In this article the authors introduce a compartment-based fat graft for facial contouring, focusing on the anatomy of temporal region and midface, the 3L3M integrated fat transfer technique, and the facial compartment-based fat injection in the face. This article includes details of pre-evaluation methods, results of cases, and postoperation care. Readers will have a clear view of how to do facial contouring fat graft in the face after reading this article. There seldom are complications while using the 3L3M technique for fat grafting. The targeted fat grafting can lead to steady and efficient results.
Key points
- •
Targeted restoration of the facial fat compartments allows for safe, reproducible, and effective outcomes of facial contouring.
- •
The authors advocate grafting fat tissue first into the deep plane (deep facial fat compartments) and then the superficial plane (superficial fat compartments), the medial part and then lateral part, and the upper side and then lower side.
- •
Better volume augmentation is based on more living fat graft transfer provided; thus, the authors use the 3L3M technique to get more living fat granules to fill the soft tissue.
Video content accompanies this article at http://www.plasticsurgery.theclinics.com .
Introduction
Facial volume loss in both bony and soft tissues results in hollowness and skin ptosis, which leads to concave facial contour, a deepened nasolabial fold, and midcheek groove, conveying an old and gaunt appearance. Autologous fat grafting is a well-accepted technique for soft tissue augmentation and has been advocated for facial contouring and body shape remodeling. There is no consensus in the literature, however, regarding the fat grafting technique, including the entry site for the cannula and the plane for fat placement. Historically, various fat grafting techniques have been developed and applied in clinical conditions and yield promising results, such as structure fat grafting (Coleman technique), the 3M3L technique, cell-assisted lipotransfer, and nanofat grafting. These techniques focus mainly, however, on the methodological aspects of fat harvesting, refining, and grafting skills in general.
Clinical observation and patient feedback reveal that long-term outcomes of fat grafting are diverse in different recipient sites, especially in the temporal region, one of the subunits with the lowest satisfaction rate after facial fat grafting. The authors believe the diversity of long-term outcomes of fat grafting is a result of different anatomic characteristics in different recipient sites that may directly influence grafted fat survival, neurovascular injury incidence, and fat tissue retention.
Based on these considerations and anatomic studies in the temporal region, midiface, and hand, the authors developed a concept of targeted fat grafting technique, which advocates targeted restoration of physiologic distribution and volume of fat compartments using anatomically adequate cannula entry sites and injection planes. The authors’ previous clinical studies have demonstrated effective and safety profiles in facial contouring, temporal hollowing augmentation, and hand rejuvenation and suggested more applications in other regions.
Preoperative evaluation and special considerations
Each patient should be evaluated for general medical conditions in addition to some special preoperative evaluations, listed as follows:
- 1.
Multiangles of standard photos—frontal, lateral, 45° lateral, 90° lateral, head up and head down, and some special angles—that can fully display the defect of face should be taken before operation. The photos can be printed to show patients where to fill and how thick they need to fill.
- 2.
Three-dimensional (3-D) laser scan and 3-D volumetric analysis can be used to evaluate the symmetriy of the 2 sides of the face. The facial models are analyzed with corresponding analyzing software to quantify the volume discrepancy before graft, determining the quantity of the fat to inject.
- 3.
For some pathologic soft tissue defects, such as radiation damage, scleroderma, and so forth, the skin may not have enough elasticity and be very tight or thin. The authors ask patient to stretch the skin for approximately 1 month to 3 months with small vacuum instruments or other tools to improve the recipient space.
- 4.
CT scans may be used for Romberg disease patients at their first visit to make sure the atrophy degree of bone, muscle, fat tissue, and the occluding relation of their teeth.
The authors propose communicating well with each patient before operation for good compliance. Fat graft absorption is inevitable for every patient, especially during the first 3 months. To reach the final satisfactory results, patients may have injections 2 times to 3 times, with each time needing a 3-month to 6-month interval.
Surgical procedure
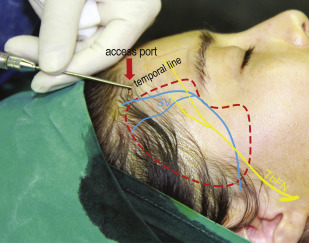
See [CR] . Before liposuction, the authors usually ask patients where the fattest part of their body is and for which part they most want to decrease the fat volume. Elderly women usually have fatty belly where abundant fat is easy to be suctioned. For young patients who do not have bigger belly, the authors prefer to get fat from their bilateral gluteal groove, which may have benefit for them to lift the most protruding point of gluteal and elongate the leg.
The second reason for harvesting fat from lower body position is because α-2 receptors located in diet-resistant areas such as the lateral thighs buttocks, and abdomen. The following are the procedure of 3L3M fat graft technique.
- 1.
Fat graft harvest: the total fat volume the authors use is no more than 100 mL for facial contouring purposes; thus, the authors prefer harvesting fat ‘Manually’ or ‘syringe suction’. The composition of tumescent anesthetic fluid is 0.08% lidocaine plus 1:500,000 epinephrine. After injecting tumescent for several minutes, the authors use a 20-mL syringe for hand liposuction. The authors keep 5 mL of air in the syringe before drawing back the Plunger pod and fixing it with a clamp or clip to create less negative pressure. The slower and gentler suction causes less oil from harvest fat. The authors may choose suction cannula with multiple side holes to do effective suction; the diameter of the side hole is chosen depending on the purpose of filling. For example, if volume augmentation and injecting to a deep layer are needed, a relatively larger hole, such as 2 mm to 3 mm, may be chosen. If injecting superficial layer or performing some subtle injection, the authors prefer smaller side holes to do suction.
- 2.
Fat graft process: after acquiring fat, the authors use saline to wash away lidocaine, epinephrine, cell debris, and red blood cells. Lidocaine and epinephrine, which contain the tumescent, are reported to reduce the viability of adipocytes. Then, the authors stand the syringe with fat and saline for a while, until the lowest part of liquid looks relatively clear, which means there are fewer small adipocytes suspension in the liquid part. Thin patients may have more fibers than fat patients. Fibers in the harvested fat are cut into pieces before low-speed centrifugation. The fat samples are centrifuged at low speed, less than 100 g, for 2 minutes to 3 minutes. After centrifuge, the lowest liquid part is ejected out and then a 3-way or 2-way pipe connected to the 20-mL syringe to transfer the middle layer of fat into a 2-mL or 1-mL syringe. The top layer of oil is left in the syringe and used to lubricated inject cannula. The whole procedure is controlled at 25°C within 30 minutes to 60 minutes.
- 3.
Recipient site preparation: Good design for patients should be done before surgery. 3-D simulation or photos can help both surgeon and patients to make a decision. Make sure the recipient site is not injected with any other fillers, such as hyaluronic acid, collagen, and so on) or not use any enzyme to dissolve the fillers within 6 months. Make sure the skin has no infection (such as infectious acne) or ulceration, and the skin should have good elasticity to strut enough room for fat graft ( Figs. 1–6 ).
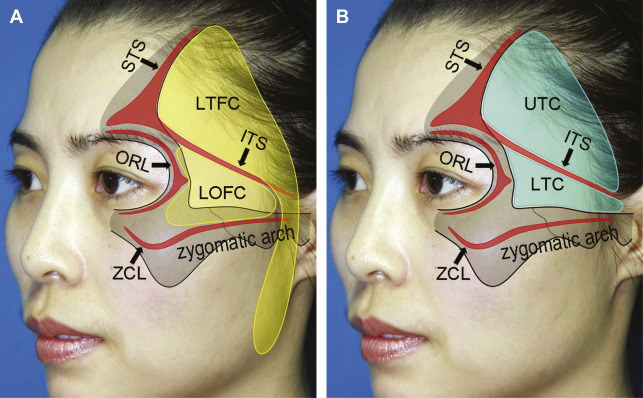
Fig. 1
Surface projection of fat compartments ( A ) and septum compartments ( B ) in the temporal region as demonstrated on a 37-year-old female patient. ITS, inferior temporal septum; LOFC, lateral orbital fat compartment; LTC, lower temporal compartment; LTFC, lateral temporal cheek fat compartmentORL, orbital retaining ligament; STS, superior temporal septum; UTC, upper temporal compartment; ZCL, zygomatic cutaneous ligament.
( From Huang RL, Xie Y, Wang W, et al. Anatomical study of temporal fat compartments and its clinical application for temporal fat grafting. Aesthet Surg J. 2017;37(8):858; with permission.)
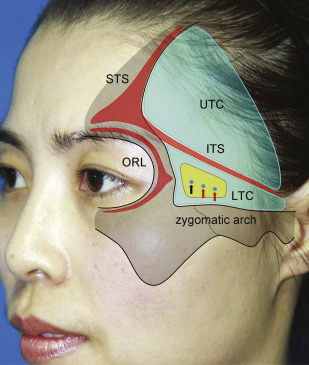
Fig. 2
Surface projection of the zone of caution as demonstrated on a 37-year-old female patient. The zone of caution is located in the lower temporal compartment at its anterior half, where the sentinel vein and branches of the middle temporal vessels perforate the temporal fascia and travel in the subcutaneous tissue layer (see arrows). ITS, inferior temporal septum; LTC, lower temporal compartment; ORL, orbital retaining ligament; UTC, upper temporal compartment; STS, superior temporal septum.
( From Huang RL, Xie Y, Wang W, et al. Anatomical study of temporal fat compartments and its clinical application for temporal fat grafting. Aesthet Surg J. 2017;37(8):859; with permission.)