This article presents the authors’ experience with the use of fat grafting via the Coleman technique, for the adjuvant treatment of facial burn wounds and their sequelae. It demonstrates the regenerative effects of fat injected under the wound and/or the scar as well as of fat delivered to the debrided surface of the wound and to the surface of the scar after laser treatment or microneedling.
Key points
- •
The use of fat grafting has been incorporated into our everyday routine, changing our practice dramatically.
- •
In relation to facial burns and their sequelae, these changes are more noticeable in the way we treat the resulting scar is taken care of, when present, because fat grafting has also greatly influenced the way hypertrophic scars are treated as a consequence of burn wounds.
- •
One of the most pleasant surprises in using fat grafts is the minimal incidence (or none) of hypertrophic scarring on the healing of wounds treated with 1 or more sessions of fat grafting.
- •
In cases whereby no fat grafting was used to treat the acute wound, fat grafting can be used to treat the sequela, and one can note improvement of the scar appearance as well as in volume, as early as 1 to 2 weeks after fat injection/fat delivery.
Introduction
Fat grafting has become a common procedure in wounds originated from trauma or other causes. Fat contains adipose-derived stem cells and a great variety of growth factors that may have a direct effect in wound healing. Fat grafting has also been used successfully for the management of scars and posttrauma healing fibrosis, scarring, and pain. Adipose-derived stem cells may differentiate into fibroblasts, keratinocytes, and other cells; they may also secrete mediators with neoangiogenic and anti-inflammatory properties. This fact would allow for them to act in all phases of the wound-healing process as it is understood today. Fat on the lipoaspirate can be isolated and/or treated by physical or chemical methods, in the operating room (OR) or in a laboratory setup.
As it was used more than a century ago to treat facial deformities, fat grafting, originally (re)introduced in the cephalic segment aiming for improvement in aesthetic aspects of the face and periorbit by Coleman in the early 1990s, soon became one of the main options for disease, trauma, or postsurgery-related deformities.
Preoperative evaluation and special considerations
Patients with wounds or scars who are candidates for a fat-grafting procedure at the authors’ service are those with the following:
- 1.
Hypertrophic scars that are not improving or not being controlled by pressure garments at 6 or more weeks after healing
- 2.
Burn wounds with 3 weeks or more with no apparent progression to healing
- 3.
Subacute burn wounds or other wounds that are transferred to the authors more than 6 weeks after the accident or wound
- 4.
Venous or diabetic ulcers
- 5.
Decubitus ulcers
- 6.
Wound cavities of any origin (avulsion, drained hematomas, tumor resection, and so forth)
- 7.
Shoulder, wrist, knee, and ankle tendinitis; postfracture “bone pain”; major joint arthrosis
Patients with subacute burn wounds (more than 3 weeks [in the authors’ service]) without apparent progression to healing and patients with hypertrophic scarring after healing of a burn or other type of trauma or keloids of any origin are also selected for treatment with fat injection/delivery. Repeat injections (up to 4 injections total) are performed at 7- to 10-day intervals for wounds or at 6- to 8-week intervals for scars.
The use of fat grafting as an adjuvant treatment in acute and subacute burn wounds aims at taking advantage of fat’s benefits: a variety of metabolic and regenerative properties, increasing vascularization, and enhancing the tissue regeneration process. When these wounds are treated with (repeated) fat grafting, healing (with minimal fibrosis) is the planned outcome. When treating burn scars, the objective is to decrease the amount of hypertrophy (fibrosis), diminishing the scar thickness, and increasing scar malleability.
The actual surgical procedure is performed in the OR, following all rigors and care for sterile procedures.
Surgical procedure
Donor Site Selection
Donor areas are “rotated” as needed, and fat most frequently is obtained from the thighs or lateral upper buttocks, and less frequently, from the abdomen (in the authors’ practice, to obtain fat from the abdomen, they first order an ultrasound of the abdominal area to verify the presence [or absence] of wall defects or hernias, which would preclude the use of this area as a donor area).
When necessary, shaving of the pubic area or proximal thigh is performed in the OR, immediately before the procedure. Puncture incisions for the introduction of the liposuction cannula are placed on the midline, at the suprapubic crease, or medial to the femoral pulse, at the inguinal crease, or in the middle axillary line, at the upper border of the iliac bone.
Fat Graft Harvest
The actual volume of harvested lipoaspirate should be at least twice the anticipated volume planned to be injected, and at least 4 times this volume, if one is also planning to have fat delivered over the wound or the scar.
Fat Graft Process
In wounds, the authors use the Coleman technique, repeating injections (and reharvesting) every 7 to 10 days, until healing or until a definite procedure (such as wound closure, skin grafting, flap, or other) is performed. After healing, injections under the scar and fat delivery over the scar are performed at 6- to 8-week intervals, also via the Coleman technique.
This approach is also used with patients with scars who seek the authors’ service for consultation after being treated elsewhere.
Fat Graft Injection
Patient positioning
Patients are positioned supine when using the abdomen or thighs as donor areas or on lateral decubitus when obtaining fat from the lateral upper thighs. Fat is usually injected and delivered while the patient is supine.
Surgical technique
Fat harvesting and fat injection are sterile surgical procedures and should be performed only in accredited ORs under rigorous, completely sterile technique. Patients are submitted to general anesthesia or regional block.
Recipient site preparation
In patients with scars (healed wounds), the donor area and recipient area are individually prepared and draped in the usual manner.
In patients with open, nonhealed wounds, the donor area is initially prepared and draped, and fat is obtained by liposuction; only then, after the planned amount of fat is obtained, the recipient area is prepared and draped, while the obtained fat is being centrifuged and distributed into various syringes.
Fat is harvested from the patient himself or herself, using a 10-cc Luer Lok syringe, attached to 3-mm canula, with multiple (8–12) distal side openings, with 10-, 15-, or 20-cm length, according to the harvesting site. In children weighing less than 25 kg as well as in women with relatively thin thighs, the authors prefer 20-cc syringes and 2.5-mm cannulas, also multiperforated distally. These cannulas will enforce a higher negative pressure and assure a more even and efficient fat harvesting, respectively. Occasionally, in very small patients (the authors’ smallest patient weighted 9.170 kg [an electrical injury to the hand]), it may be necessary to harvest fat from more than 1 donor site.
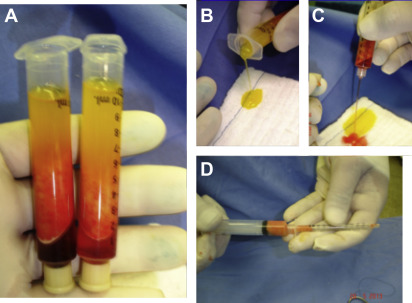
As recommended by Coleman, 1 or more distally plugged 10-cc syringes containing the obtained fat is centrifuged at 3000 rpm for 3 minutes on a 45° angle centrifuge (1200 g ). The obtained compound has a top layer of oil, a middle layer of fat (with the Stromal Vascular Fraction within at its lower portion), and an aqueous inferior layer. The top layer of oil is discarded while the plug still is on the syringe. The plug is then removed, and the aqueous layer drains out by gravity. The remaining compound is sequentially injected in an anterograde manner into “insulin” syringes without the plunger, which is then replaced ( Fig. 1 ).
Fat Grafting
Using a 16-gauge needle, a perforation is made at an acute angle in healthy skin in the periphery of the wound or the scar. A 1.2-mm outside diameter 70-mm-long cannula already connected to a Luer Lok 1-cc syringe is inserted through the needle puncture hole and (forcefully, if needed) driven immediately under the wound bed or the scar. Fat is then deposited in a retrograde manner, in several “passes” until the entire area is grafted (via as many puncture sites as needed around the periphery of the scar or wound). On average, 1.8 to 2.5 cc of fat are injected per each 10-cm 2 area, and it is necessary to make 25 to 30 “passes” to inject 1 cc.
After the wound area has been completely (under)grafted, the surface of the wound is thoroughly debrided, and fat is deposited in quantity to cover the entire wound. If bone (with or without periosteum), tendons, or nerves are already exposed or exposed after debridement, fat is delivered directly over any or all of these structures. The authors usually debride the wound only after the undersurface has been grafted because in doing so, they avoid having to do multiple punctures around a bleeding wound or running the risk of moving debris along with the injection cannula under the wound.
Similarly, in scar areas, fat also treated by the Coleman technique is injected immediately under the scar. After fat grafting is complete, the scar surface area is treated with a derma roller (usually with 0.5–1.5-mm needle length), or the scar surface may be treated with a fractional CO 2 laser, opening “pores” or holes, through the epidermis, into the substance of the scar. Centrifuged fat is then delivered directly to the treated surface (on average, 2.2–3 cc/10 cm 2 ; Figs. 2 and 3 ).


Very frequently, partial scar removal and fat grafting/fat delivery will be associated. In these cases, the authors perform the partial scar resection first, keeping the resection within the scar substance (trying not to go into subcutaneous tissue). A running nylon suture closes the surgical wound. Surprisingly, these patients, originally healed from a facial burn with variable amounts of hypertrophic scarring, will NOT hypertrophy at the suture line within the hypertrophic scar. This fact is attributed to the local effect of the fat grafting and the delivered fat previously treated by the Coleman technique ( Fig. 4 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree