Abstract
Aesthetic female genital surgery has been on the rise for several years. The popularity of Brazilian waxing and visibility of the vulva on the Internet contribute to the popularity of labia minora reduction or labiaplasty. Patients of all ages complain of labia minora excess causing embarrassment and physical discomfort. Safe and effective surgical procedures exist to reduce the bulk and protrusion of the labia minora and have been found to improve these patients’ quality of life.
The education and evaluation of women presenting with aesthetic genital concerns require a unique skill set that may not be familiar to plastic surgeons. These women are usually embarrassed and somewhat ashamed of their genital appearance and hence need gentle encouragement to express their specific concerns. It is helpful to have patients fill out a questionnaire to help elicit their aesthetic and functional concerns.
The consultation with the patient should be in the presence of a female physician extender. It is helpful to educate patients regarding the anatomy of the vulva with digital or print media. Patients need to understand the great variability of the labia minora appearance and be assured that they are normal. It is helpful to show before and after photographs to the patients in order to determine their aesthetic goals. Some patients prefer a more natural appearance with the preservation of more labia minora where others prefer a very trim result.
Below are the step-by-step instructions for performing the wedge labiaplasty and radiofrequency treatment of the labia majora.
88 Extended Wedge Labiaplasty with Bipolar Radiofrequency Labia Majora Reduction (AVIVA)
Key Points
Aesthetic vulvar surgery requires a thorough preoperative analysis of the anatomy as it pertains to meeting the aesthetic goals of the patient.
Labia minora reduction or labiaplasty is the most common aesthetic genital procedure; patient selection and surgical planning provide the pathway to successful and reliable results.
The minimally invasive labia majora radiofrequency (RF) treatment provides a “scarless” option for patients with mild to moderate labia majora skin laxity.
88.1 Preoperative Steps
Female physician extender (physician assistant [PA], medical assistant [MA], nurse) sees the patient first to inquire about labial concerns (appearance, symptoms, and desires), any psychological issues, and a detailed sexual history. Written questionnaires given to the patients prior to the consultation are useful in determining aesthetic and functional vulvar complaints.
Digital anatomic diagrams of the vulva are useful patient educational tools that demonstrate variations in anatomy, surgical techniques (animations), and scar location. The review of before and after photographs with patients at consultation aids in determining the patient’s desired postoperative appearance.
Patient examination (physician extender should be present in room) with the patient in the lithotomy and standing positions. A handheld mirror may be helpful for the patient to point out specific concerns.
Assessment in the lithotomy position should include mons pubis and labia majora skin laxity and volume, clitoral hood redundancy in the sagittal and coronal planes, palpation of the clitoris to determine if any enlargement is present (clitoromegaly), labia minora skin excess, pigmentation, and connection at the posterior fourchette.
Assessment in the standing position should include extent of labia minora visibility beyond the labia majora, width of the intervulvar commissure, projection of the clitoral hood, and the laxity of the labia majora.
Informed consent with particular emphasis on the risks of dyspareunia, asymmetry, and cosmetic dissatisfaction due to existing anatomical limitations.
88.2 Intraoperative Steps
Photograph patient in standing position.
Oral or intravenous (IV) antibiotic.
Topical anesthetic x 20 minutes if under local.
Photograph patient in lithotomy position (pose labia in several positions).
Mark wedge resection anteriorly just distal to junction of clitoral hood with labia minora and posteriorly so as to not cause excessive tension on approximation of wedge markings (Fig. 88.1).
Inject local 1% lidocaine with 1:100,000 epinephrine (30-gauge needle) subcutaneously and submucosally.
Betadine prep and drape.
Wedge resection:
#15 blade or low temperature RF device (needle tip Bovie or Peak Plasma blade on cutting mode).
Resect wedge superficially to maintain vascular pedicle (Fig. 88.2a–d).
Closure:
Buried suture of 4–0 Monocryl in dermis of leading edge of resection. Leave tail long and grasp with snap.
Close the wedge from medial to lateral with interrupted 4–0 or 5–0 buried Monocryl sutures.
Lateral closure:
Excise dog-ear (if present) superolaterally so scar falls near the sulcus of the labia majora.
If double fold is present (Fig. 88.3) consider running dog-ear along the double fold.
Close leading edge with vertical mattress suture of 5–0 Monocryl. Edge eversion is important to prevent a notch.
Final layer closure with running 5–0 Vicryl Rapide.
Inject Marcaine 0.25% with 1:200,000 epinephrine.
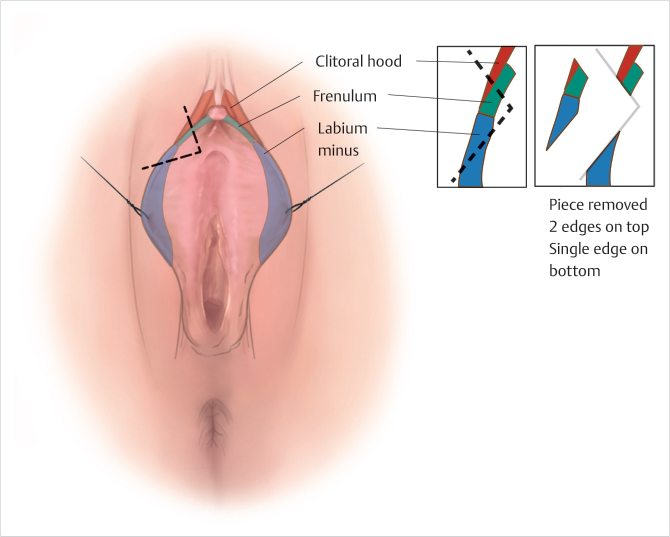
Fig. 88.1 The anatomy of wedge incision placement just posterior to the confluence to prevent closure of a W edge to a V edge. (Reproduced with permission from Hamori CA. Female Cosmetic Genital Surgery. Thieme; 2017.) 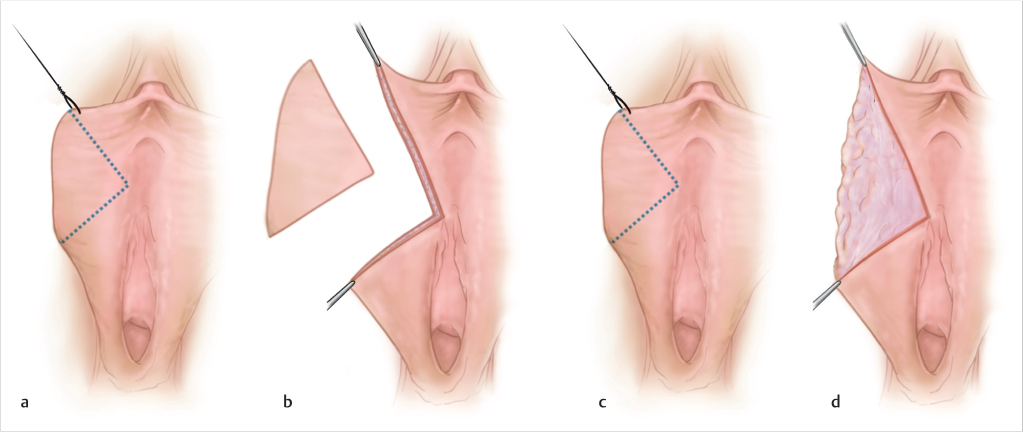
Fig. 88.2 (a–d) A full-thickness wedge resection for thick labia versus demucosalization for thin, atrophic labia. (Reproduced with permission from Hamori CA. Female Cosmetic Genital Surgery. Thieme; 2017.) 
Fig. 88.3 This 50-year-old woman has a double-fold variant. (Reproduced with permission from Hamori CA. Female Cosmetic Genital Surgery. Thieme; 2017.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree