70 Split Thickness Skin Graft
Abstract
Split-thickness skin grafts (STSGs) are indicated for wounds that cannot close primarily and are at risk of secondary skin contracture. A healthy wound bed is required for STSG. Healing occurs by plasmatic imbibition, which provides the necessary nutrients for capillary ingrowth (inosculation) and fibroblastic maturation. Vacuum-assisted closure (VAC) device dressings can aid in take of the skin graft. The technique for successful STSG harvest and application is described, and so are techniques for salvage and dealing with complications.
70.1 Introduction
70.1.1 Indications
Split-thickness skin grafts (STSGs) are indicated when primary wound closure is not an option and closure by secondary intention is a poor choice. In order for a STSG to heal, a suitable wound bed is required. The wound should be debrided of necrotic tissue and bacterial load should be minimized in order to prevent graft loss from infection. 1 In addition, the graft bed must be well-vascularized to allow for plasmatic imbibition, the diffusion process by which skin grafts receive their nutrition. The wound bed should not contain any areas of denuded bone, or exposed tendon or joint, as these tissues will not support inosculation, which is the process whereby the skin graft undergoes capillary ingrowth from the underlying tissue. A simple rule of thumb is to avoid skin grafting on top of any white structures: bone, tendon, joint, ligament, or nerve. Healthy fat, muscle, paratenon, or periosteum is suitable for successful incorporation of skin graft.
Skin grafting can be performed using either STSGs or fullthickness skin grafts. A STSG harvests the epithelium and a varying portion of the dermal layer. A full-thickness skin graft harvests the epithelium and the entire dermal layer. STSGs undergo secondary contraction and, as such, are not suitable for wounds over joints. In addition, STSGs have poor elasticity and durability and this should be considered when grafting wounds over areas that are subject to frequent shear. An advantage of STSGs is that they adhere more readily to wound beds and therefore are more likely to take in less ideal wound beds. Fullthickness skin grafts are preferred in wounds around joints or in the palm of the hand due to a lower degree of secondary contracture. However, full-thickness skin grafts experience greater levels of a hypermetabolic state after harvest due to the increased thickness of dermal tissue requiring nutritional support. Therefore, full thickness skin grafts are more likely to fail than STSGs in difficult wounds.
70.1.2 Alternatives
Skin graft substitutes offer an alternative to skin grafting. There are several classes of skin substitutes. Two commonly used skin substitutes are: (1) AlloDerm (LifeCell Corp., Branchburg, NJ), a cadaveric human acellular dermal matrix and (2) Integra Dermal Regeneration Template (Integra LifeSciences Corp., Plainsborough, NJ), a dual layer of bovine collagen dermal matrix with a silicone membrane. Skin graft substitutes provide a scaffold for cellular invasion and capillary growth, which can be beneficial for soft tissue coverage of large wounds 2 , 3 as well as for staging prior to skin grafting in order to enhance the wound bed or thickness of the underlying dermal layer. 4
Another treatment alternative is allowing for secondary wound closure. However, large wounds often are better managed surgically to minimize wound healing time and prevent secondary wound or joint contractures.
70.2 Surgical Technique
70.2.1 Preparation—Planning and Special Equipment
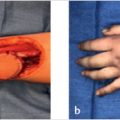
Skin grafting can be performed once the wound has been appropriately debrided to a healthy, vascularized wound bed with minimal bacterial contamination. The vacuum-assisted closure (VAC; KCI, Inc., San Antonio, TX) device is a useful tool to help promote healthy granulation tissue prior to skin grafting. 5 (► Fig. 70.1) In addition, it can also be used as a dressing over the skin graft which can enhance take of the graft by limiting fluid collection under the skin graft and promoting epithelial mitosis and vascular ingrowth through the negative pressure effect. 6

The surgeon should discuss the planned donor site with the patient during informed consent, as well as the possibility of failed take of the skin graft. For STSG, the most preferred site for harvest is the anterior or lateral thigh, due to the ease of harvest and postoperative care. The medial and posterior thigh should be avoided, if possible, to minimize postoperative pain from the donor site resting on the bed or rubbing the contralateral thigh. A dermatome is required as well as a mesher. Meshing of the STSG is not required, but does help prevent fluid from collecting between the graft and the wound bed and allows for a greater area of coverage than the area of donor skin. Various ratios of meshing are available: 1:1.5 is recommended for improved cosmesis and quicker time to reepithelialization. 7 An alternative to meshing is “pie-crusting,” whereby serial small (1–2 mm) holes are perforated in the skin graft to allow for egress of fluid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree