9 Osseous Lesions of the Craniofacial Region
Summary
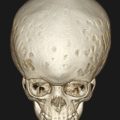
Osseous lesions in the craniofacial region can be discovered in a variety of clinical and radiological scenarios and often present as facial asymmetry or as a disturbance in growth such as tooth eruption. Having a broad understanding of the range of lesions that can occur in this area of the body is critical given that benign lesions can often be destructive and result in significant morbidity. Early diagnosis and a multidisciplinary team approach is often warranted in order to optimize results for the growing child.
9.1 Introduction
Osseous lesions in the craniofacial region can be discovered in a variety of clinical and radiologic scenarios. Most commonly, when a pediatric patient is found to have a facial asymmetry or a mass, initial consultation is with a plastic surgeon or a maxillofacial surgeon. Having a broad understanding of the range of lesions that can occur in this area of the body is critical to understanding appropriate workup and surgical management. Because of the intimate association of lesions in this area with vital structures such as the jaw, sinuses, orbits, and ears, a multidisciplinary team approach is often warranted.
In this chapter, we classify osseous lesions of the craniofacial region broadly into cysts and tumors and further subdivide these lesions into odontogenic and nonodontogenic cysts and tumors.
9.2 Odontogenic Cysts
Most commonly, odontogenic cysts and lesions are discovered when there is radiographic investigation for asymmetric or delayed eruption of adult teeth. It is important to know the timing of eruption, and if there is significant delay between the right and left sides, then a radiologic examination is necessary. The most common finding is a cyst associated with an impacted and displaced tooth. Odontogenic cysts are broadly divided into inflammatory and developmental cysts.
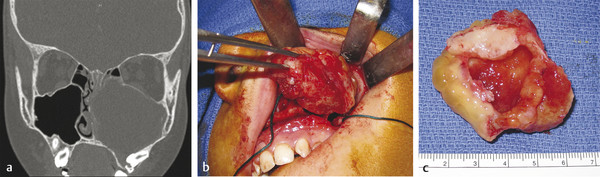
In the pediatric population, the most common developmental cyst is a dentigerous cyst associated with an impacted canine, a premolar, or a molar such as the third molar (Fig. 9‑1a). On a radiograph, there is a well-circumscribed, unilocular radiolucency associated with the crown of an unerupted tooth attached at the cementoenamel junction (CEJ). The cyst can cause tooth displacement, and the treatment consists of enucleation of the cyst and, in most cases, removal of the impacted tooth (Fig. 9‑1b, c).
The odontogenic keratocyst and the adenomatoid odontogenic cyst were previously considered developmental cysts but are no more considered tumors. They are now known as keratocystic odontogenic tumor (KCOT) and adenomatoid odontogenic tumor (AOT) and will be discussed in the section on odontogenic tumors.
9.2.1 Inflammatory Cysts
Inflammatory cysts are often associated with a nonvital tooth and are painful on palpation and percussion. They can be asymptomatic if the lesion is chronic in nature and are usually associated with the roots of a nonvital tooth or a tooth with a large carious lesion. Treatment often involves root canal therapy of the tooth or extraction, with enucleation of the granulation tissue within the cyst.
9.2.2 Buccal Bifurcation Cyst
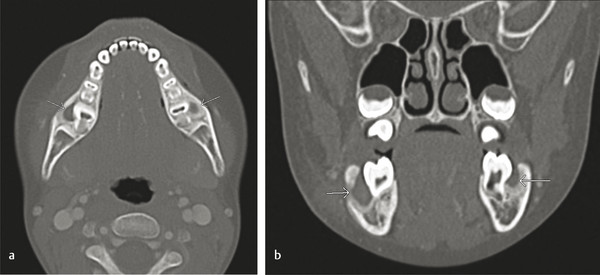
The buccal bifurcation cyst (BBC) is inflammatory rather than developmental and usually develops on the buccal region of vital mandibular first or second molars (Fig. 9‑2). It is usually seen in children between the age of 5 and 15 years. Treatment options include curettage of the lesion with daily irrigation or enucleation and removal of the tooth. They can become secondarily infected and may require antibiotics and surgical drainage of the surrounding tissue.
9.3 Nonodontogenic Cysts
The most common nonodontogenic cyst in childhood is the traumatic or simple bone cyst (SBC). Typically, the patient has an asymptomatic radiolucent lesion of the mandible, with no clinical swelling or any other abnormalities on examination (Fig. 9‑3). The lesion favors the male population and presents in the first two decades of life. The radiographic imaging warrants surgical exploration and curettage in order to rule out an epithelial lined cyst or tumor. The clinical finding is an empty bony cavity with very little tissue, if any, to submit to pathology. If the lesion is large enough or near the condylar head, a bone graft may be warranted, but typically, after curettage of the bony wall, the lesion will fill in with normal bone over time.
9.3.1 Aneurysmal Bone Cyst
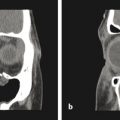
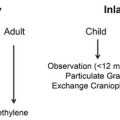
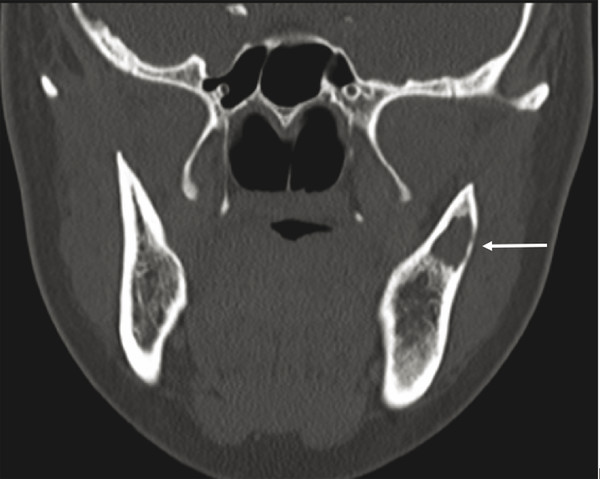
Another similar radiographic presentation to a traumatic bone cyst is the aneurysmal bone cyst (ABC). This lesion tends to favor the female population, and often, there can be jaw swelling and pain. The most common type is the vascular type, which can be rapid growing and destructive (Fig. 9‑4a, b). Unlike a traumatic bone cyst, on entry of this lesion, you will encounter brisk bleeding, which is controllable with pressure and resolves with curettage of the lesion (Fig. 9‑4c–e). Aneurysmal bone cysts tend to have a recurrence rate of 10% and are part of a spectrum of vascular lesions; these cysts are associated with jaw tumors.
9.3.2 Nasopalatine Duct Cyst
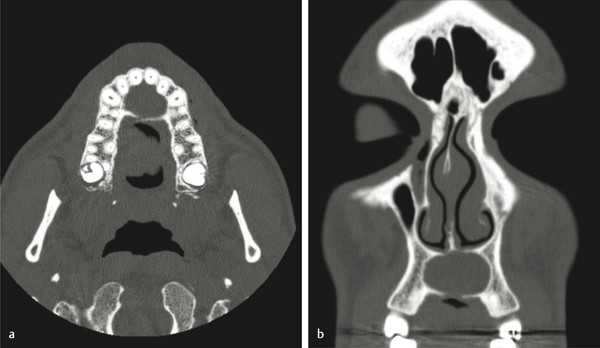
Finally, the nasopalatine duct cyst (NPDC) is a nonodontogenic developmental cyst that is usually found incidentally in the anterior maxilla in the area of the incisive canal. It can become painful, especially if secondarily infected. Radiographically, on an occlusal plain film radiograph, one finds a midline heart-shaped unilocular radiolucency. The lesion often is symmetric and is present in the anterior maxilla along the length of the incisive canal (Fig. 9‑5). Treatment comprises enucleation and curettage, with recurrence being very rare.
9.4 Odontogenic Tumors
Odontogenic tumors are common in children because of the natural course of tooth development of the adult teeth, leading to eruption of the adult teeth and exfoliation of the deciduous teeth. As a result, the most common clinical signs of an odontogenic lesion are asymmetric tooth eruption and alveolar bone asymmetry.
9.4.1 Odontoma
The most common odontogenic tumor of the jaws is the odontoma. There are two types of odontomas: compound and complex. The compound odontoma consists of multiple toothlike structures surrounded by a radiolucent zone, whereas the complex odontoma is a radiodense mass made up of enamel and dentin without toothlike structures and is surrounded by a radiolucent zone. The mean age of people found with odontoma is 15 years, and odontomas are often asymptomatic and found on routine dental radiographs. They may cause delayed eruption of teeth. Clinically, they are typically well-circumscribed dense masses that can be treated with simple surgical excision that must also include complete removal of associated soft tissue, follicular tissue, or cyst. Prognosis is excellent, without recurrence (Fig. 9‑6).

9.4.2 Cementoblastoma
Similar to odontomas in appearance, cementoblastoma tends to appear radiographically in patients younger than 20 years as a round radiopaque mass fused to the roots of vital teeth (Fig. 9‑7). This is a rare benign tumor of odontogenic origin and is treated with surgical excision of the mass and the affected tooth or teeth, followed by curettage or peripheral ostectomy. Cementoblastomas tend to recur if not completely removed, with reported recurrence rates near 40%.
9.4.3 Keratocystic Odontogenic Tumor
The keratocystic odontogenic tumor is a benign intraosseous cystic tumor of odontogenic origin, and it can be locally destructive. Majority of the lesions occur in the posterior mandible, with bony expansion and tooth displacement. Depending on the size and location, small lesion can be treated with enucleation and peripheral ostectomy, whereas larger KCOTs should be first decompressed, enabling the placement of a stent, followed by daily irrigation for 9 months, which reduces the lesion’s size and causes dedifferentiation of the residual epithelium, thus enabling cystectomy. It has lower recurrence rates of around 10% (Fig. 9‑8). This is useful in children with multiple lesions and or lesions that are in close proximity to vital structures such as the inferior alveolar nerve. Finally, marginal or en bloc resection can be utilized for large, recurrent lesions. Recurrence rates range between 10 and 55%, with enucleation alone having the highest rate.

9.4.4 Nevoid Basal Cell Carcinoma Syndrome
When multiple KCOTs are present, the child must be further worked up for nevoid basal cell carcinoma syndrome (NBCCS), also known as Gorlin–Goltz syndrome. Keratocystic odontogenic tumors occur in 75% of patients with NBCCS. Keratocystic odontogenic tumors that occur as a part of this syndrome tend to have a higher recurrence rate.
9.4.5 Adenomatoid Odontogenic Tumor
The adenomatoid odontogenic tumor is a benign cystic hamartoma that is known as the “two-thirds” tumor, because about two thirds occur in maxilla, two thirds occur in young women (preteenagers and teenagers), two thirds are associated with impacted tooth, and two thirds of those teeth are canines. They can become very large and radiographically appear as a well-demarcated, unilocular radiolucent lesion usually associated with an impacted tooth. Treatment involves direct exploration and enucleation, ensuring that the capsule is intact upon removal. Recurrence is rare.
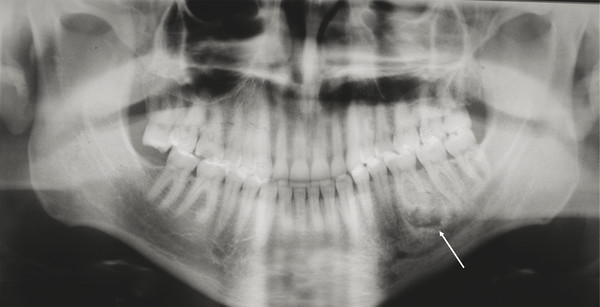
9.4.6 Ameloblastic Fibro-odontoma
Ameloblastic fibro-odontoma (AFO) is usually seen in teenagers as an asymptomatic jaw expansion that may resorb adjacent teeth. It has a mixed radiolucent–radiopaque presentation and is radiographically similar to a developing odontoma (Fig. 9‑9a). Majority of these tumors are found in the posterior mandible and are often associated with an unerupted tooth. Treatment includes simple enucleation and curettage (Fig. 9‑9b, c). Prognosis is excellent, and recurrence is rare.
9.4.7 Ameloblastic Fibroma
Ameloblastic fibroma (AF) is usually seen between 6 and 15 years of age and usually presents as an asymptomatic expansion of the jaw in the molar region of the mandible. It can be of unilocular or multilocular radiolucency, occurs most commonly in the mandible, and is associated with an impacted tooth (Fig. 9‑10). Because it may have a similar appearance to other large destructive lesions, an incisional biopsy should be performed in children as an AF is treated with simple enucleation and curettage versus a resection for other lesions of similar appearance. Although rare, in some cases, an AF can convert into an ameloblastic fibrosarcoma. There is a significant higher risk of malignant transformation and recurrence in patients older than 20 years. As a result, resection is the treatment of choice in patients older than 20 years, patients with massive tumors, and those who have recurrent ameloblastic fibroma.
Ameloblastic fibrosarcoma is the most common malignant odontogenic tumor and is capable of metastasis. It tends to appear later than ameloblastic fibroma, usually in the 20s. Treatment involves resection by using 1.0 to 1.5 cm bony margins and one uninvolved anatomic carrier.
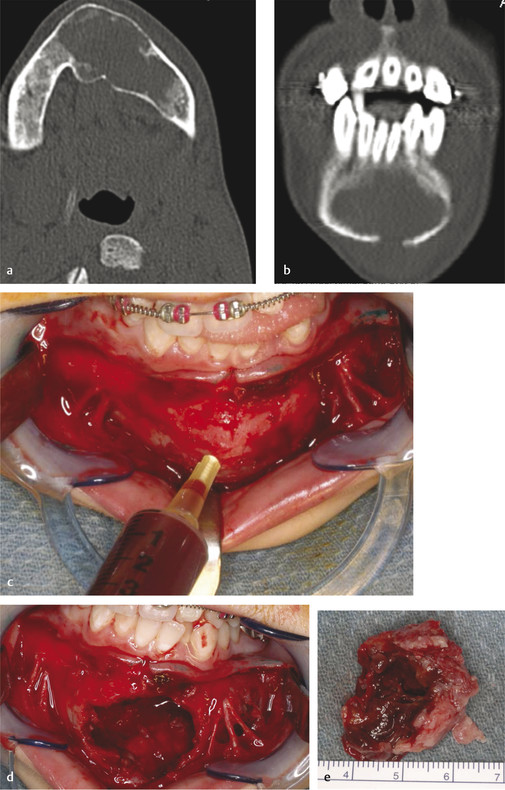
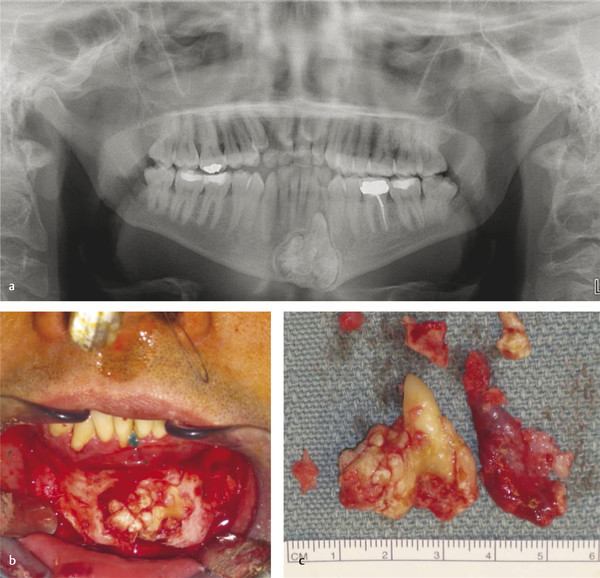
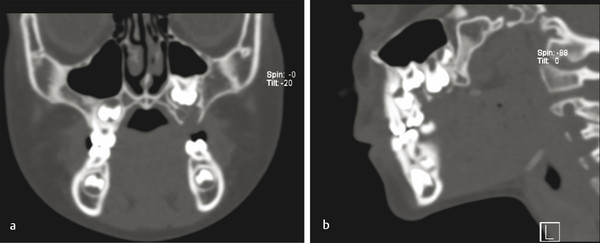
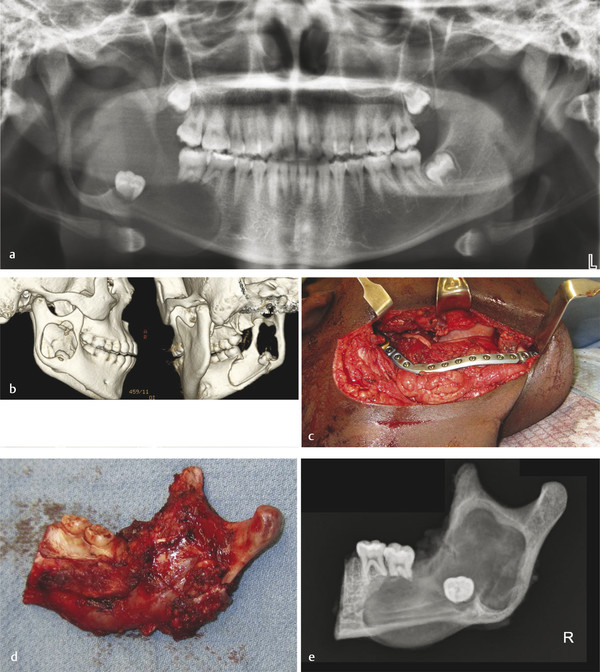
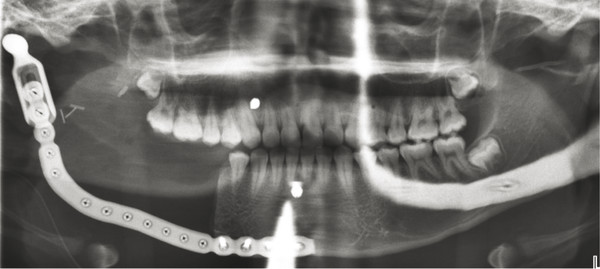
Ameloblastoma is the most common odontogenic tumor, with about 50% of them occurring between 20 and 40 years of age. In the pediatric population, ameloblastoma must be considered in the differential diagnosis of any unilocular or multilocular radiolucency. Unicystic ameloblastoma represents about 5% of all ameloblastomas and tends to occur in younger age range (10–24 years) (Fig. 9‑11a, b). For all ameloblastomas, 80% occur in the mandible and 75% in molar–ramus region. They are benign, locally aggressive, expansile neoplasms that commonly cause dental changes such as mobility, tooth displacement, and root resorption. Untreated tumors can progress to a tremendous size. Treatment involves resection with 1.0 to 1.5 cm bony margins and one uninvolved anatomical barrier (Fig. 9‑11c, d). Consider frozen sections of soft tissue margins as well as taking a radiograph of the specimen to ensure that you have 1-cm margins past radiographic margins (Fig. 9‑11e). Cure rate with resection is about 98%. Controversy exists around immediate reconstruction at the time of resection versus a staged approach. If enucleation and curettage are performed, there is a recurrence rate of more than 80% (Fig. 9‑12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree