78 Radial Forearm Flap
Abstract
The radial forearm flap is perfused by the reliable and consistent radial arterial system and provides well-vascularized tissue that can include skin, subcutaneous tissue, fascia, tendon, nerve, and bone. Perfusion to the hand is preserved via the ulnar artery and an intact palmar arch. Skin paddles of up to 35cm by 15cm have been described. It can be raised as an antegrade, retrograde, or free flap further increasing its versatility. Recent reports have demonstrated its use as a perforator-based rotational flap, thus preserving the radial artery. Care must be taking during the dissection to preserve the radial artery perforators to the overlying soft tissue and, if harvesting bone, the periosteum of the radius. The resulting donor defect can be closed primarily for smaller flaps, or skin grafted for larger ones.
78.1 Description
First described in 1981, and initially termed the “Chinese flap”, the radial forearm flap (RFF) provides well-vascularized tissue that can include skin, subcutaneous tissue, fascia, tendon, nerve, and bone.
78.2 Key Principles
The RFF is raised on the radial artery or one of its perforators. Distal perfusion to the ipsilateral hand is preserved via the ulnar artery and an intact palmar arch. Sensibility can be preserved by including the medial or lateral antebrachial cutaneous nerves.
78.3 Expectations
The RFF can be raised as a fasciocutaneous, adipofascial, osteocutaneous, or fascial flap. If taken with a skin paddle, dimensions of up to 35cm by 15cm have been described. 1 If pedicled, it has an arc of rotation from the dorsum of the hand to the elbow. If raised as a free flap, its pedicle can be dissected to the point of origin at the brachial artery providing generous length. It can be raised as a sensate flap but provides only protective sensation.
78.4 Indications
The RFF can be used to reconstruct small-to-moderate size defects involving skin, subcutaneous tissue, fascia, bone, and tendon requiring well-vascularized coverage with thin and pliable tissue. It can be used anywhere but is ideally suited for use in oropharynx, facial, and neck reconstruction or for distal upper extremity coverage. The fascia can provide cover for exposed tendons while allowing gliding and is especially useful in treating radioulnar synostosis, recurrent carpal tunnel syndrome, and neurostynalgia of the median nerve. It can be harvested as a proximally based pedicled flap for defects around the elbow, a reversed (distally based) pedicled flap for defects as distal as the proximal phalanges, and as a free flap for remote defects.
78.5 Contraindications
Incomplete palmar arch with inability to reconstruct the radial artery after harvest
Prior damage to the radial artery
History of surgery on the extremity or scarring along course of the radial artery
Smokers or diabetics (relative contraindication)
Osteopenia/osteoporosis (relative contraindication for osteocutaneous flap)
78.6 Special Considerations
A detailed examination of the hand is required to observe for both radial and ulnar pulses, intact superficial and deep palmer arches (assessed via an Allen’s test), and any indications of prior surgery, trauma, or arterial catheterization at the wrist. Suboptimal arterial inflow that cannot be reconstructed with a vein graft will lead to hand ischemia, especially of the thumb, and may limit flap viability. Attention should be paid to the quality and quantity of the hair, if any, if the flap is to be used for mucosal resurfacing. If venous outflow is suboptimal, the cephalic vein can easily be harvested to provide additional drainage for antegrade flaps.
78.7 Special Instructions, Positioning, and Anesthesia
Supine patient positioning with the arm abducted and placed on a hand table. Ideally the non-dominant hand is selected. The entirety of the upper extremity is prepped into the field.
The recipient site, if distant, should be separately prepped to allow for wide exposure of recipient vessels. A portion of a leg should also be prepped providing access to the saphenous vein in case reconstruction of the radial artery is necessary.
A tourniquet is helpful but is not mandatory. If used, the arm should only be partially exsanguinated to allow better visualization of the vessels.
The flap can be raised under region block or general anesthesia.
78.8 Tips, Pearls, and Lessons Learned
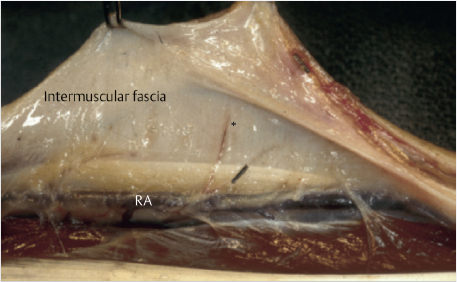
78.8.1 Radial Artery Perforator Location
The radial artery perforators are primarily located within the distal half to third of the forearm (► Fig. 78.1). 2 , 3 In addition, they tend to run in an axial fashion once they reach the fascia. Free flaps, whether perforator-based or incorporating the radial artery, or pedicled flaps with skin paddles must be designed with this consideration in mind. Reverse pedicled flaps based on a very proximal skin paddle for maximal pedicle length are possible if the distal fascia is also incorporated while leaving the overlying skin behind or taking a larger paddle to capture more perforators. Two or more separate islanded skin paddles can be designed if based distally or perforators are identified within each island (► Fig. 78.2).
78.8.2 Composite Flap
A composite flap can be created utilizing multiple tissue types depending on the nature of the defect being reconstructed. The RFF is capable of supplying a small segment of rigid bone by raising the lateral cortex of the distal radius. The palmaris longus tendon can be included if tendon is required.
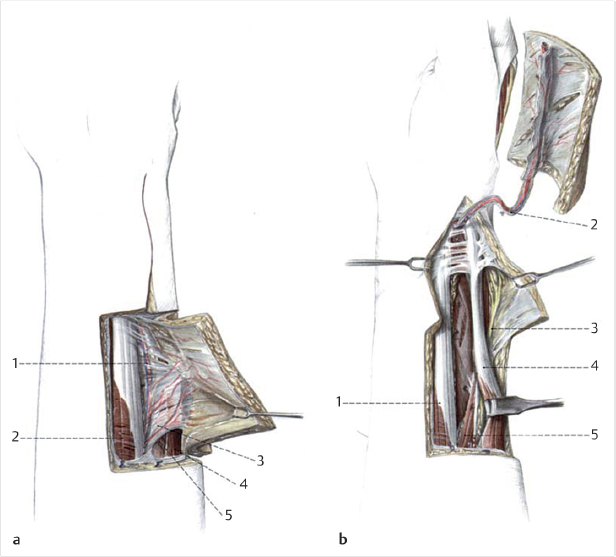
78.8.3 Tunneling a Pedicled Flap Under a Skin Bridge
Passing a flap through a tunnel under a skin bridge can be challenging. Squeezing the flap through a tight space can shear the perforators between the radial artery and skin paddle and cause partial or full loss of the paddle. To avoid this problem, the flap can be wrapped with a sterile plastic drape with the end of the flap sutured to the drape while the pedicle is left free. This will protect the skin paddle as it is transposed while maintaining its orientation so the pedicle does not get twisted (► Fig. 78.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree