60 Partial Distal Ulna Resection (Wafer, Hemiresection)
Abstract
Partial distal ulnar resection can be used to manage symptoms related to ulnar impaction syndrome and distal radioulnar joint (DRUJ) arthritis. The wafer procedure involves removal of a small portion of the distal ulna in order to offload the ulnocarpal joint in cases of ulnar impaction syndrome. The ulna hemiresection arthroplasty involves removal of the ulnar portion of the DRUJ while maintaining the ulnar styloid and triangular fibrocartilage complex (TFCC), and is performed for management of DRUJ arthritis or incongruity. Neither procedure requires healing of an osteotomy and both maintain the stabilizing structures of the DRUJ and ulnocarpal joints. Each procedure has been shown to decrease pain and improve motion for management of their specific indications.
60.1 Wafer Procedure
60.1.1 Description
The wafer resection of the distal ulna is one means of treating ulnar impaction, or ulnar abutment syndrome. This diagnosis is made clinically when excessive load on the ulnocarpal joint is identified. This most often occurs due to ulnar positive variance, although it has also been described in the ulnar neutral or negative wrist. 1 Patients can present with ulnar-sided wrist pain, decreased motion, and grip weakness. Ulnar positive variance can occur as a normal variant, after a trauma resulting in shortening of the radius such as malunion of a distal radius fracture, or due to a congenital deformity such as Madelung’s deformity or multiple enchondromatoses. This procedure involves resection of the very distal ulna while preserving the triangular fibrocartilage complex (TFCC) foveal attachment. It can be done through an open incision, arthroscopically, or a combined approach.
60.1.2 Key Principles
The wafer procedure can offload the ulnocarpal joint without healing of an osteotomy or implantation of hardware. 2 It has been shown in an ulnar neutral wrist that 18% of force across the wrist joint is centered on the ulnocarpal joint, and when ulnar length increases by 2.5 mm, the force across the ulnocarpal joint increases to 41.9%. 3 Injury to the TFCC is commonly associated with ulnar abutment due to constant loading between the ulna and lunate and triquetrum, and can be addressed during the same surgical procedure. Distal radioulnar joint (DRUJ) pathology, such as arthritis, is not addressed with an ulnar wafer resection.
60.1.3 Expectations
The results of the wafer procedure have shown diminished pain, with return of wrist motion and grip strength 4 in patients with mild ulnar impaction syndrome. When comparing the wafer procedure to ulnar shortening osteotomy, both groups of patients achieved a return to functional wrist motion and pain relief, although hardware removal in patients who undergo ulnar shortening osteotomy is a relatively common occurrence. 5 Return to normal activity after the wafer procedure may take up to 6 months, and there is no guarantee of return to heavy manual labor postoperatively.
60.1.4 Indications
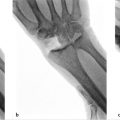
The wafer procedure is considered for patients who present with ulnar-sided wrist pain from ulnar impaction syndrome. Their pain is typically aggravated by forceful grip, forearm pronation, and ulnar deviation. Clinical examination may reveal swelling over the dorsal wrist with tenderness to palpation over the ulnocarpal joint and triquetrum and decreased range of motion. Other causes of ulnar-sided wrist pain must be ruled out, including lunotriquetral (LT) pathology, DRUJ arthritis, DRUJ instability, hook of the hamate injury, extensor carpi ulnaris(ECU)subluxation, andpisotriquetraljointinjuryorarthritis. Imaging studies begin with three view X-ray of the wrist which can reveal ulnar positive variance (► Fig. 60.1) and possible cystic changes of the lunate and/or triquetrum. Ulnar impaction is frequently associated with tears of the TFCC, 6 which can be evaluated by magnetic resonance imaging (MRI), magnetic resonance arthrogram, and/or arthroscopy. For a successful wafer procedure, no more than 4 mm of the distal ulna is resected, or the procedure will result in removal of the majority of the ulnar head articular surface in contact with the sigmoid notch, potentially compromising the DRUJ articular surface.

60.1.5 Contraindications
The wafer procedure is contraindicated in the setting of DRUJ or LT instability or DRUJ arthritis, as the procedure does not address these pathologies. A distal ulnar wafer resection should not be done if more than 4 mm resection is required to neutralize ulnar variance.
60.1.6 Special Considerations
With a three view X-ray of the wrist, ulnar variance is measured on the A/P X-ray with the wrist in neutral rotation. This is achieved with the shoulder abducted at 90 degrees, elbow flexed at 90 degrees, and the forearm and palm flat on the X-ray cassette. A true A/P X-ray can be confirmed by identifying the location of the ECU groove radial to the long axis of the ulnar styloid. The measurement is performed by drawing a line through the volar sclerotic line of the distal radius and perpendicular to its long axis. The distance between this line and the cortical margin of the ulnar dome is then measured as ulnar variance. Ulnar positive variance can be further exacerbated by X-ray performed with the patient in power grip or with the forearm pronated. Ulnar height increases on average 0.4 mm with forearm pronation versus neutral, and this difference may not be clinically significant, 7 but ulnar height can increase an average of 2 mm with a power grip in pronated position. 8 An X-ray of the contralateral wrist is performed for anatomic comparison. Cystic changes and osteophytes of the lunate, triquetrum, and distal ulna usually best seen on PA view are sequelae of long-term ulnar impaction. The DRUJ and LT intervals must also be visualized. Widening or incongruity of either joint or volar intercalated segmental instability (VISI) deformity is consistent with instability and would raise other causes of wrist pain and concern that ulnar wafer resection would be inadequate treatment for the patient.
MRI is useful to diagnose pathology of the TFCC prior to attempting surgical intervention. Increased T2 signal in the ulna and carpal bones is consistent with edema related to increased load and stress across the joint. If TFCC injury is suspected, but not identified on routine MRI, an MR arthrogram can be performed with greater sensitivity in diagnosing injury sustained to the TFCC. 9
60.1.7 Special Instructions, Positioning, and Anesthesia
The wafer procedure can be performed under general anesthesia or upper extremity regional nerve block with monitored anesthesia care. The patient should be positioned on the operating room table with the arm abducted to 90 degrees and forearm pronated for dorsal open approach to the wrist. Upper arm tourniquet is inflated prior to incision for hemostasis and visualization. Mini-C arm fluoroscopy may be used for confirming the location of the incision and extent of the wafer osteotomy. A fine oscillating saw, fine burr or hand-held osteotome can be used for the bony resection.
Wrist arthroscopy instruments with traction tower can also be utilized for diagnostic arthroscopy of the wrist and distal ulnar resection with a burr through the central defect in the TFCC which typically occurs with impaction syndrome. It is controversial whether the arthroscopic wafer procedure should be performed in patients who have an intact TFCC.
60.1.8 Tips, Pearls, and Lessons Learned
Identification of the dorsal sensory branch of the ulnar nerve is critical for the approach to the distal ulna. The nerve should be found in the subcutaneous tissues, just deep to the basilic veins and gently retracted away from the surgical site. Fluoroscopy is helpful to identify the width of bony resection, in order to ensure that the DRUJ is not violated, and verify that sufficient bony resection is performed. It is critical that the foveal attachment of the TFCC and ECU subsheath be kept intact to maintain the stability of the DRUJ and ulnar carpal bones.
60.1.9 Difficulties Encountered
The wafer procedure is performed through an open or arthroscopic approach to the distal ulna. The dorsal branch of the ulnar nerve must be identified and carefully retracted out of the surgical field to prevent laceration or traction injury to the nerve.
In exposing the distal ulna for an open resection, preservation of the TFCC foveal attachment and DRUJ ligaments is critical for maintaining DRUJ stability. Injury to these structures must be repaired, upon recognition, or the wafer procedure will be unsuccessful. The TFCC should also be tensioned appropriately when closing the wrist capsule.
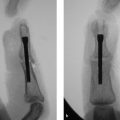
Once all important structures are exposed, the wafer resection can be verified with fluoroscopy. This is essential to ensure that an adequate amount of bone is resected without compromising the DRUJ itself. If the ulnar styloid is fractured during the osteotomy and DRUJ instability occurs, a pin, or other hardware, must be placed for fixation, and the postoperative regimen must be altered to protect healing of this fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree