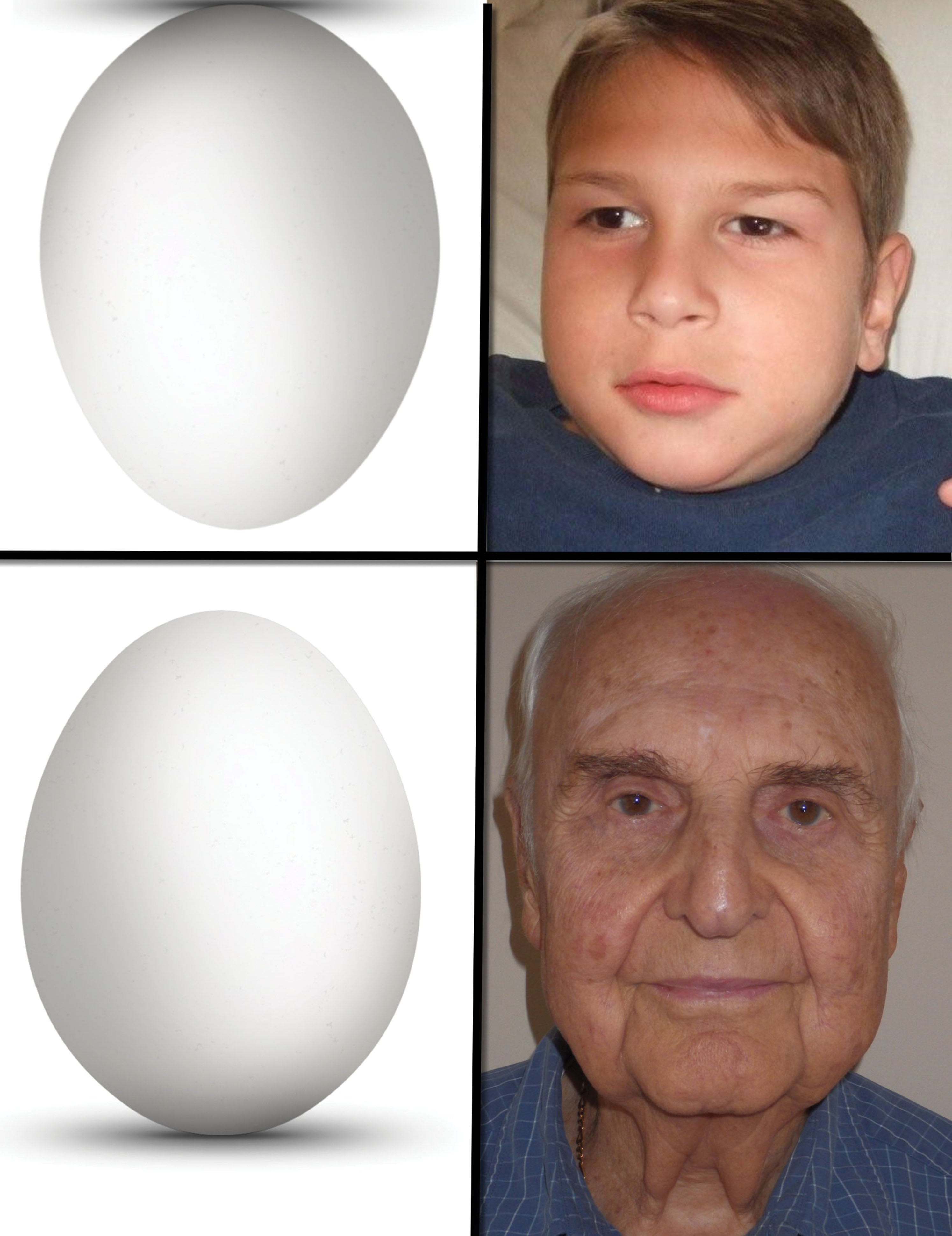
If one were to read this textbook from cover to cover and write down 10 important facts that they have gleaned from these chapters, one of these would be the importance of fat for not only youthful appearance, but also the caution of removing excessive fat during cosmetic procedures. Fat provides youthful volume, and loss of fat causes deflation with aging ( Fig. 15.1 ). Understanding the importance of reducing or augmenting the face and neck with fat is imperative. As highlighted earlier, the youthful face has plentiful midfacial fat volume and tapers to a youthful jaw and neck profile, whereas the aging face becomes deflated, which allows accumulation of fat deposits on the jawline and neck. This deflational shift coupled with other hard and soft tissue changes is in short what produces aging changes.
Numerous intrinsic and extrinsic factors influence the hard and soft tissue changes that occur throughout life. The main goal of rejuvenation is to reestablish the tapered face of youth. Treatment varies depending on the age of the patient. Younger patients may benefit from simple volume inflation with facial fillers and implants, while older patients will require fat removal and sculpting as well as skin tightening or removal. Injectable fillers, facial implants, and fat transfer have been detailed in previous chapters, and the remainder of this chapter will deal with fat reduction, recontouring (sculpting), and augmentation in the face and neck. It is very common for cosmetic surgeons to remove fat in some areas and add fat in other areas in the same procedure.
Anatomy
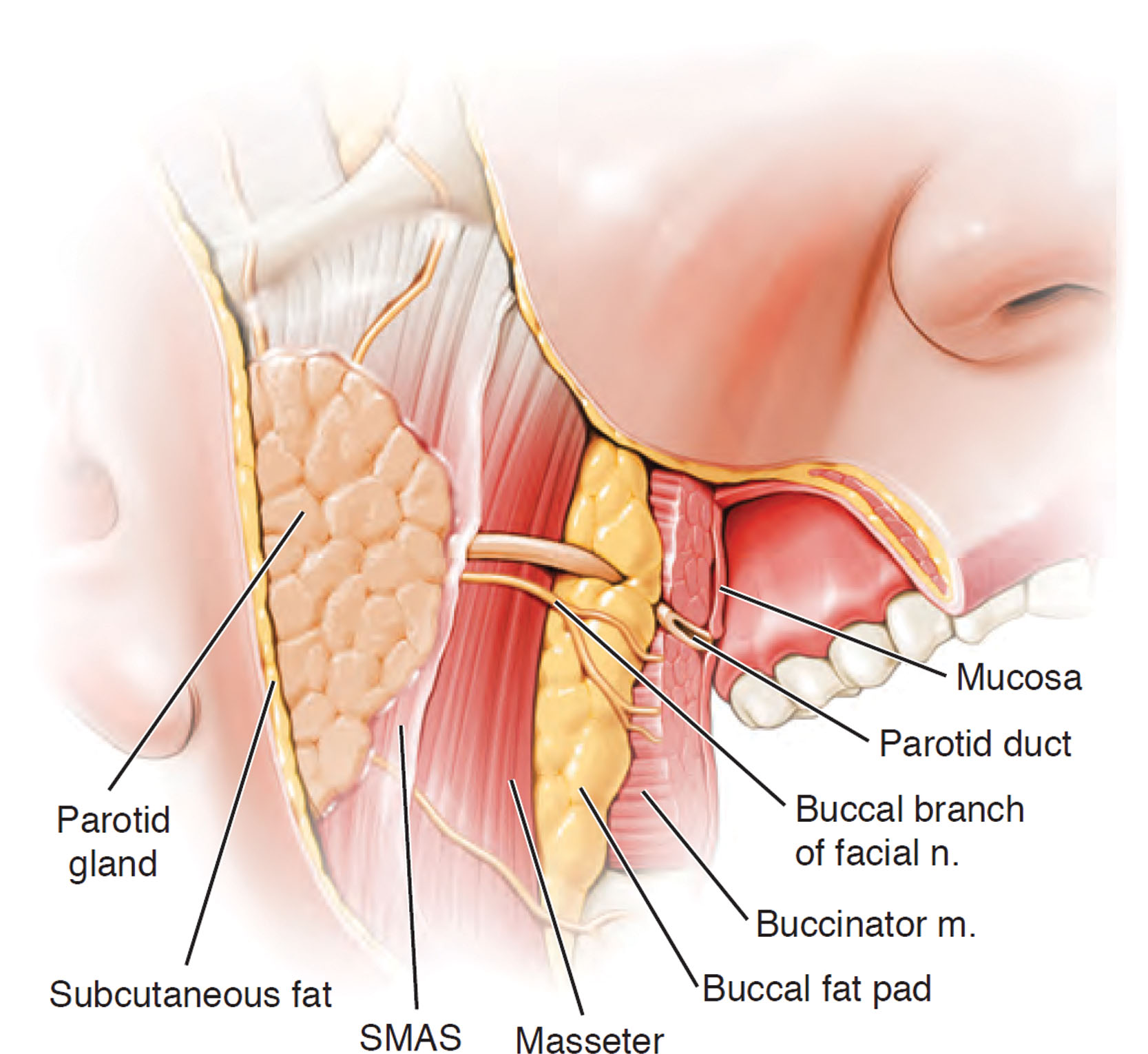
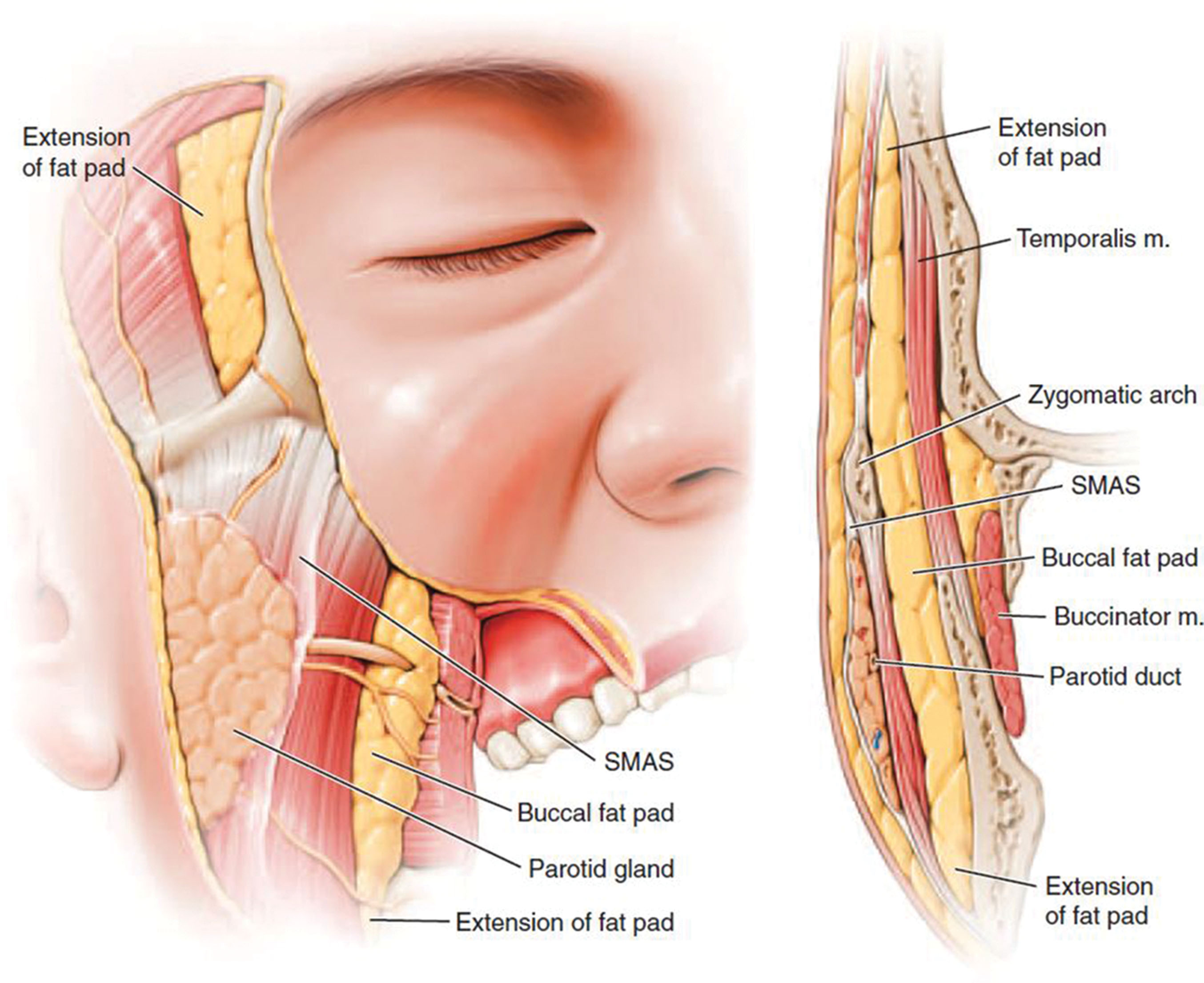
The malar fat pad supplies the majority of youthful midfacial volume and is discussed in Chapter 7 . The buccal fat pad (BFP), also called Bichat’s fat pad , provides facial volume and is a distinct and separate structure from the malar fat pad. Teleologically, the function of the BFP is not singularly defined. Theories include that the buccal fat aids in nursing and also forms a gliding plane to facilitate movement of the masticatory muscles and to cushion and protect the muscles ( Fig. 15.2 ).

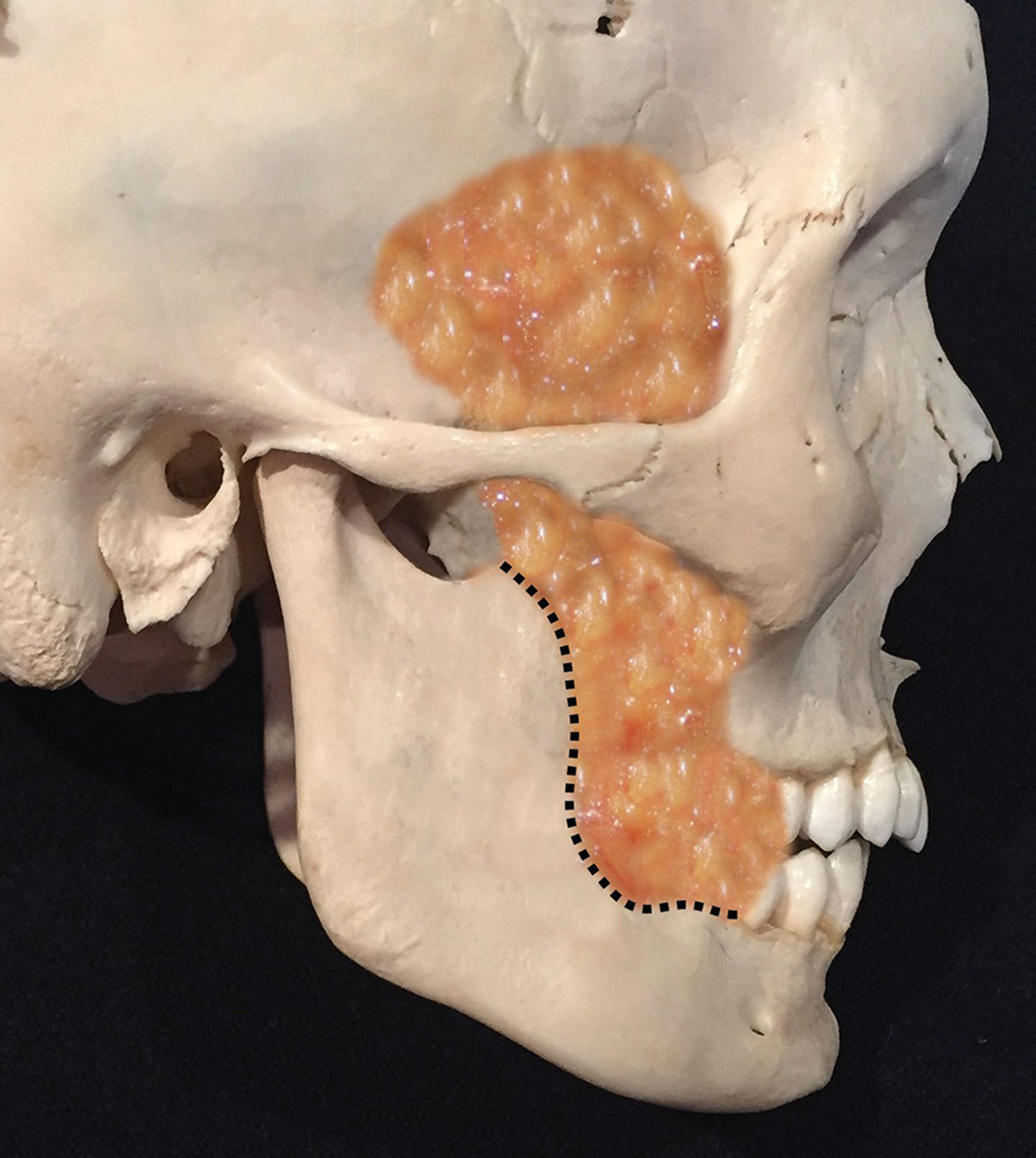
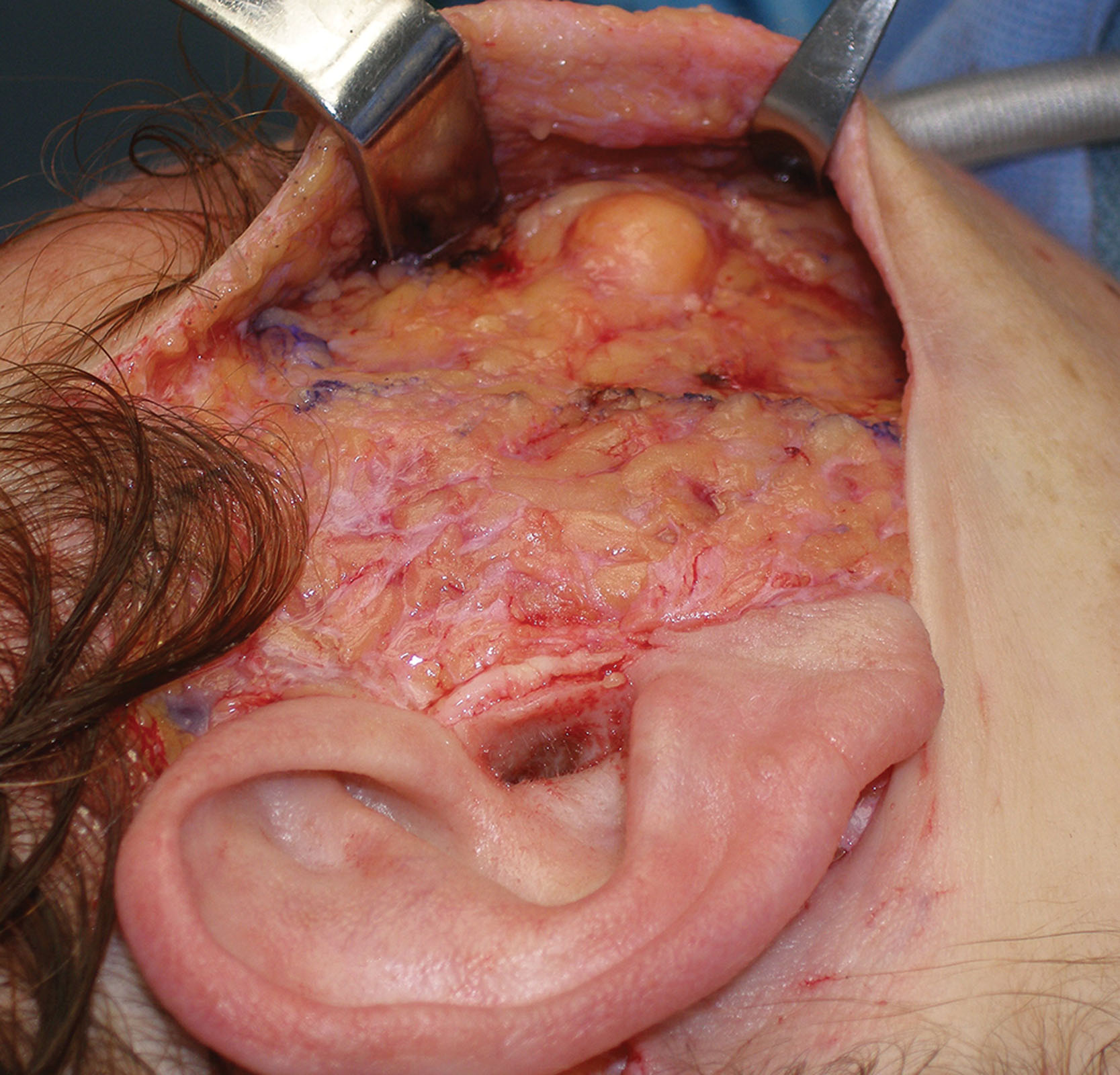
The BFP sits between the buccinator muscle and the masseter muscle and should never be confused with the malar fat pad. The BFP is an encapsulated adipose mass that spans the lateral face from the temporal region to the mandibular region. Depending on the specific text or article, it has three lobes and four extensions. The temporal extension envelops the temporalis muscle on both sides, the body of the pad occupies the space under the zygoma, the pterygoid extension is in the region of the posterior maxilla, and the buccal extension sits inferiorly over the mandible ( Figs. 15.3–15.5 ). The parotid duct pierces the BFP on its intraoral entry ( Fig. 15.3, 15.4 ). The BFP can herniate with aging and can be approached intraorally or through the facelift incision during rhytidectomy ( Figs. 15.7 and 15.8 ).

Diagnosis
Buccal fat reduction (BFR) is a procedure that can assist in reducing facial fat in selected patients. The procedure can assist to trim and taper the cheek area but is not a procedure that will make a fat face skinny. This is an important point as many young patients seek this procedure with the intent to slim their entire face. BFR is more of a precision procedure used to sculpt the cheek area in selected patients. It is requisite for the surgeon and patient to understand the realistic results of BFR. This has become a popular procedure with millennials, and social media has propagated the notion that a chubby face can be “sculpted.” It is not uncommon for some of these patients to think that such a small procedure will give them a face like a fashion model. It is a big mistake to operate on a patient with such expectations. BFR is a procedure that can lure patients with body dysmorphic disorder. The surgical result is obviously related to the size and volume of the BFP. The area of reduction is in the mid to lower cheek ( Figs. 15.8 and 15.9 ).

The importance of what this procedure will do and which areas will be affected is paramount to patient communication as many patients have inflated ideas of what this procedure does. Patients who cannot understand that this procedure is conservative are not operative candidates. This is one procedure in which I always underpromise in terms of results. Sometimes the results are very noticeable, and other times they are very subtle. This is obviously influenced by the amount of buccal fat the specific patient possess.
Contrary to the belief of many patients, the entire BFP is never removed. It is generally the buccal extension and body that is reduced and sometimes a portion of the pterygoid extension. The goal with this procedure is reduction and not ablation. This adipose mass is important in providing youthful facial volume, and overzealous excision will skeletonize the patient.
Although it is not possible to provide a completely accurate prediction of the surgery result, having the patient lightly create a vacuum and slightly suck in their cheeks will produce a concavity in the region of the BFP ( Fig. 15.10 ).

Surgical Procedure
Although this is a simple procedure, the BFP can be very elusive, especially for novice surgeons. Like most of the procedures we perform, the operation becomes easier with experience.
Very similar to blepharoplasty, doctors claiming that the patient does not have a BFP usually translates into they just could not find it. I perform a lot of these procedures, so I can generally find the fat pad in a matter of seconds, however selected cases can be more difficult. I have never not been able to find a fat pad, although in some patients it is much smaller than in others.
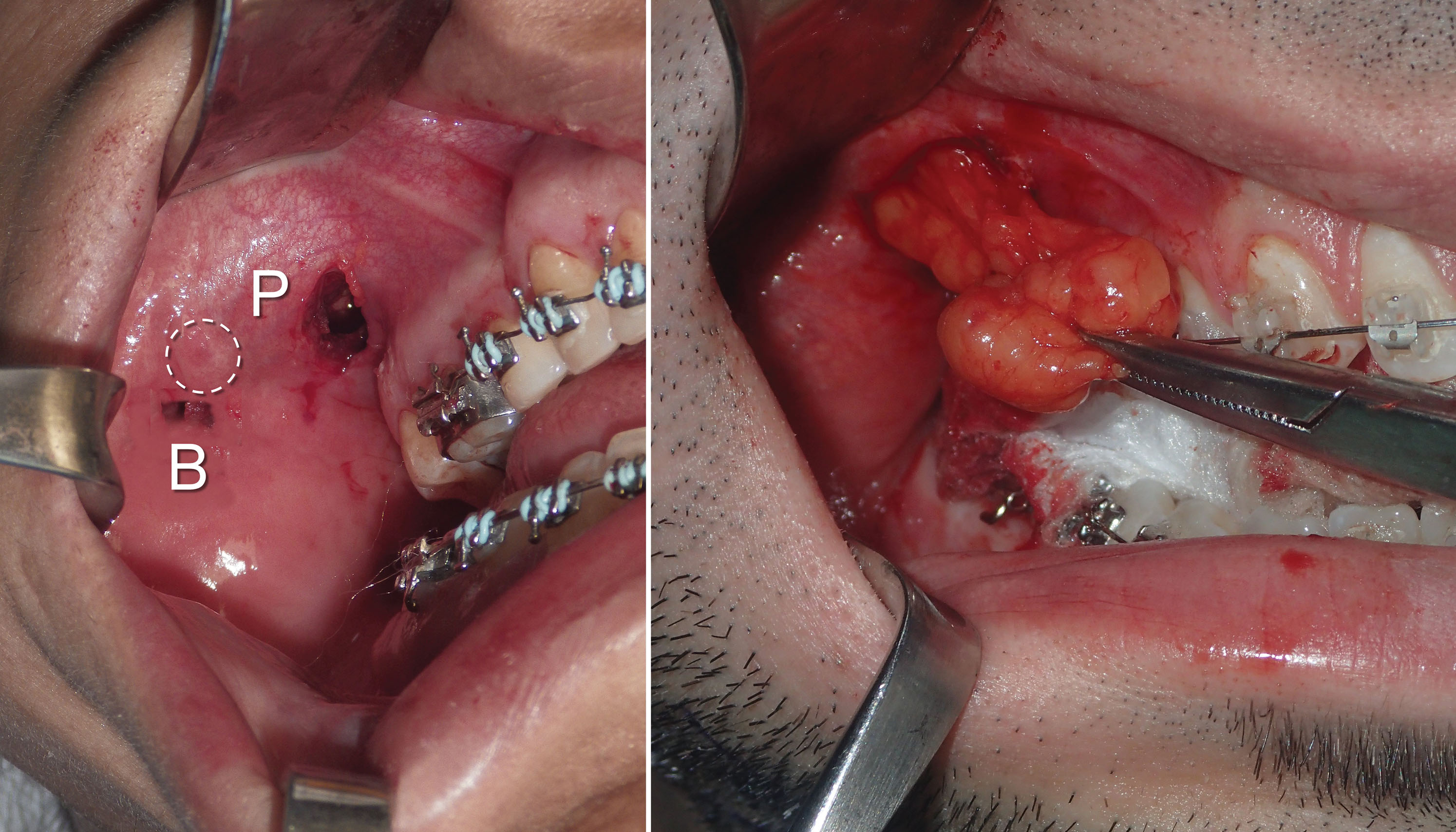
BFR can be easily performed with local anesthesia or intravenous sedation. The first step is to infiltrate the proposed incision site with local anesthesia. Approximately 2 mL of 2% lidocaine with 1:100,000 epinephrine is infiltrated just under the parotid duct (Stenson’s duct) into the mucosa. The duct is located opposite the first molar region on the cheek mucosa. On some patients it is very easy to see, and on others the orifice is more hidden. Several more milliliters of local anesthetic are infiltrated into the buccinator muscle (which is just submucosal) and into the generalized region to be reduced. I prefer to make the incision several millimeters below the parotid duct. In general, the BFP is easily located and reduced, but location can be challenging in some patients,. My first approach is always through the infraductal incision. If the fat cannot be located through this incision, my secondary mucosal approach (pterygoid approach) is more superior and lateral to the second and third molars in the maxillary sulcus.
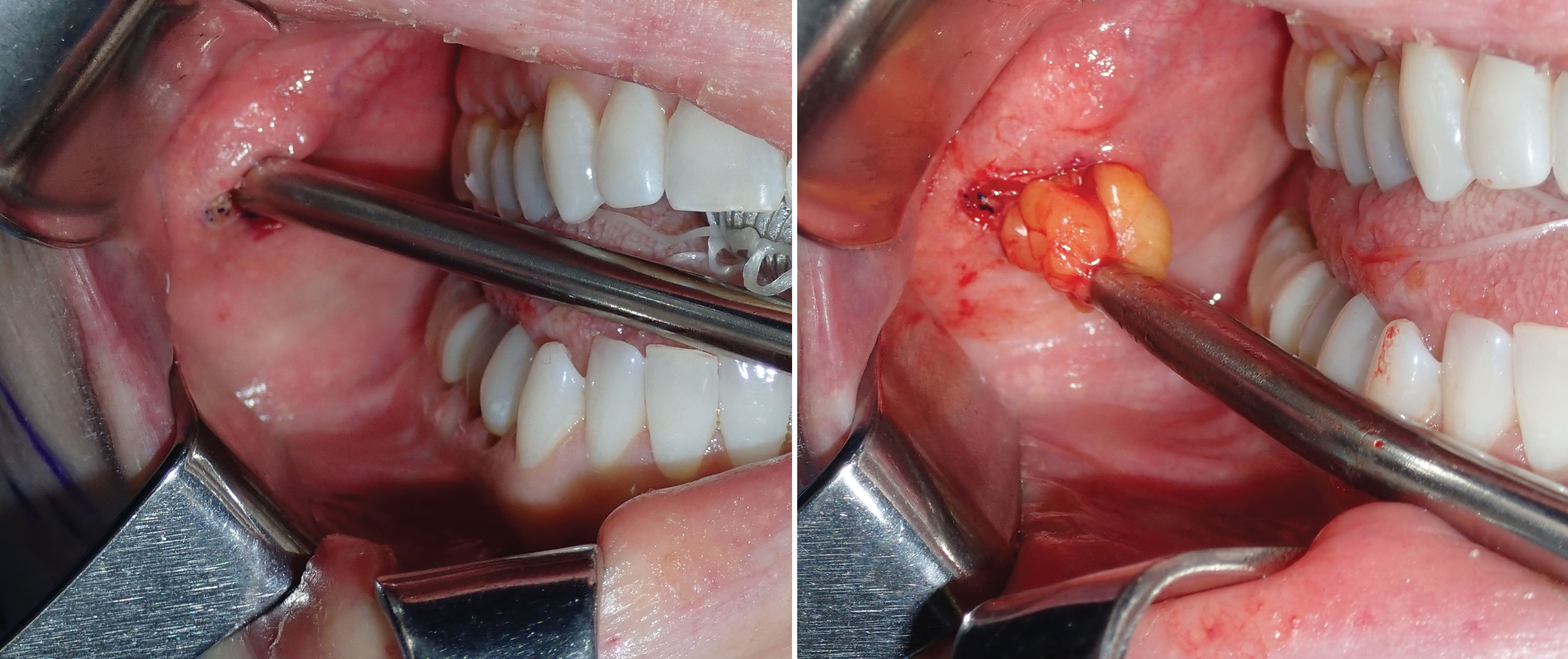
As stated, a 4- to 5-mm-wide incision is made with a radiofrequency microneedle just through the mucosa several millimeters under the parotid duct ( Fig. 15.11 ). This area is very vascular, and a coagulative incision modality is preferred. The actual incision is made only through the mucosa as the vascular buccinator muscle can bleed significantly, and this is sometimes difficult to coagulate. The parotid and buccal branches of the facial nerve traverse the BFP, so blind coagulation is not desirable.
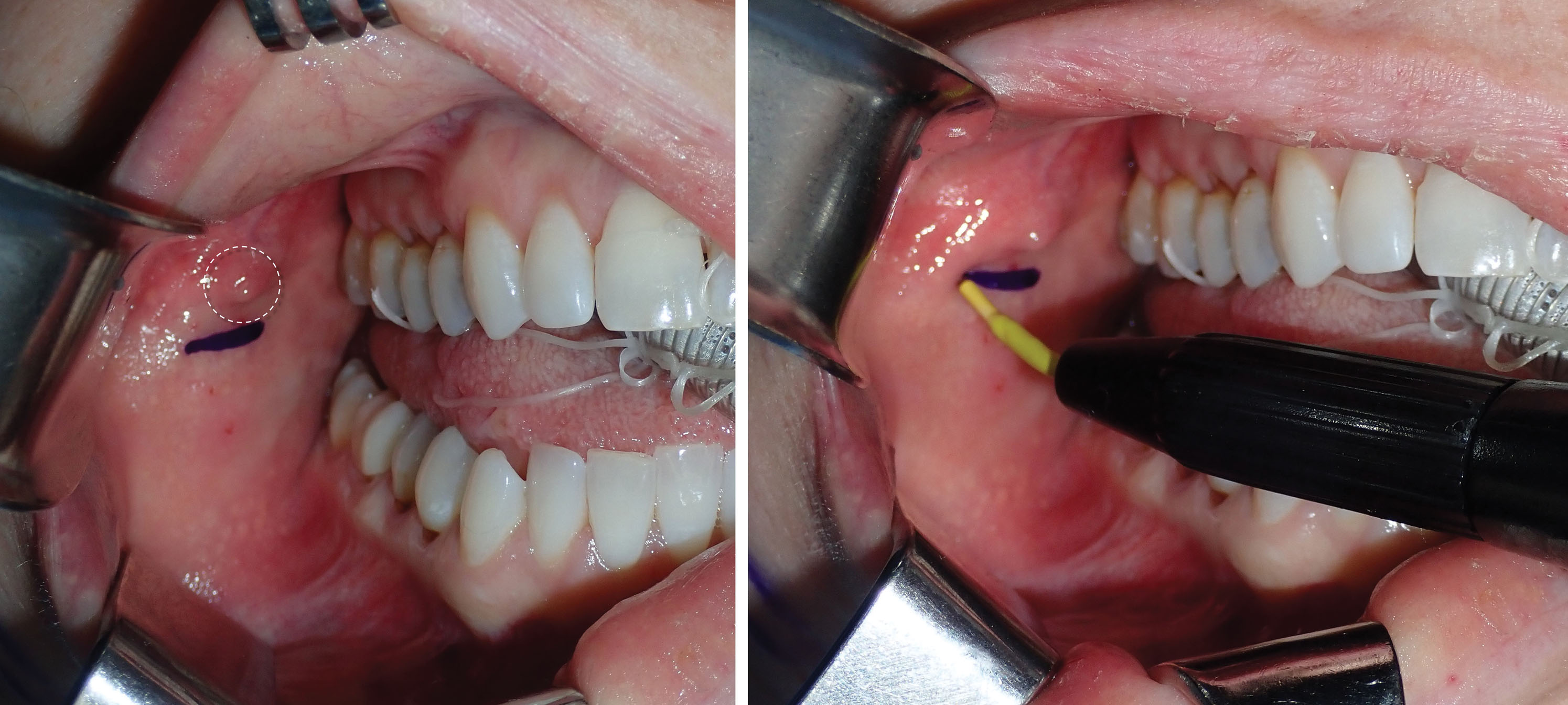
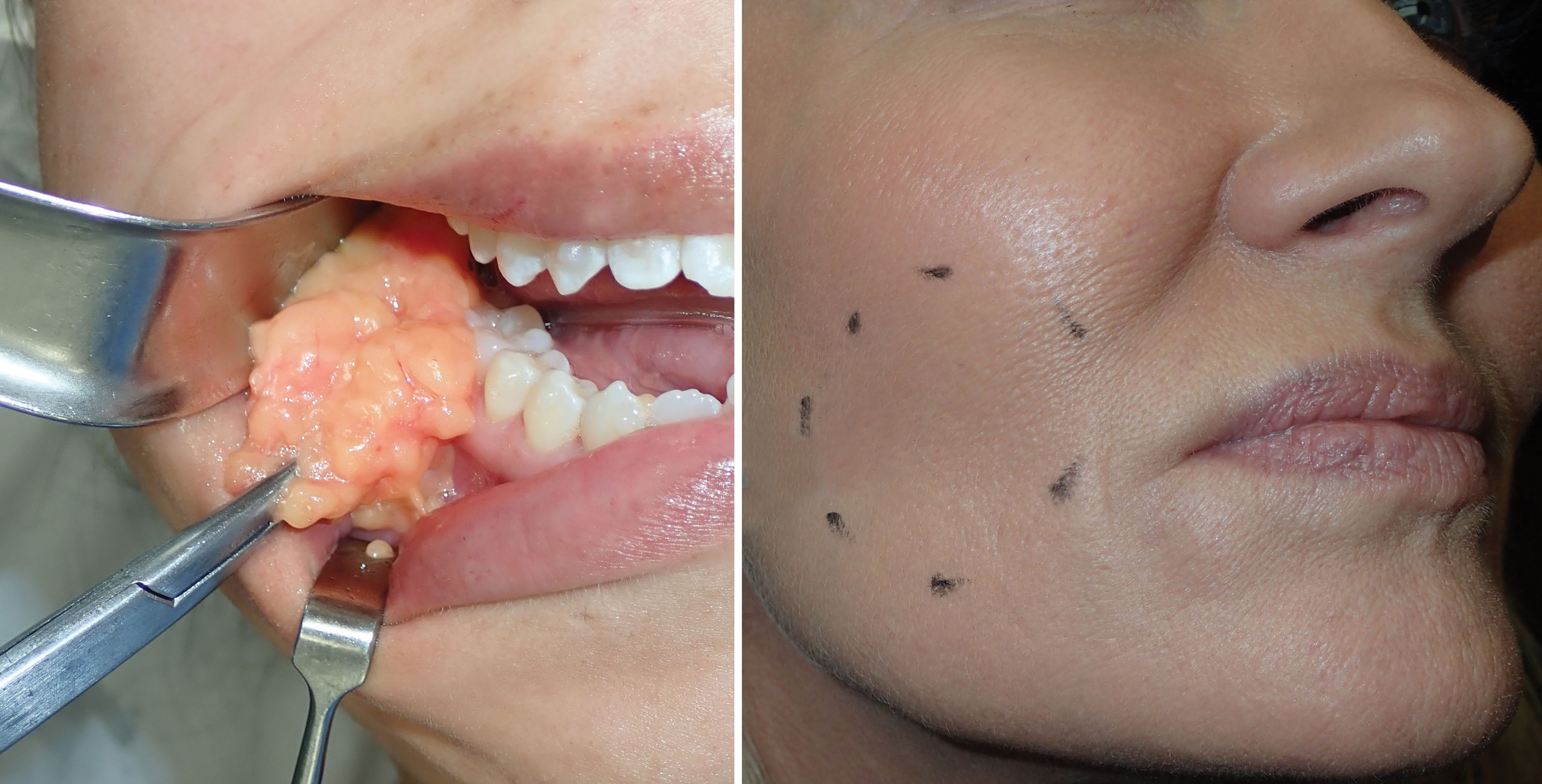
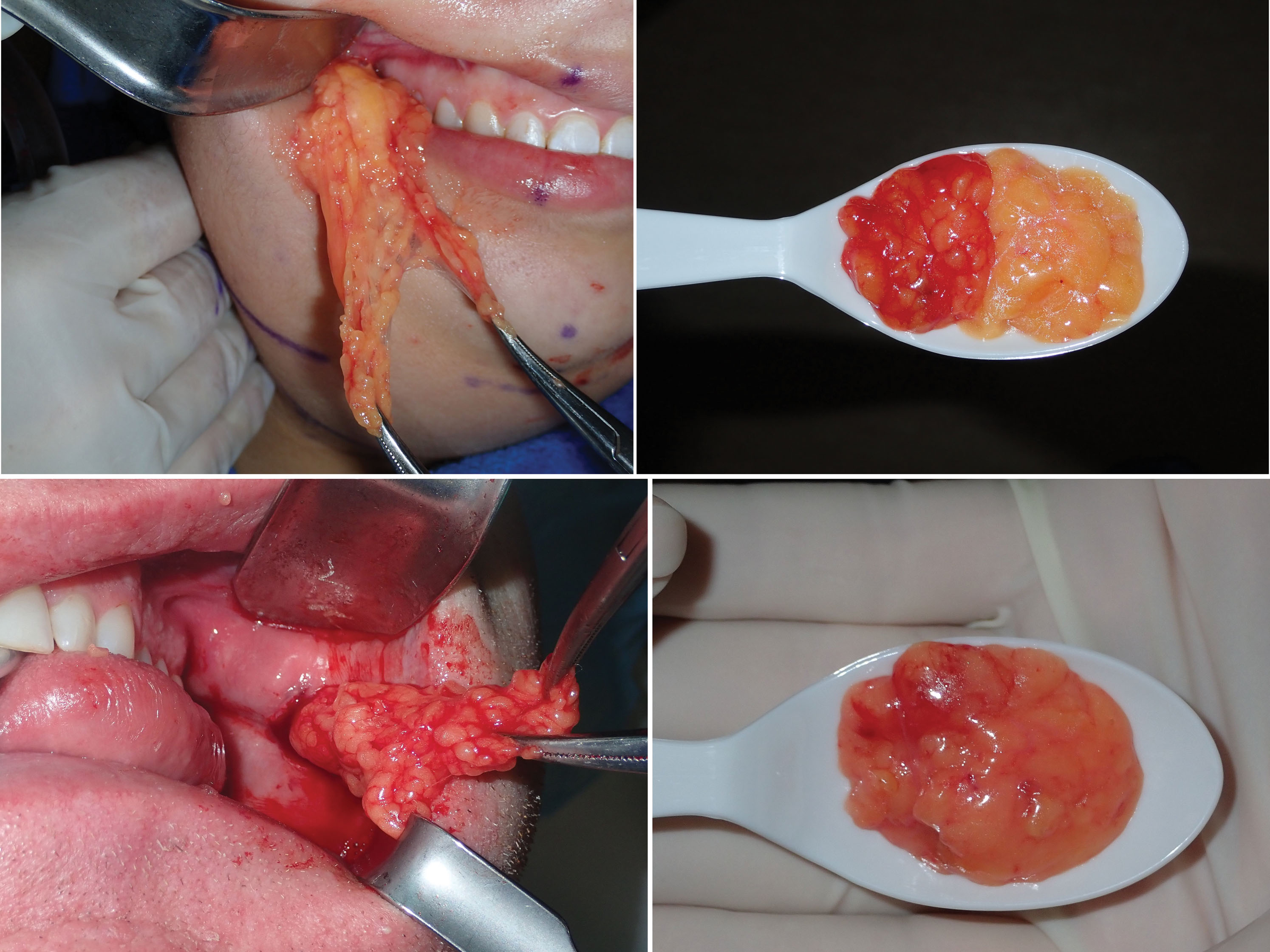
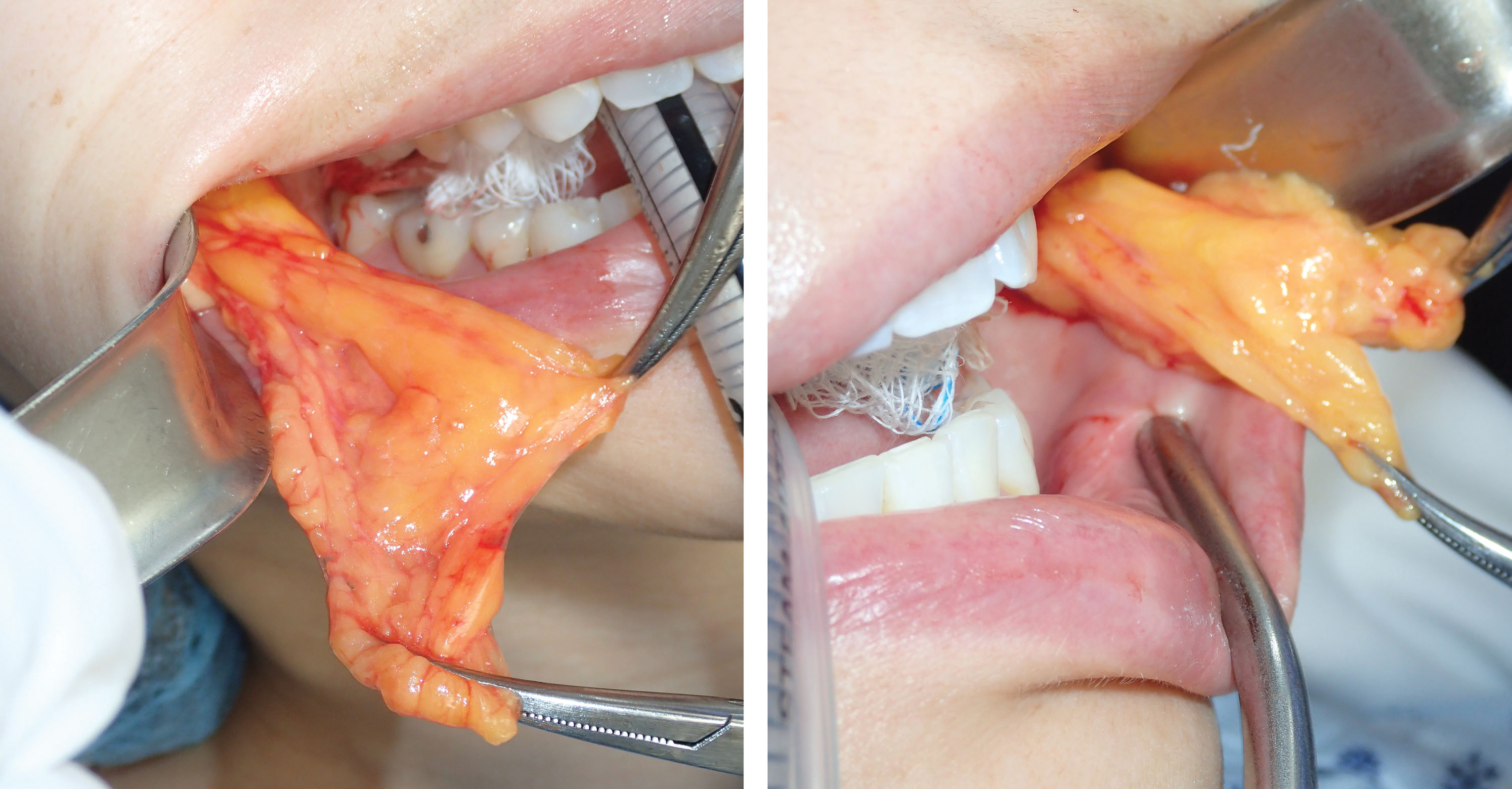
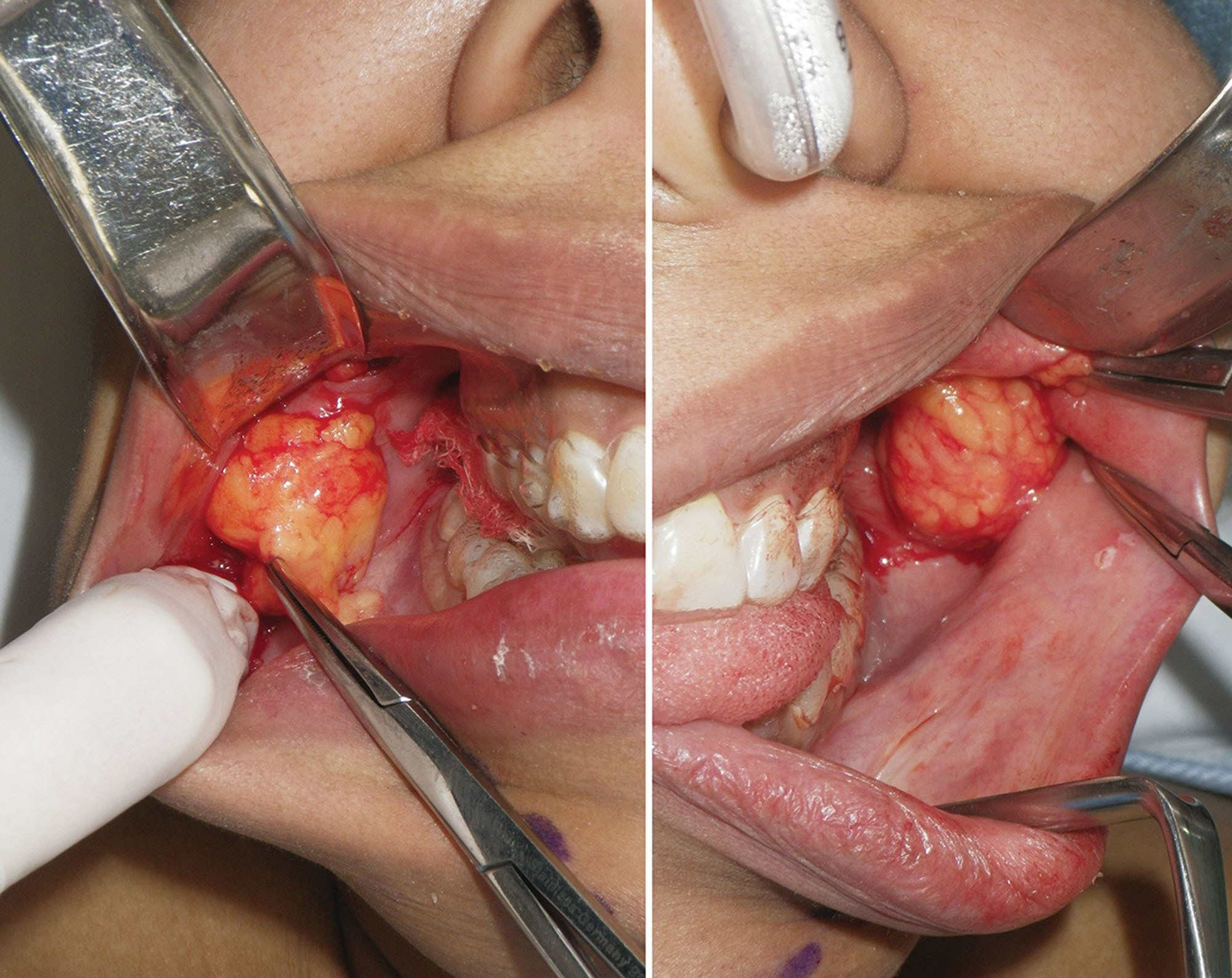
After the incision is made through the mucosa, a long, thin tonsil clamp is used to bluntly puncture through the buccinator muscle. This is a perfect instrument for atraumatic entry through the muscle, and the delicate curved tips are efficient to spread and grasp the fat pad. After the hemostat punctures the buccinator, the tips are spread within the buccal space, and the fat will frequently billow out of the incision ( Figs. 15.12 and 15.13 ). It is very common to secure a small lobe of the BFP, and once it is teased out of the capsule or incised, the other lobes pour out into the incision, much like blepharoplasty fat pads. As stated earlier, the parotid and buccal branches of the facial nerve traverse this area, so gentle manipulation is required ( Fig. 15.14 ).
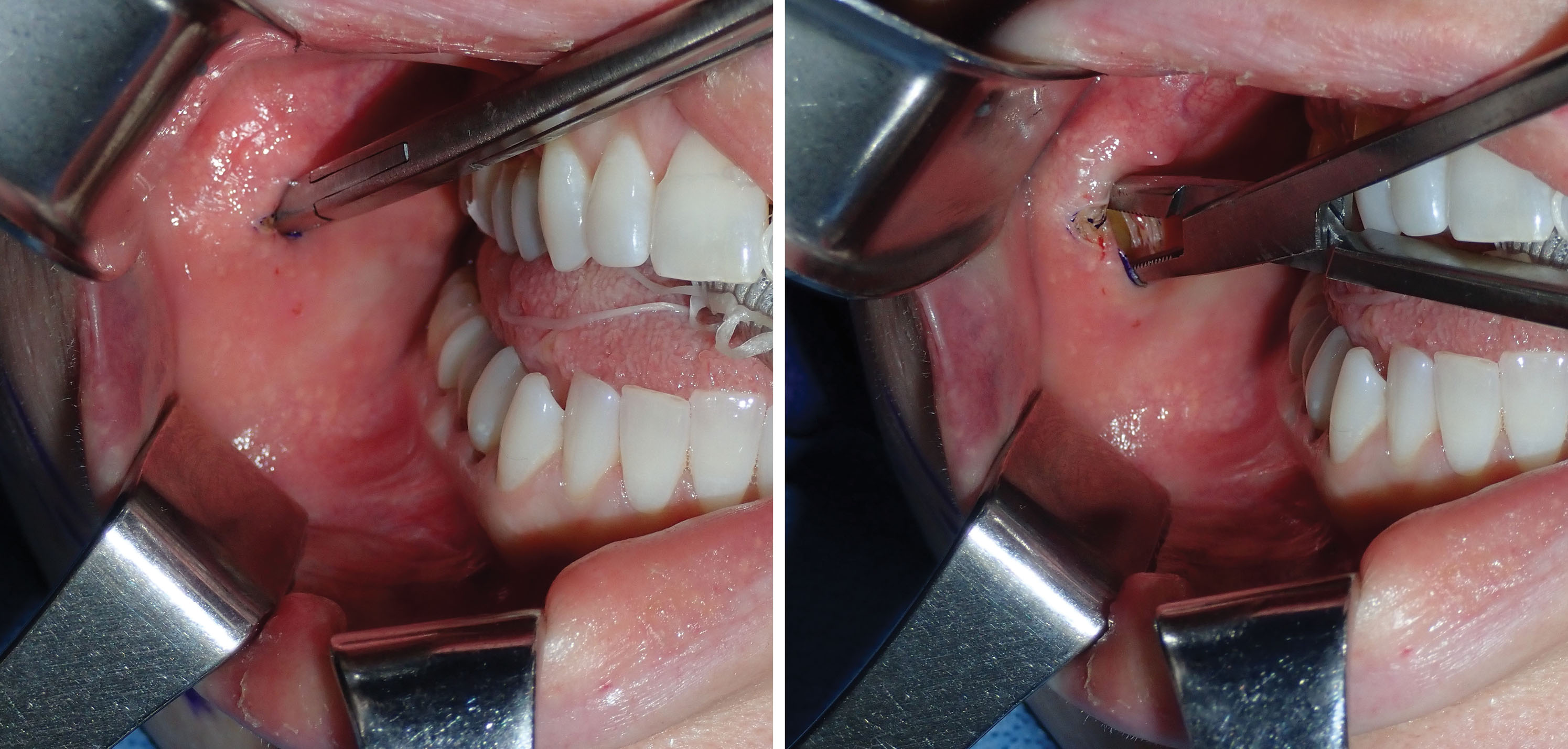


Angling the hemostat slightly superolaterally can be helpful in locating the fat pad. Placing digital pressure on the cheek skin and manipulating the fat pad to the incision is helpful to capture the fat if it does not readily present ( Fig. 15.15 ). Once delivered, the fat pad is then secured with another pair of hemostats under slight traction ( Fig. 15.16 ). Usually this reveals more fat, and the second pair of hemostats is placed at the base and traction applied. This reciprocal procedure is repeated and allows the majority of the fat to be teased out of the capsule into the incision.


If the fat does not present itself, the hemostat is repositioned superolaterally, and spreading is continued. If the fat pad mass is still not located, a 3- to 4-mm suction tip can be inserted while the assistant pinches the suction hose. The suction is then directed superolaterally, and the hose is unpinched to activate the suction. This maneuver will frequently engage the fat pad and pull it from the incision ( Fig. 15.17 ). Once secured, the buccal pad may present in various configurations in given patients ( Fig. 15.18 ).
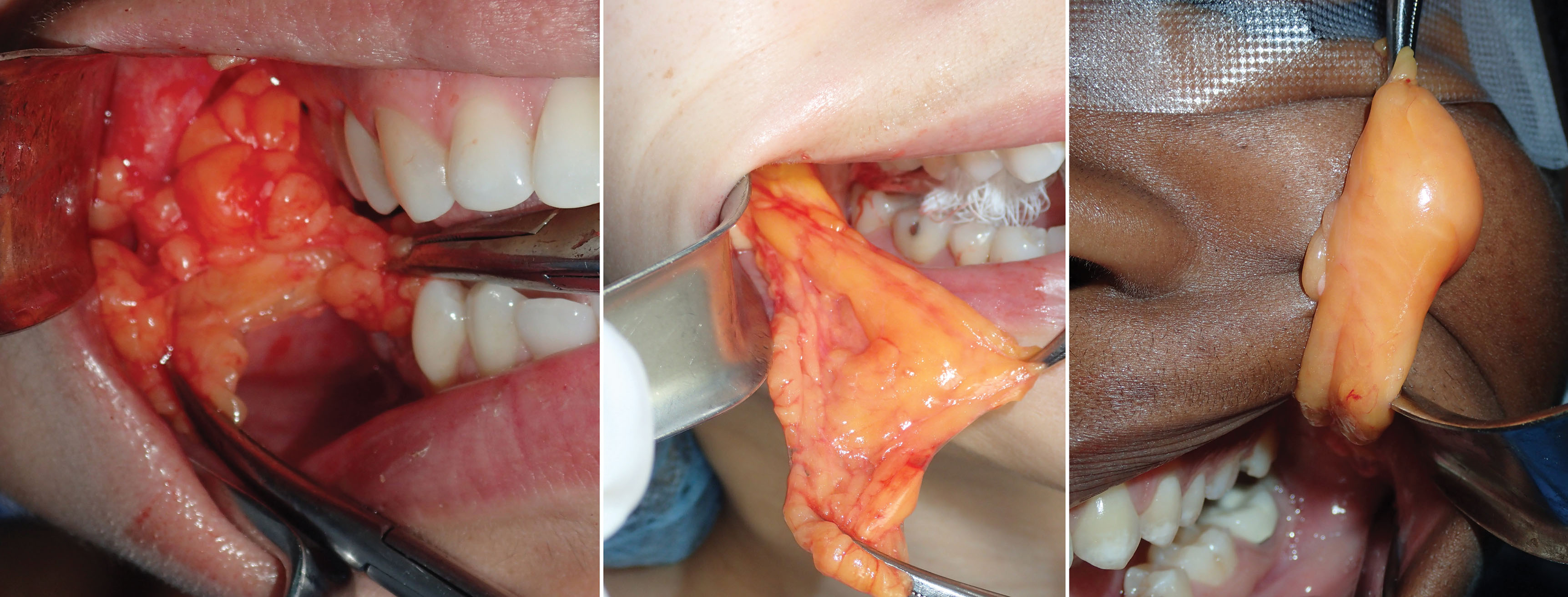
If the surgeon cannot locate the fat pad through the parotid duct incision, a pterygoid approach is performed in which a more superior incision is made in the sulcus lateral to the second and third molars, and the hemostats are introduced and guided inferolaterally ( Fig. 15.19 ). Spreading the tips of the hemostats and employing the suction as described may be necessary in the pterygoid approach as well. Fig. 15.20 shows the BFP in place as viewed through an upper-right cheek implant incision.

Once the available fat is delivered into the oral cavity, it is reduced with bipolar forceps or an electrosurgery tip at the base for coagulation ( Fig. 15.21 ). It is important to use a coagulative modality as vessels penetrate the fat pad in the same manner as blepharoplasty.
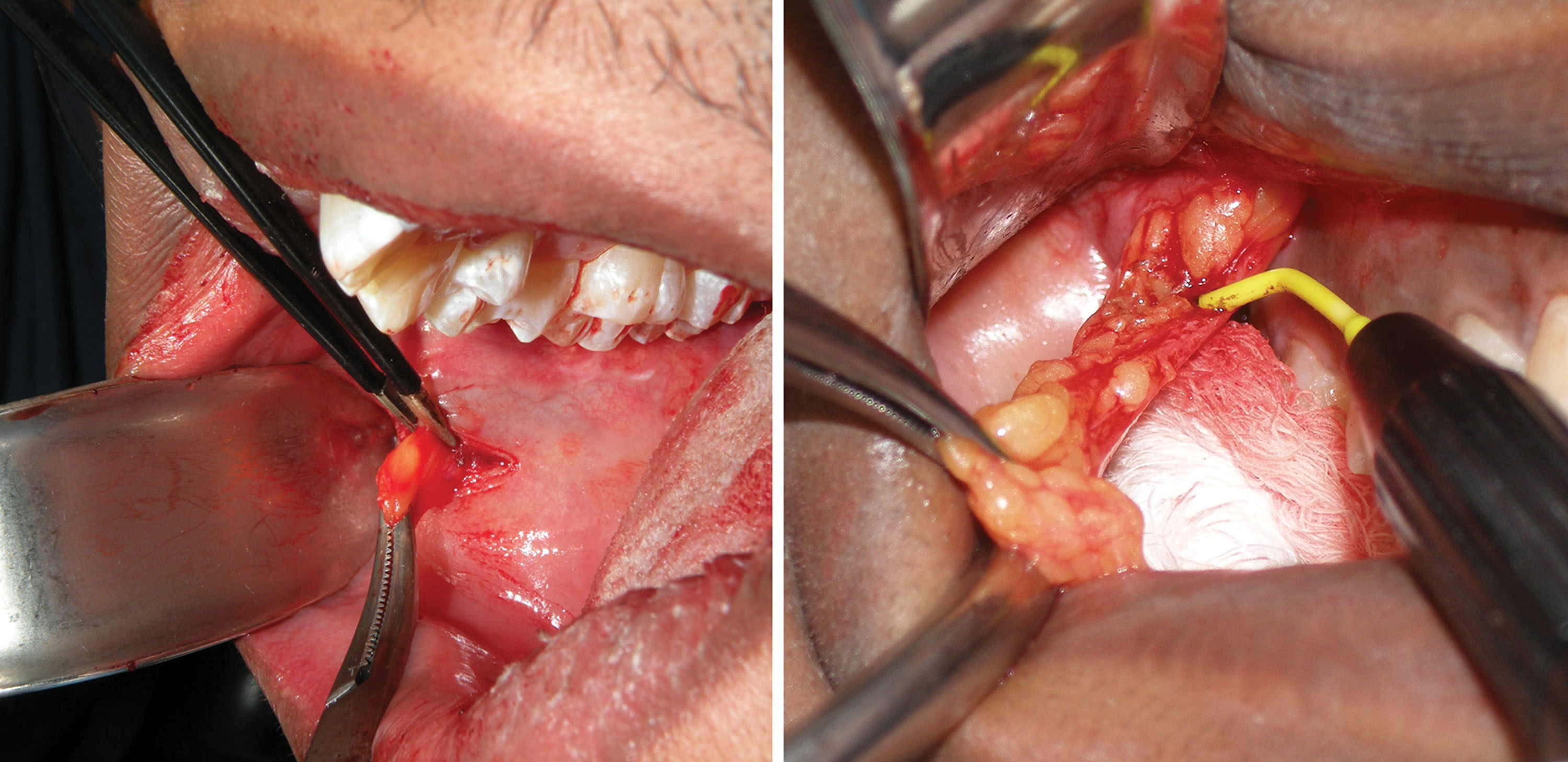
The end point of buccal fat reduction is gauged in a similar manner to blepharoplasty. The excess fat that readily presents itself with minor traction and superficial exploration is removed. Additional contributions to the end point are the lack of additional fat delivered into the mouth and visible depressions at the site of the BFP ( Fig. 15.22 ). Performing BFR is very similar to blepharoplasty in that overresection can produce a skeletonized appearance. Facial fat is a friend and not an enemy, and reduction should be judicious. Generally removing all of the easily available fat that herniates into the oral cavity with suction or moderate traction is sufficient for a noticeable clinical result.
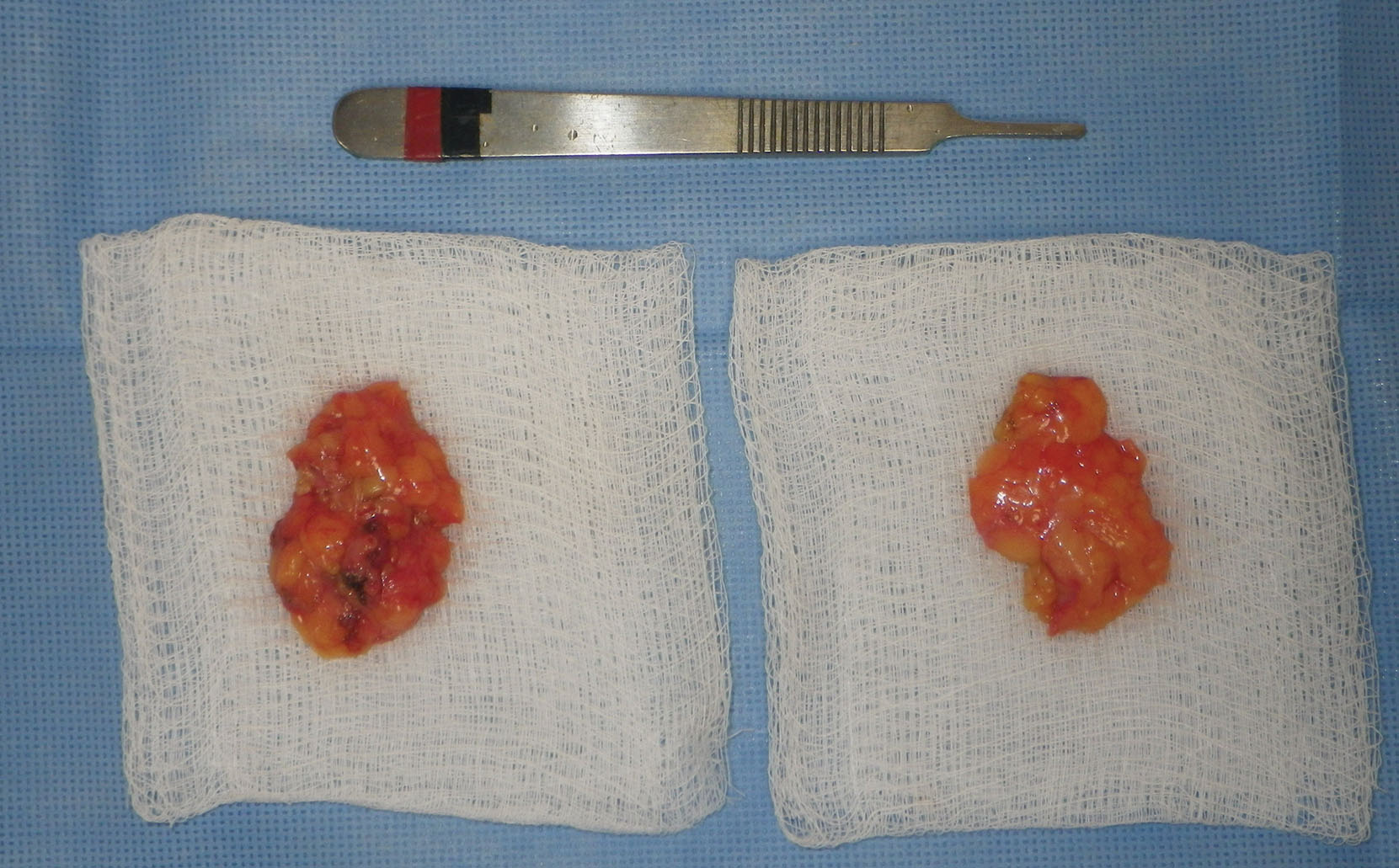
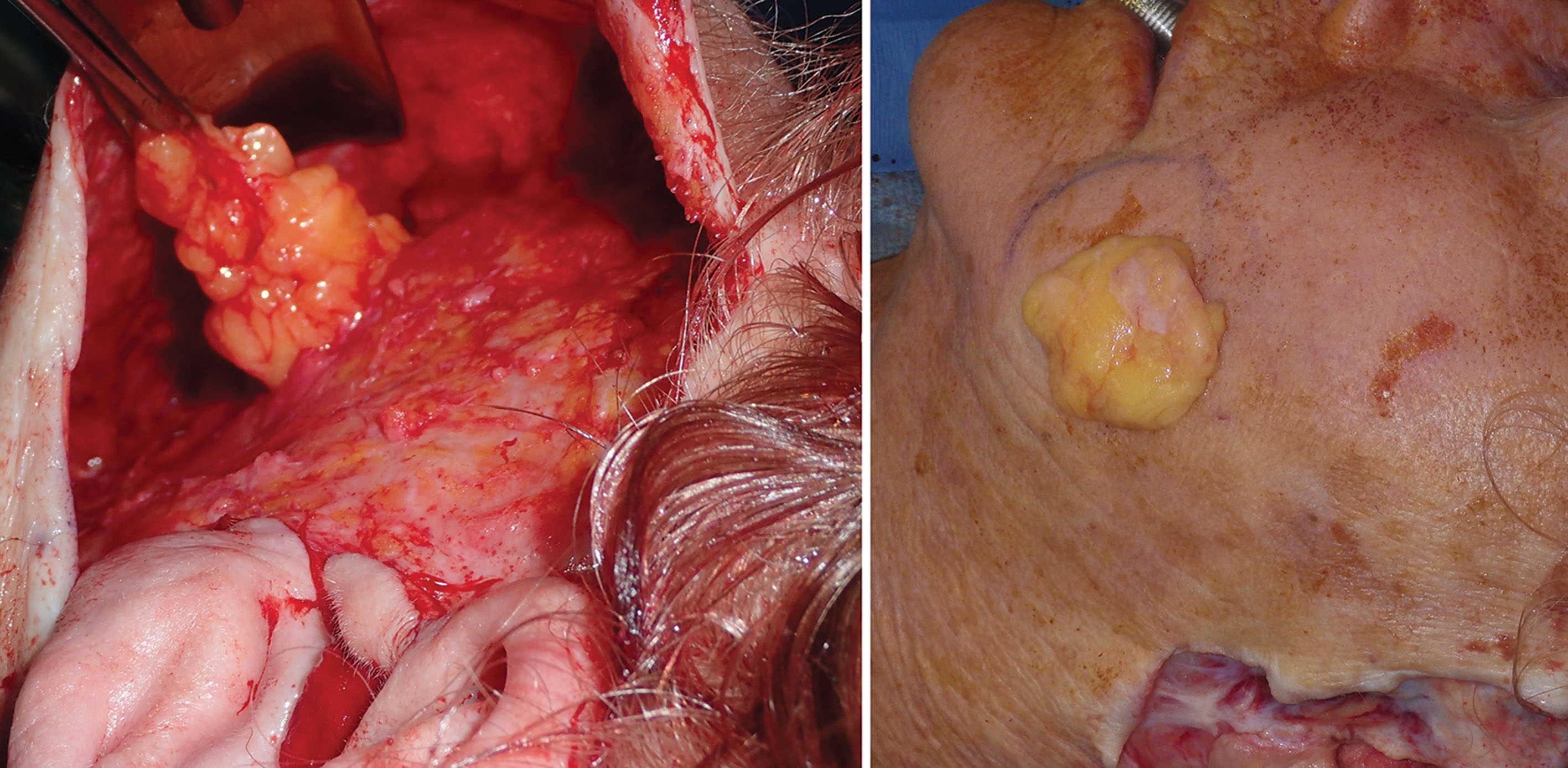
Before transection, a photo is taken of the BFPs when delivered into the mouth. A photo is also taken of the excised specimen ( Figs. 15.23 and 15.24 ). This is done for medical records and also because every single patient is interested in how much fat was removed.
After sufficient fat is removed, the surgical site is checked for hemostasis. The buccinator muscle at the incision site is a frequent source of bleeding and can contribute to a hematoma. If active bleeding is encountered deeper in the wound, cauterization must be carefully addressed as facial nerve branches can be in the proximity as they traverse the masseter muscle. Packing the wound with gauze can also assist in hemostasis. Wound closure is performed with one or two 4-0 gut sutures.
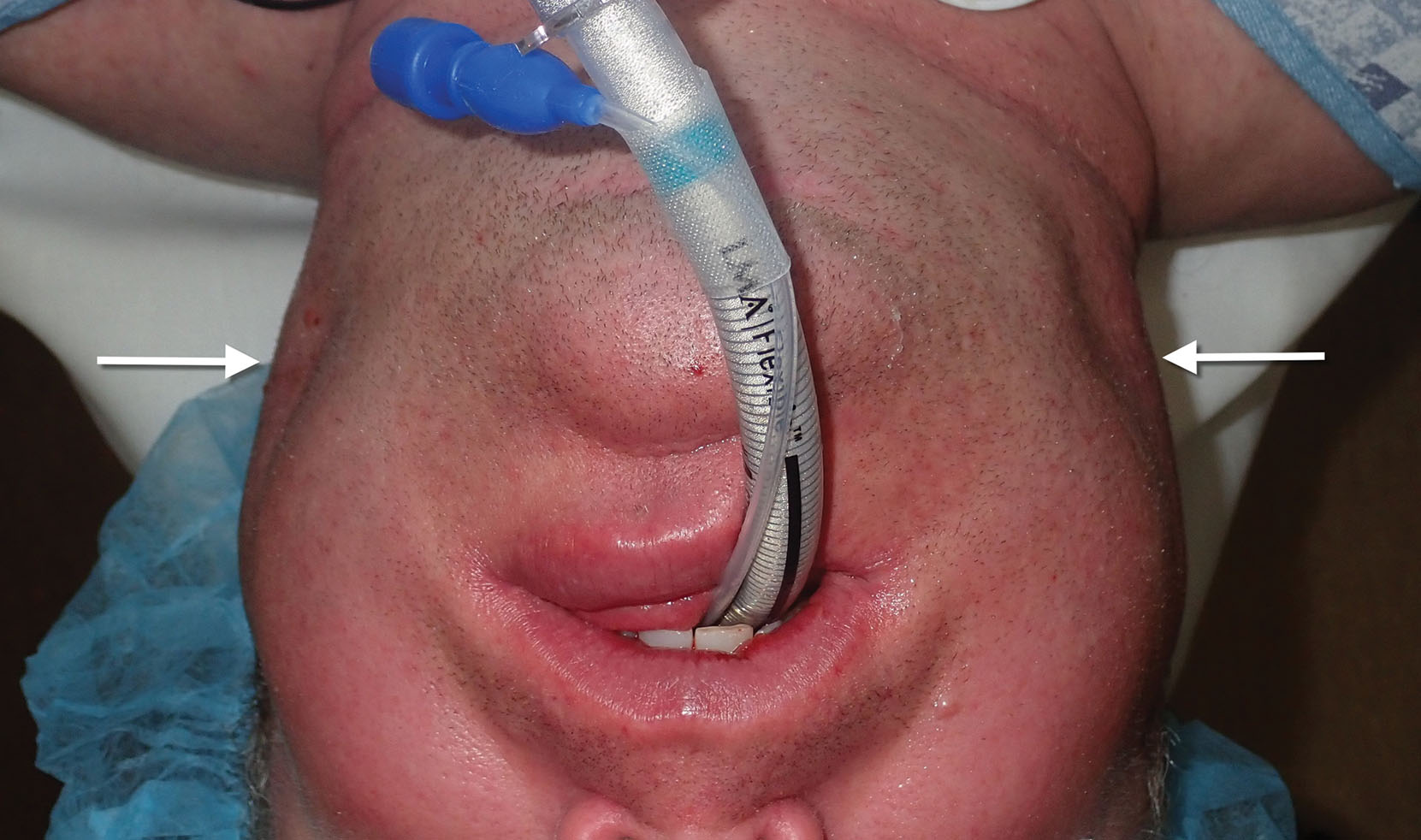
Postsurgically, gauze packs are placed between the cheeks, and a compressive dressing is placed for 24 hours. This dual-layer compression assists in eliminating dead space and may assist in control of bleeding and swelling ( Fig. 15.25 ).

Recovery is generally minor, although some patients may experience significant edema. Patients are told to avoid bending, lifting, or any activity that produces the Valsalva maneuver and to expect an approximately 1-week recovery.
Figs. 15.26–15.34 show before and after cases of BFR. Although plentiful fat can be removed bilaterally, the clinical result is subtle, and it is sometimes difficult to see a big difference in before and after images. Most frequently the patient can appreciate a change regardless of photos and is happy. Patients must be informed preoperatively that the changes with average BFR are small to moderate. Patients with inflated presurgical expectations are not good candidates.






Complications
As stated, judicious dissection and grasping must be performed because related anatomic structures such as the parotid duct and large vessels can traverse the cheek ( Fig. 15.35 ). Minor punctures or lacerations can be treated with a simple suture closure. In the case of severe laceration or transection of the parotid duct, cannulating the parotid duct orifice with an intravenous cannula assists in stabilizing the sutured repair and maintaining patency of the duct. The cannula is sutured to the cheek mucosa and left in place for several days.

The buccal fat reduction procedure traverses some very vascular structures, and brisk bleeding can occur. This is problematic as the buccal branch of the facial nerve and the parotid duct preclude aggressive blind coagulations. In the case of excessive intraoperative bleeding, hemostatic gauze can be packed into the surgery site and left for 10 minutes ( Fig. 15.36 ). This usually will assist in controlling bleeding and allowing exploration. Failure to control intraoperative bleeding can lead to hematoma formation ( Fig. 15.37 ).


I have witnessed temporary buccal branch paresis from this procedure. Infection is a possibility, but I have not witnessed any.
Cervicofacial Liposuction
Joe Niamtu, III
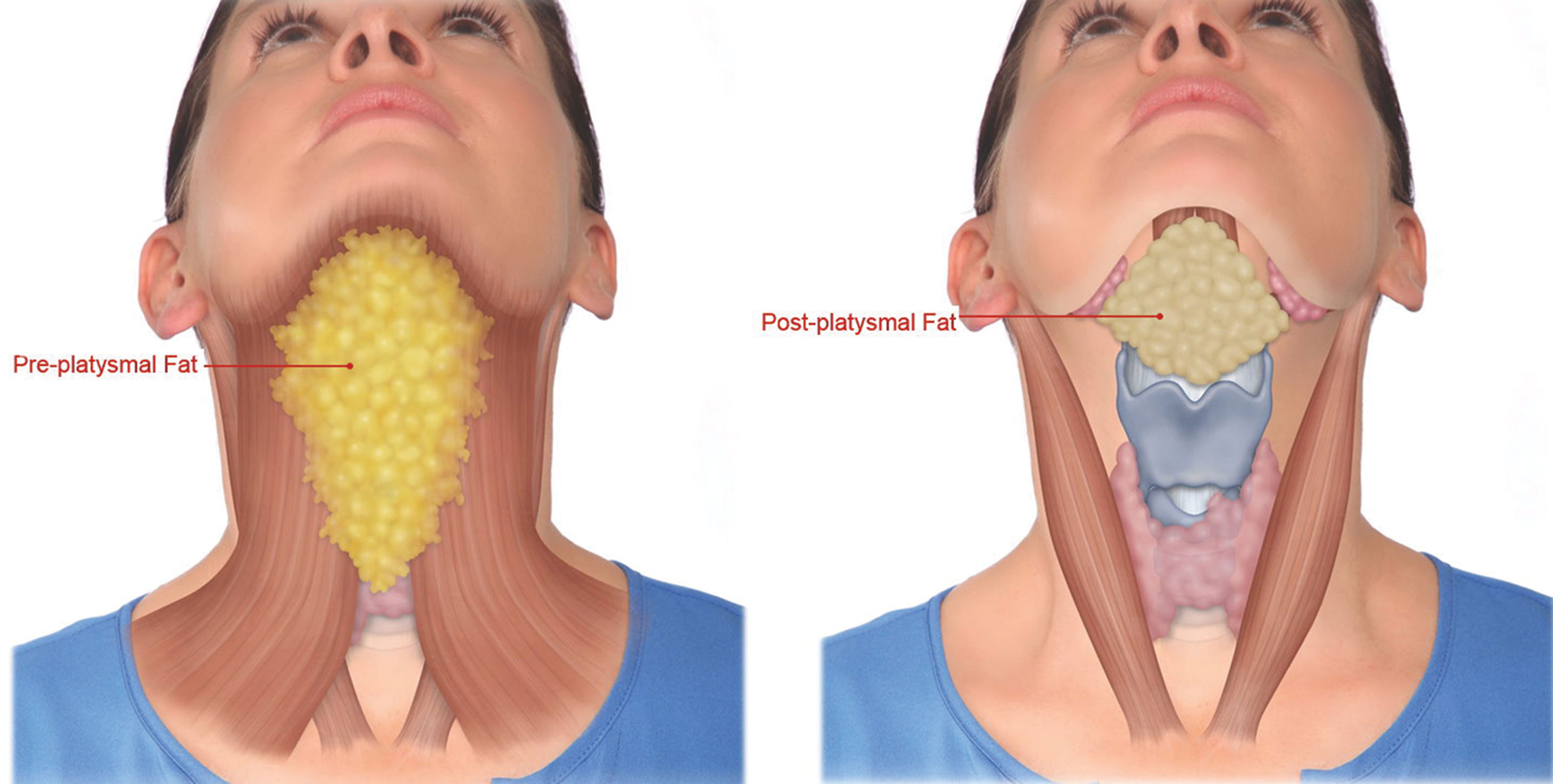
The subcutaneous planes in the face and neck have a distinct layer of fat in young and fit individuals. Deeper fat deposits such as the BFPs and the subplatysmal submental fat also contribute to youthful facial volume ( Fig. 15.38 ). With aging and weight gain, patients can accrue large amounts of subcutaneous and deep fat ( Fig. 15.39 ).

Liposuction is an effective procedure for fat reduction and one of the most commonly requested cosmetic procedures. Although it can be very effective in the face and neck, it is not a treatment for obesity. Liposuction is more indicated for sculpting of specific areas such as the neck, jowls, and jawline. It is important that patients understand the limitations of isolated cervicofacial liposuction. All of my consents detail not only the expected results, but also “what your procedure will not do.” Cervicofacial liposuction is most effective for small, isolated fat deposits that are resistant to weight loss.
Anatomy of Liposuction
Lobules of fat are separated by fibrous septae that contain neurovascular structures and lymphatics. The individual fat cells contain triglyceride, and in weight gain the fat cell increases in size. Weight loss from diet and exercise can decrease the quality of the fat cells (decrease in intracellular fat) but not the quantity (number of fat cells). Liposuction removes the actual fat cells, and these cells will no longer contribute to fat increase; therefore the results are permanent in this context. When the fat cells are removed with the cannula, the septae remain intact, giving the region a “Swiss cheese” appearance ( Fig. 15.40 ).
Skin tightening can occur with tumescent liposuction by unknown means, although it is believed to relate to posttraumatic fibrosis and collagen ratcheting and or shrinkage. Younger patients have a better skin-tightening response to liposuction than older patients. It is important for patients to understand that removing fat can lead to skin excess, especially in older patients. Many patients present with submental fat and cervical skin excess and request liposuction. By removing the fat in this region, a volume reduction occurs that can create more skin excess. Although submental liposuction may be very effective in a younger patient with increased fat and minimal skin excess, it could be problematic in an older patient with excess skin. In these cases, facelift surgery is necessary to address the skin.
Tumescent Anesthesia
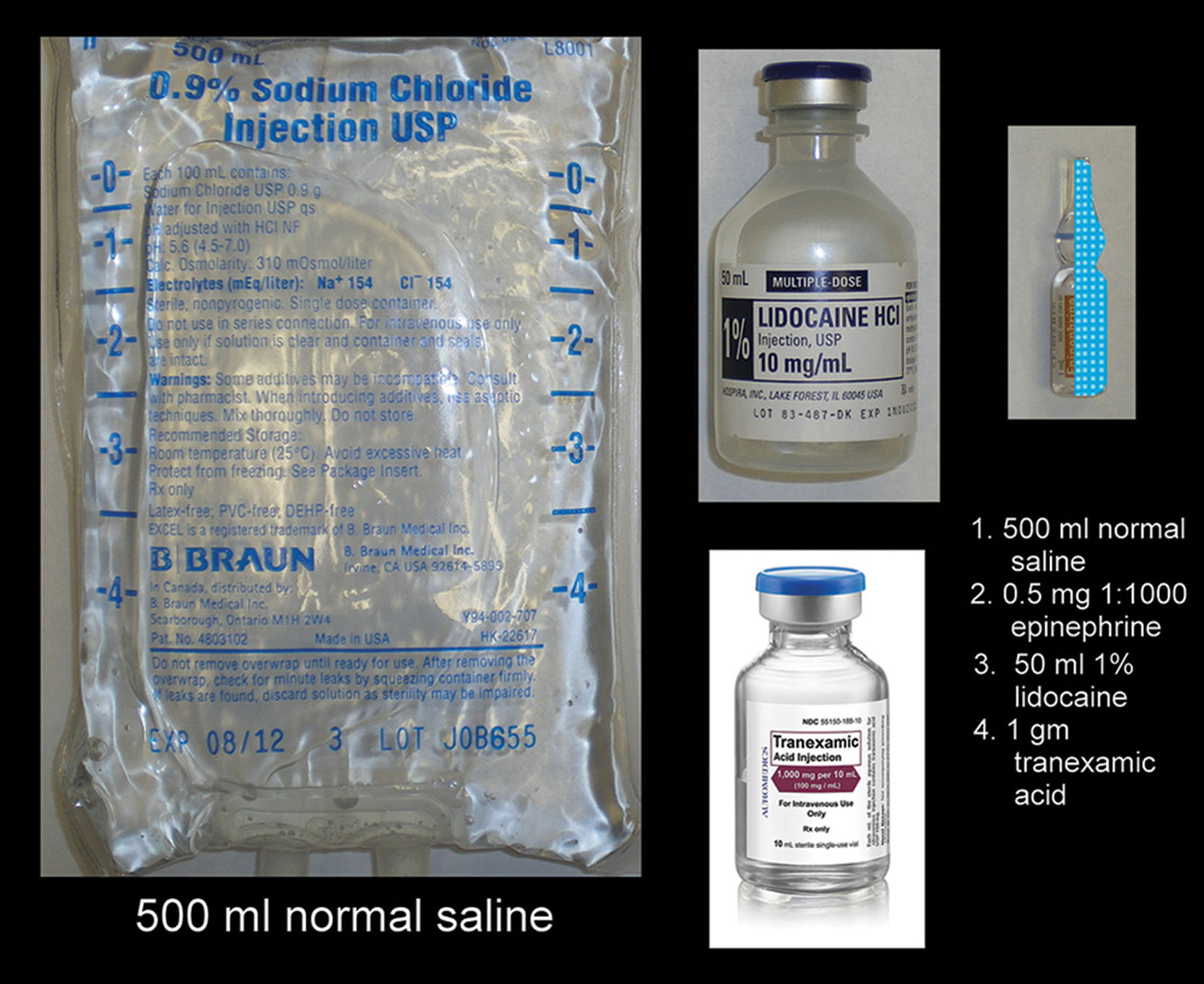
Tumescent liposuction was a true paradigm shift in cosmetic surgery and enabled safe and predictable fat sculpting with local anesthesia. The basic functions of tumescent anesthesia are hydrodissection of tissue planes allowing for more accurate treatment, hemostasis from the epinephrine and tranexamic acid, and local anesthesia from the lidocaine. Body liposuction patients may receive up to 6 L of tumescent solution, and there are much more significant fluid balance considerations than in the face and neck, where much smaller volumes are used. Typical tumescent anessolution consists of 1 L of saline or lactated Ringer’s solution with 1 g of lidocaine and 1 mg of epinephrine (1:1000 concentration). Over the past several years I have begun adding 1 g of tranexamic acid to the mixture as well. Because an entire liter of solution is usually not necessary for facial procedures, the components can be halved for a 500-mL volume ( Fig. 15.41 ).
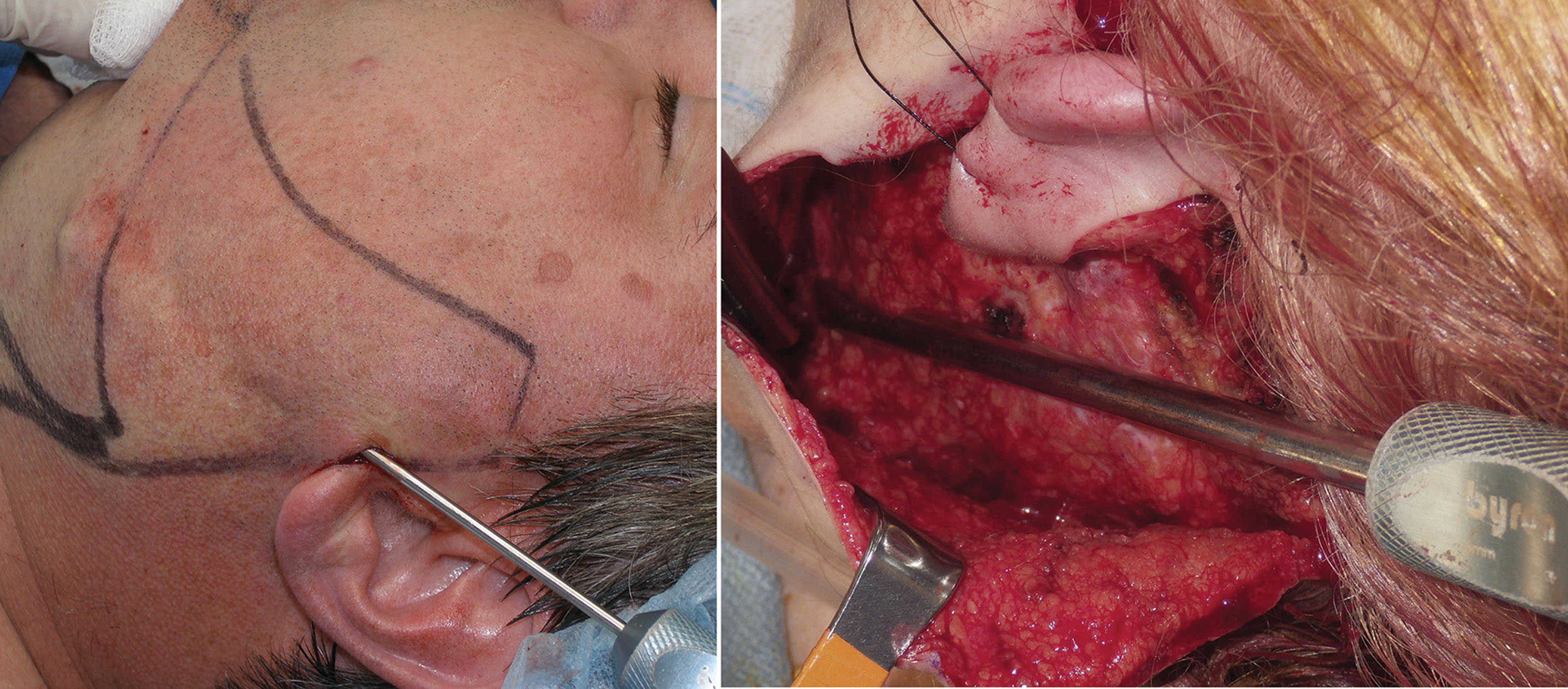
The areas of intended liposuction are marked with the patient in the upright position before surgery or administration of tumescent anesthesia. Commonly treated areas are the submental regions, jowls, jawline, and lateral neck.
After the patient is prepped, tumescent anesthesia is infiltrated. I prefer a Klein pump with a 22-gauge spinal needle ( Fig. 15.42 ). Alternately, a dedicated blunt infiltration cannula may be used and is a better choice for novice surgeons as it is less traumatic. Hypodermic syringes can be used in place of a peristaltic pump. The tumescent solution is injected in the subcutaneous plane.
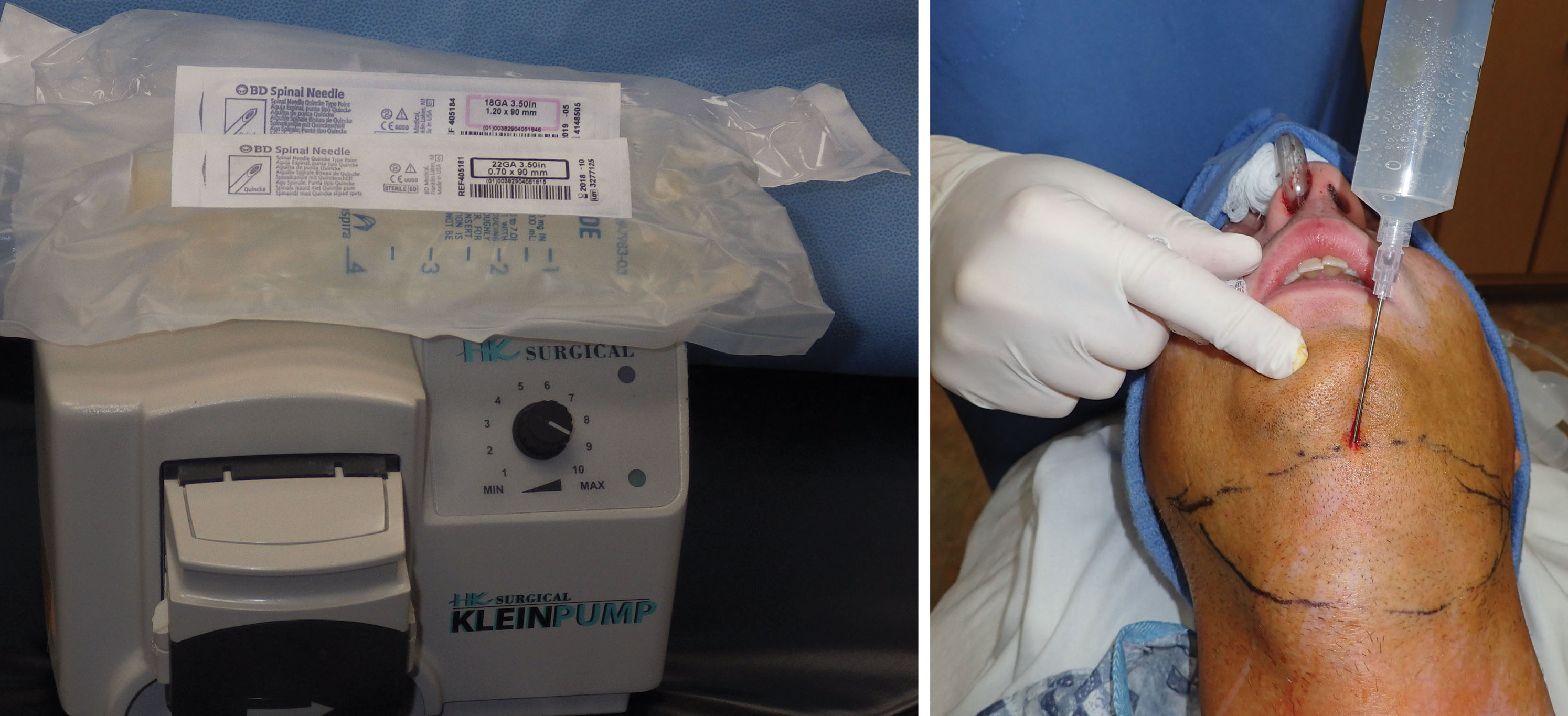
Approximately 100 mL of tumescent solution is infiltrated into the submental region, about 50 mL on each submandibular region and about 30 mL over each jowl ( Fig. 15.43 ). The tumescent solution is injected, and the patient is prepped and draped, which gives the tumescent time to percolate through the tissue planes in a process called detumescence . When the surrounding skin is blanched, the patient is ready for the procedure ( Fig. 15.44 ).


Liposuction Instrumentation
As opposed to body liposuction, the relatively small volumes of fat removed during cervicofacial liposuction (15–30 mL) only require basic instrumentation. Although a dedicated liposuction pump is generally used for body liposuction, standard wall suction will suffice for face and neck liposuction as the fat accumulations are much less ( Fig. 15.45 ).

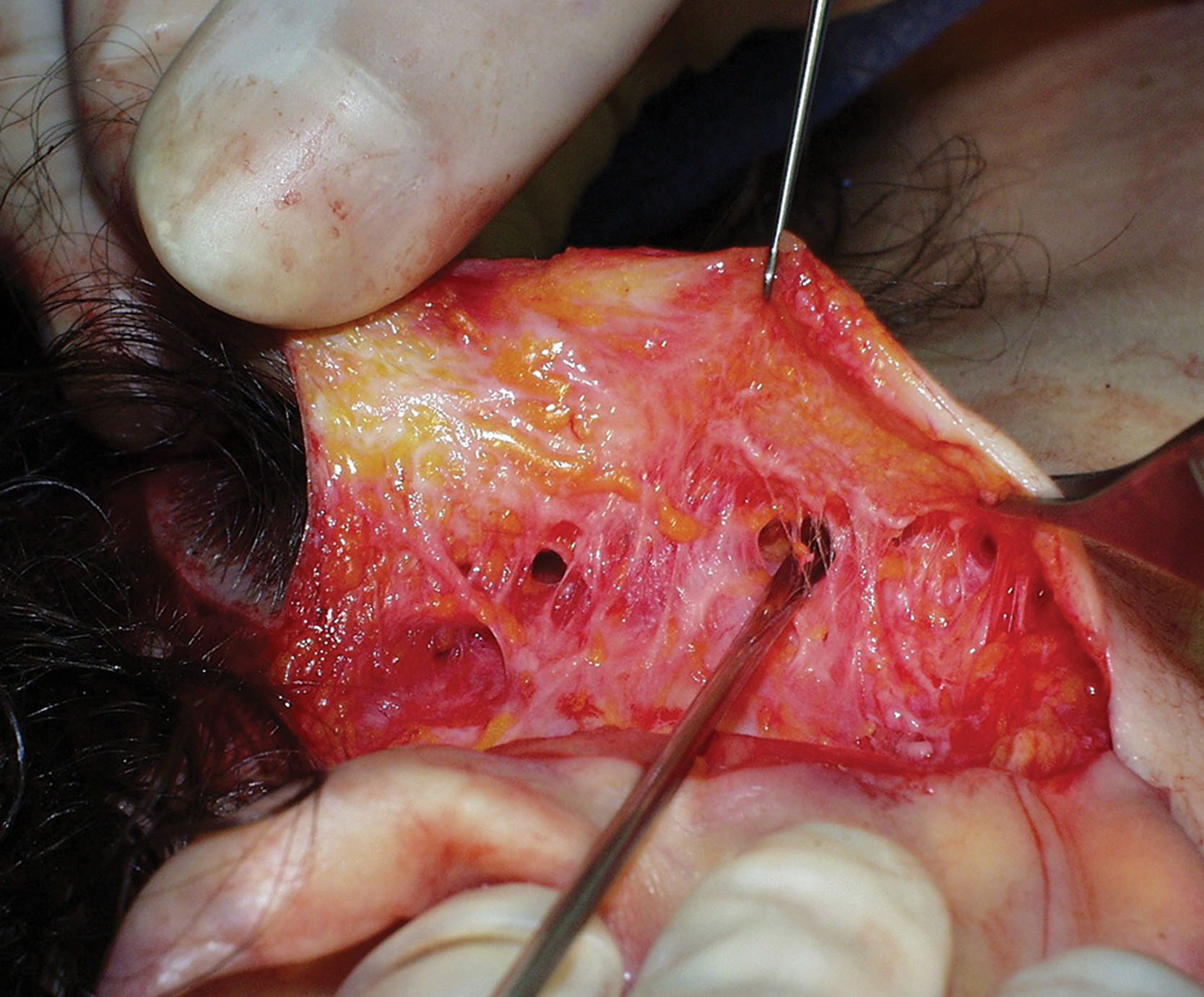
Liposuction cannulas (cannulae) are available in a vast array of sizes, shapes, and configurations. The selection is more varied for large-volume body liposuction, but the instrumentation is simpler for the face and neck ( Fig. 15.46 ). If liposuction is performed in a “closed” manner (i.e., from a puncture), then the entire region is under negative pressure and more efficient. This means that small cannulas of 1–2 mm can be used to sculpt isolated regions of fat, and 2–6 mm cannulas can be used for larger collections. When “open” liposuction is performed, it is generally through a larger incision or flap under direct vision. This means that the area to be treated is not under negative pressure, and fat removal is directly visualized ( Fig. 15.47 ). Larger cannulas can be used in these situations if large fat deposits exist. I frequently use a 6-mm cannula for open submental liposuction with generous fat deposition.

The basis of the liposuction procedure is to place the correct cannula in the correct tissue plane to reduce the correct fat deposit ( Fig. 15.48 ). This basically means that most facial liposuction is performed in the subcutaneous plane, and hydrodissection from the tumescent injection helps define this plane. Small deposits warrant smaller cannulas and vice versa. It is always important to keep the orifice of the liposuction cannula facing away from the dermal surface. Failure to do so can create contour irregularities and grooves from dermal damage. It is also important for the operator to keep in mind relevant anatomy as facial nerve branches and vessels can be injured with liposuction.

The suction hose is pinched (or aspirator turned off) during entry into the puncture site as not to damage the skin. Once the cannula is inserted into the puncture site in the subcutaneous plane, the suction is activated, and the cannula is kept in continual motion. A rapid, reciprocal, to-and-from motion is performed while observing how much fat is exiting the suction tubing and the clinical improvement of the treated site. This is best thought of as a sweeping motion similar to sweeping a carpet with an electric vacuum. The operator should cover a single area with multiple strokes, while trying not to repetitively overlap the same area. Several strokes over the same area are acceptable, but the goal remains a homogenous sculpting treatment over the entire region. With small fat deposition, a single series of strokes may be all that is required, whereas large depositions may require several “passes” of strokes. Marking the patient to indicate the larger areas of fat deposition is efficient as more fat removal will be performed in these areas.
Some surgeons advocate right-angle intersections of the cannula to create a cross-hatch pattern for liposuction. This may allow better removal and contour but is probably more relevant for large-volume body liposuction than for the face. Liposuction is best thought of and referred to as liposculpture because it is important to gently sculpt and reshape the treated regions as opposed to simply emptying them.
It is important (especially for novice surgeons) to be able to judge the end point of treatment. Part of this judgment is a learned tactile experience. Pinching the skin and fat between the finger and thumb before, during, and after the cannula strokes can help judge the amount of fat present and remaining ( Fig. 15.49 ). This also allows the surgeon to ensure that the skin thickness is homogenous over the entire treatment region. It also helps guide the fat to the cannula tip and allows the surgeon to feel the fat going up through the cannula. Careful observation of the suction tubing is also important. If generous yellow fat is coming through the tubing, the target and removal is effective. When the fat stops coming out or when blood tinged fat is seen (or blood without fat) then the end point is present or near.











