61 Complete Distal Ulna Excision (Darrach)
Abstract
Darrach resection of the distal ulna has been performed for over 150 years to treat arthritis and instability of the distal radioulnar joint (DRUJ). The procedure is performed on low-demand, elderly and sedentary patients, but provides reliable pain relief with good long-term functional results. Radioulnar convergence and symptomatic stump instability with impingement have been described, but with proper technique, these negative effects can be minimized. The Darrach procedure remains a reliable and viable treatment option in the correctly selected patient.
61.1 Description
Many procedures have been described for the treatment of the symptomatic distal radioulnar joint (DRUJ). Complete resection of the distal ulna was first described in the 1850s by Bernard and Huette, 1 and Malgaigne, 2 and several others in the decades to follow, typically indicated for acute trauma. Darrach described the technique in 1912 for management of DRUJ instability, which became the eponym of choice to describe the procedure. Classically, the procedure involves a limited resection of the distal ulna (typically 1.5–3cm)(► Fig. 61.1).
61.2 Indications
Older and lower demand patient’s with DRUJ arthritis.
Rheumatoid arthritis of the DRUJ with symptomatic synovitis.
Radial or ulnar malunions with posttraumatic incongruency oftheDRUJ.
Chronic DRUJ instability.
Ulnar impaction, caput ulna syndrome.
61.3 Contraindications
Young, active, and higher demand patients.
Ulnar translocation of the carpus.
61.4 Pertinent Anatomy
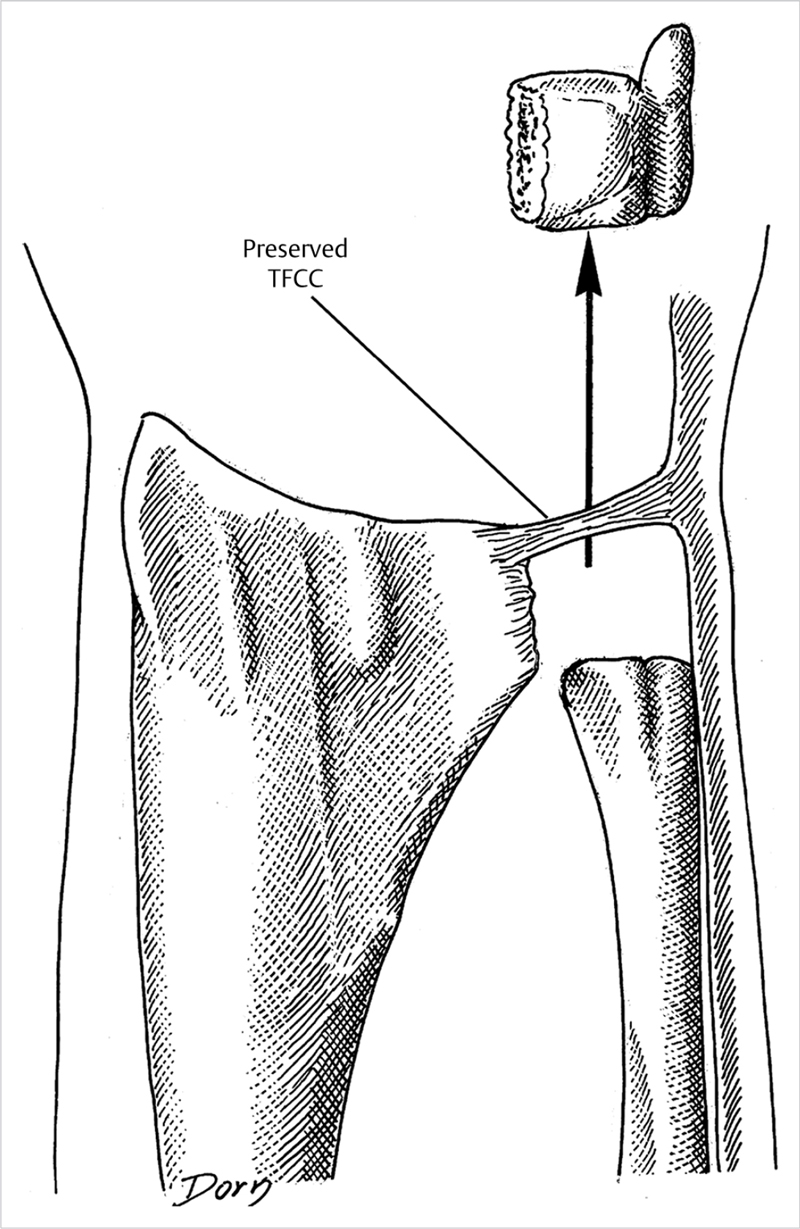
The DRUJ is the distal articulation head of the ulna and the sigmoid notch of the distal radius. This loosely constrained joint allows for forearm rotation, some proximal and distal migration, and palmar and dorsal translation during forearm rotation. The ulnar head not only serves as a fulcrum through which pronation and supination occur but also allows for support of the ulnar carpus. The fovea contains the critical deep attachment layer of triangular fibrocartilage complex (TFCC), extensor carpi ulnaris (ECU) tendon, its subsheath, as well as the dorsal and volar radioulnar ligaments also play critical roles in stabilizing the DRUJ. A considerable percentage (70%) of DRUJ stability is provided by the soft tissue stabilizers with only 30% related to the bony articulation itself. 3 However, presence of the ulnar head serves to tension the soft tissues, and keeps them at a correct length in order to provide that stability. The pronator quadratus also originates from the distal radius and attaches to the distal ulna, serving as a dynamic stabilizer of the distal ulna.
The dorsal sensory branch of the ulnar nerve lies within the subcutaneous tissue, and is potentially at risk during exposure and the surgical procedure. This nerve travels from volar to dorsal, and bifurcates distally typically 1 to 2 cm distal to the ulnar head.
61.5 Clinical History and Physical Examination
Degeneration of the DRUJ can be due to inflammatory arthritis, osteoarthritis, or posttraumatic conditions. Pain with activated grip, activities which require torque, lifting and turning doorknobs, or opening jars, can reproduce pain over the DRUJ. Patients with inflammatory arthritis typically have prominence of the distal ulna and fullness over the DRUJ relating to the synovitic response. Concomitant extensor tendon rupture may occur and should be evaluated preoperatively. ECU subluxation is distinguished from DRUJ arthritis by noting any ECU subluxation with supination and ulnar deviation of the wrist.
Patients present with limited and painful forearm rotation, and with tenderness at the DRUJ. Pain or instability with shuck of the DRUJ can be encountered. The shuck test should be performed in neutral, pronation, and supination, and compared to the contralateral side. The compression squeeze test where the examiner applies manual pressure across the DRUJ can also elicit pain with forearm rotation.
61.6 Imaging
Standard radiographs are the mainstay for diagnosis of arthritis and instability of the DRUJ. A grip view with weight can elucidate convergence. In posttraumatic cases, CT scan may help elucidate incongruity of the DRUJ if X-rays are inconclusive. MRI is typically unnecessary, but can be used to differentiate pathology related to ulnar abutment, and competency of the TFCC. In patients with inflammatory arthritis, evaluation of the radiocarpal joint and ulnar translation of the carpus is paramount, as resection of the distal ulna will further destabilize the wrist.
61.7 Nonoperative Management
Immobilization in a Muenster-type cast or sugartong splint, and activity modifications which limit torque and forearm rotation, can diminish symptoms. Anti-inflammatory medications can be helpful, and intra-articular cortisone injection can provide relief.
61.8 Positioning and Anesthesia
The patient is positioned supine, with the extremity abducted on the hand table under tourniquet control. The procedure may be performed under regional block or general anesthetic.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree