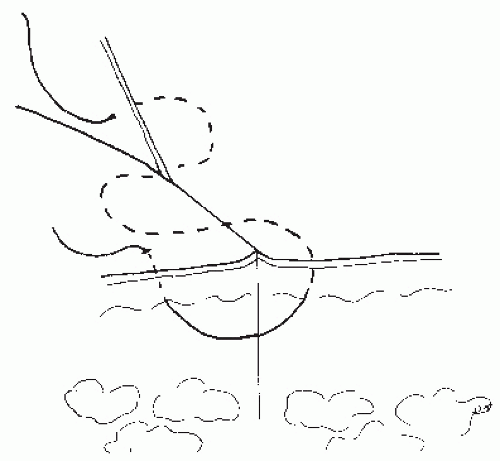
Vertical Mattress Stitch
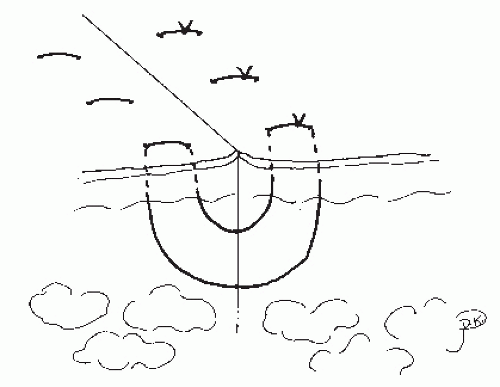
The vertical mattress stitch tents up the skin edges (Fig. 6-4). This eversion of the edges compensates for contracture that later occurs in the wound which may produce a linear depression. If with simple interrupted stitches or with a simple running stitch the wound is not everted sufficiently, vertical mattress stitches may be placed in the areas not everted.
Horizontal Mattress Stitch
The horizontal mattress stitch is used for the closure of a wound under tension. It can cause strangulation of the skin (Fig. 6-5). Therefore, it may be used with a bolster such as a small piece of a red Robinson catheter through which the
exposed suture passes to reduce the pressure on the skin. In general it is not a preferred stitch for facial surgery.
exposed suture passes to reduce the pressure on the skin. In general it is not a preferred stitch for facial surgery.
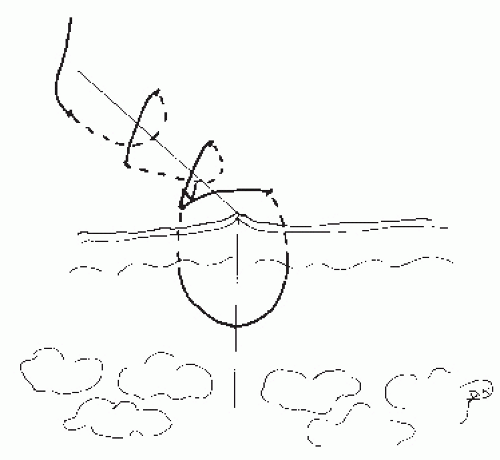
Corner Stitch (Tip Stitch)
The corner stitch is used for v-shaped corners, to prevent necrosis of the skin tip. It is inserted vertically down through the main segment of skin and out through the dermis. It then enters horizontally through the dermis in the tip of the flap and out and then back up through the main segment of skin (Fig. 6-6). The suture should enter and leave the flap tip in the same dermal plane that it exits and reenters the dermis of the main body of skin for an even wound.
Running Simple Stitch
The running simple stitch is a continuously repeated over-and-over stitch that is a rapid method of closure (Fig. 6-7). This stitch can evenly distribute tension along the wound. By adjusting the depth of bite of tissue with each placement of the suture, the height of the wound edges may be adjusted. This stitch is easier and less traumatic to remove than multiple interrupted stitches.
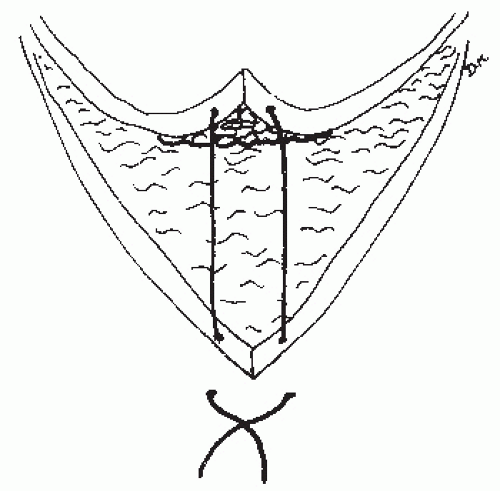
Running Intradermal Stitch
The running intradermal stitch is placed in the dermis and may be left in place for an extended period without causing cross-hatching of the skin (Fig. 6-8). The suture used may be a permanent type such as Prolene because of its memory and strength or an absorbable type such as PDS or Monocryl depending on the stress on the wound. The suture enters the skin at a point 4 to 5 mm beyond the edge of the incision. From this point it is brought into the wound and then into the dermis on one side and crosses to the other side. The stitch is continued in a running S pattern staying in the same plane of the dermis from one side to the other. In a long running intradermal stitch that is to be removed, it is wise to have it periodically come through the surface of the skin and then back in through the skin. This allows for removal of the suture in short segments facilitating later removal since the friction on the suture and the healing process tend to secure the suture. With PDS or Monocryl, the need for removal can be avoided.
Although the running intradermal stitch nicely coapts the wound edges, further approximation may be accomplished with a tissue adhesive to the surface of the skin edges.
Suture Tying
Sutures should be tied so that they lie down as square knots. The sutures should be tied to coapt the wound edges but not to strangulate. Most err by tying too tightly. One way of avoiding too tightly tied knots is to not snug down the second throw of the suture. Leaving this throw slightly loose also compensates for the tissue edema that develops in wounds. Tying too tightly is a major cause of suture track marks on the skin. Leaving sutures in too long is another factor. Granulomas or microcysts may form along the suture tract if the suture is left in too long.
Hemostasis
Hemostasis is essential to good wound healing. A rule of thumb on controlling bleeders is that named vessels should be clamped and ligated, and unnamed vessels may be
electrocoagulated. In tying off vessels, use the smallest suture that is practical, usually a 4-0 or 5-0 on the face. The suture should be cut on the knot to leave the least amount of material in the wound that might cause a foreign body reaction.
electrocoagulated. In tying off vessels, use the smallest suture that is practical, usually a 4-0 or 5-0 on the face. The suture should be cut on the knot to leave the least amount of material in the wound that might cause a foreign body reaction.
A biterminal device is usually used for electrocoagulation. The current enters the patient through an active or coagulating electrode. When tissue contact is made, heat is generated and coagulation occurs. The current passes through the patient and out via the dispersing electrode, the grounding pad. The patient usually becomes part of the current circuit.
The grounding pad should be placed as close as possible to the surgical site. If possible, the heart should not be between the active electrode and the grounding pad because it then becomes part of the current pathway. The area of coagulation should be kept dry with sponging or with suction; bleeding into the area disperses the current and diminishes the coagulation effect.
Biterminal coagulation is not bipolar coagulation. Bipolar coagulation is the system in which a single electrode contains both terminals. With bipolar coagulation forceps, the current passes between the tines of the forceps, coagulating the tissue between the tines. Bipolar coagulation is more precise, produces less tissue damage, and does not involve current transmission through the patient.
True electrocautery is essentially a red-hot branding iron that seals blood vessels by the direct application of heat. An electrocautery system uses either low-frequency alternating current or direct current. The current remains in the electrode tip and does not pass into the patient. There are a variety of disposable battery-powered cautery pens.
In the preoperative evaluation, it is important to ask whether the patient has any implanted electrical devices such as a pacemaker, vagus nerve stimulator, or other neurostimulator. The majority of newer pacemakers are defibrillating. With the defibrillating pacemakers, electrocoagulation should not be used until proper protective measures have been undertaken. The manufacturers have toll-free numbers to call for instructions. In the event that there is a question, the cautery pens should be safe because they seal the blood vessels by direct heat and not by electricity.
Patient Information on Potential Complications or Side Effects of Skin Surgery
1. Scar formation: Scars form whenever there is injury to the skin. Some scars are more noticeable than others. Some individuals are more prone to thickened or keloid scars. Scars in areas of high sebaceous gland concentration and activity such as the nose and forehead are more likely to be widened and become depressed. Postoperative treatment of the scar may be necessary.
2. Pain: Postoperative pain will depend on the extent of surgery and also on the particular individual. Pain medications are prescribed and may be taken after surgery if needed. With pain medications, do not drive, operate machinery, or make important decisions. Alcohol can amplify the effects of pain medications. It is best to eat something solid before pain medications since they may irritate the stomach and cause nausea.
3. Bleeding: Bleeding after surgery can usually be controlled with pressure applied to the wound for 15 to 20 minutes and with ice compresses. Some oozing is to be expected. In the case of severe or persistent bleeding, please call the doctor.
4. Swelling: Various degrees of swelling will occur. Cold compresses on for 20 minutes and off for 10 minutes for the first 24 to 48 hours will lessen swelling. Elevation of the head at 15 to 20 degrees when lying down or sleeping will help to reduce edema. A reclining chair usually provides a good angle of head elevation.
5. Bruising: Bruising around the surgery site will resolve. With surgery of the anterior scalp, forehead, or around the eyes, a black eye may develop within 12 to 72 hours after surgery. Sometimes the eye will swell shut.
6. Hematoma: This is a lump that forms under the skin from bleeding after the surgery. It represents a collection of blood.
7. Infection:With any injury to the skin or surgery, infection is possible. Therefore, an antibiotic ointment, and sometimes antibiotic tablets, may be prescribed at the time of surgery. Wound infections usually occur 4 days after surgery. If you suspect an infection, please call the doctor.
8. Numbness: It is common to have numbness in the area of surgery because there are always sensory nerves running through the skin. Usually this numbness will go away in 6 to 12 months. But in some instances, it may be permanent.
9. Paralysis of nerve: If a cancer extends into the area of a nerve that controls the movement of muscles, temporary or permanent paralysis may occur. The greatest areas of risk on the face are the temple area where the nerve to the eyebrow and eyelid runs and the lower cheek where the nerve to the lower lip runs.
10. Wound dehiscence: In straightforward terms, this means the wound separates or pulls apart. This can happen anywhere, but it is most prone to occur when the wound overlies an area of muscle mass such as on the back or the extremities. If a body movement seems to tug on the wound, stop the movement and relax.
11. Wound healing: Not all skin wounds heal ideally. At times a skin repair, graft, or flap may fail to heal well or the wound may seem to lift up or protrude. This may affect part of the wound or the whole wound. Most often, the wound will still heal adequately with treatment. Sometimes additional surgery is required.
Patient Instructions for Surgery
1. If you are taking prescribed medications, continue to take them unless instructed otherwise.
2. If you are taking Plavix (clopidogrel) or Coumadin (warfarin) because of a heart attack, atrial fibrillation,
blood clot, heart stent, stroke, or transient ischemic attack (TIA), you will usually be able to continue on the medication, although you will probably bleed more and may have a greater chance of postoperative bleeding. If you are taking Coumadin, you may require a blood test international normalized ratio (INR) within a week of surgery.
blood clot, heart stent, stroke, or transient ischemic attack (TIA), you will usually be able to continue on the medication, although you will probably bleed more and may have a greater chance of postoperative bleeding. If you are taking Coumadin, you may require a blood test international normalized ratio (INR) within a week of surgery.
3. If you are routinely taking aspirin or ibuprofen products such as Motrin, Aleve, or Advil for headaches, pain, or preventive measures, please stop 10 days before surgery. These products may cause more bleeding during and after surgery. Aspirin and ibuprofen may be in various products. For instance aspirin is in Pepto-Bismol and Alka-Seltzer. Aspirin may be listed as salicylate or salicylic acid. If you have arthritis, celecoxib (Celebrex), an anti-inflammatory drug that does not have an effect on bleeding, may be prescribed. It is used with caution in patients who have cardiovascular disease or risk factors for cardiovascular disease.
4. If you have a pacemaker, it is important that you inform the doctor and specify its type and whether it is a defibrillating pacemaker so that proper precautions may be taken. Please also mention if you have a neurostimulator implant such as a vagus nerve stimulator.
5. If you have any joint replacement implants you may need antibiotics prior to surgery. If you have had carditis, mitral valve prolapse, or heart valve replacement, you will be prescribed preoperative antibiotics.
6. Two weeks before surgery, stop taking vitamin E and supplements such as garlic, ginger, ginkgo biloba, ginseng, and ephedra. In general, it is best to stop all supplements 2 weeks prior to surgery.
7. Stop smoking for 2 weeks before and for 2 weeks after surgery. It is well documented that smoking causes poor wound healing.
8. Wash your hair the night before or morning of surgery.
9. Shower and wash your face the morning of surgery.
10. Someone should come with you or be available to drive you home.
11. Please arrive at the designated time.
12. If you decide to cancel surgery, please let your surgeon know in enough time so that another patient can be scheduled. However, doctors do understand that illness may occur unexpectedly.