Abstract
This chapter surveys the anatomy of the breast and covers the matter of breast reduction surgery. The reasons—physical, emotional, reconstructive, aesthetic, etc.—why women of all ages wish to have their breast size reduced vary greatly. Surgical options are varied and the one selected should correspond to the patient’s morphology, nipple placement, previous surgeries, and goals, as well as to the surgeon’s comfort level, training, and experience. The five key steps common to all breast reduction techniques are listed and recommended surgical options and procedures (e.g., liposuction, Wise pattern reduction, vertical reduction, etc.) are discussed in detail. The chapter concludes with suggestions for postoperative care and an enumeration of possible complications.
30 Breast Reduction
30.1 Goals and Objectives
Understand and describe the anatomy of the breast as it relates to breast reduction surgery.
Understand the proper evaluation of a patient considering breast reduction surgery.
Clearly define the indications for breast imaging prior to breast reduction surgery.
Describe the incidence of invasive breast cancer in surgical specimens.
Have an understanding of the basic techniques available to treat a patient with macromastia and which patients are best suited for a particular technique.
Be able to identify and treat the common early and late complications associated with breast reduction surgery.
30.2 Patient Presentation
Women seeking out breast reduction surgery can vary from adolescents to the elderly. Although these patients are from different backgrounds, age groups and body shapes, they consistently present with a similar constellation of symptoms. These symptoms include upper back pain, neck pain, headaches, inframammary intertrigo, difficulty with physical activities, painful bra strap grooving, dissatisfaction with breast appearance, poor sexual well-being, emotional distress, and, though less common, ulnar paresthesias due to pressure on the brachial plexus.
Most patients present for evaluation based on referral from their individual primary care physicians. Though they are physician referred, not all women are candidates for breast reduction surgery due to their current health status, smoking status, or medical history. As such, upon initial presentation, a thorough medical history (including pregnancy, and ability and desire to breastfeed) and examination of pertinent systems is necessary. Specific attention should be given to addressing comorbidities such as diabetes, obesity, and nicotine abuse that can all impair normal wound healing. Any use of antiplatelet and anticoagulant medications should be investigated to determine the exact cause for need of the medication and its implications for the surgery. Personal or family history of breast masses, breast cancer, abnormal mammograms, nipple sensory changes, and current oral contraceptive or hormone replacement therapy should be noted. The patient’s current bra size should be recorded as well as her ideal cup size.
Concerning the adolescent population, emotional distress due to peer pressure, or ridicule from others should be delved into as it can be a driving factor for desiring surgery. This can be a significant issue which can lead to stunted social development at an important time in a young woman’s life and alone can justify undergoing the procedure. 1
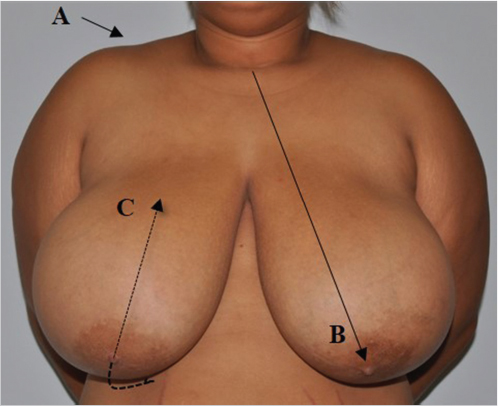
The physical assessment includes height, weight, and calculation of body mass index (BMI; weight in kilogram/height in meter squared). A full breast exam is performed looking specifically for (1) symmetry of the breast and nipple–areola complex, (2) tissue quality, (3) degree of ptosis, (4) presence of masses in the breasts or axilla, (5) position of inframammary fold and changes to the skin in the fold (intertrigo), and (6) presence of shoulder grooving. The manual exam should be done in supine position with the remainder of the exam in the upright position with arms placed at sides. Standard measurements should also be taken measuring the sternal notch to nipple distance and nipple to inframammary fold distance bilaterally. Many other measurements can be helpful depending on surgeon’s preference (Fig. 30‑1).

Understanding anatomy of the breast is key for both evaluation and treatment of macromastia. Especially important is a familiarity with the blood and nerve supply to the nipple–areola complex. Sensation to the complex comes from the lateral and medial cutaneous branches of the intercostal nerves T3, T4, and T5. The lateral branches exit chest wall at the midaxillary line and travel medially along the pectoralis major fascia terminating in the breast skin and nipple–areola complex. Sensation to the upper breast is provided by the lower cervical plexus (Fig. 30‑2). 2 The blood supply is based on musculocutaneous perforators from the internal mammary, anterolateral intercostal and anteromedial intercostal, and fasciocutaneous perforators from the lateral mammary branches of the long thoracic artery (Fig. 30‑2). All of these vessels interdigitate and are present in all four quadrants of the nipple–areola complex forming a dense subdermal plexus. This is important as it allows many different pedicles to be created while still allowing the nipple–areola complex to thrive. Factors such as radiation, smoking, and previous surgery can alter the normal blood flow of the breast and result in necrosis if they are not taken into consideration. Coopers suspensory ligaments are the connective tissue support of the breast and course through the parenchyma to attach to the overlying dermis. These attachments can become lax due to pregnancy, significant weight gain, smoking, and aging, which results in increased breast mobility and ptosis. 3
30.3 Preparation for Surgery
Photographic documentation of the patient’s preoperative appearance is important to obtain during the preoperative consultation. The photos serve as a permanent part of the medical record for patient reference when needed, and also are required for any cases submitted through insurance. The photos should frame the patient from the neck down to just below the lowest level of the breast and from just outside each arm. All jewelry should be removed and hair should be swept back or put up. Three views are sufficient including a frontal view and two lateral views. A three-quarter photo, one with hands over the head and one exposing the inframammary fold, can be beneficial as well for documentation purposes (Fig. 30‑3).

Diagnostic data in preparation for surgery would be similar for other elective major procedures and would be dependent on age, presence of comorbidities, as well as requirements of the surgical center in which the procedure will be performed. If per history there is reason to suspect preoperative anemia, a hemoglobin and hematocrit are obtained. Cardiac workup is dependent on patient age, history, and the facility in which the procedure is being done. In general, if an electrocardiogram is abnormal, internal medicine or cardiology clearance is mandatory. Breast reduction surgery can safely be done in an outpatient setting; however, patients with multiple medical comorbidities or difficulty with anesthesia may require an inpatient setting.
Deep vein thrombosis screening and appropriate prophylaxis should be undertaken. Using a model such as the Caprini Risk Assessment score was found to be effective for stratifying plastic and reconstructive surgery patients for venous thromboembolism risk. 4 Regardless of risk score, all patients should have pneumatic compression devices placed. While there is no consensus at present for perioperative chemoprophylaxis for many plastic surgery procedures, operative times greater than 2 hours can increase the risk despite the type of surgery. 5 As breast reduction surgery is elective, patients who fall into the highest risk category should only be operated on with extreme caution. Data are still lacking determining the safety profile, specifically incidence of hematomas, for use of chemoprophylaxis at this time. The authors’ preference is 40 mg subcutaneous unfractionated heparin in the preoperative holding area for most breast reduction patients with pneumatic compression devices placed prior to and functioning before induction in order for them to be effective.
All patients should be screened for tobacco use, including cigarettes, chew and vapors. For each cigarette, the peripheral blood supply is diminished for up to 90 minutes. The direct link between smoking and delayed wound healing represents an unfavorable shift of the risk-to-benefit ratio for breast reduction such that it should be avoided if possible. 6 Recommendations vary for smoking cessation prior to surgery from 2 to 4 weeks depending on surgeon’s preference. If needed patients should be referred to smoking cessation programs to help ensure their success. If there is any question whether the patient has abstained from nicotine, a urine cotinine test may easily be obtained in the preoperative area.
A common question from patients concerns insurance coverage of breast reduction surgery. Most insurance plans require a predetermination. This may simply require the plastic surgeon’s office notes documenting a detailed history of the patient’s symptoms and assessment of severity from the plastic surgeon, but may also require photographs, and documentation from a primary care physician describing the symptoms the patient has experienced and conservative measures taken and failed. Conservative measures generally include physical therapy, chiropractic treatment, ointments, powders, anti-inflammatory medications, and any other modifications made to treat the symptoms. An estimated weight of resection is made based on experience. Many insurance companies have adopted charts based on body surface area to estimate total resection need for coverage. These should be used as a guide, but the patient’s ultimate goals should be taken into consideration if there is any conflict with the amount of tissue needed to be resected for insurance approval. This is best handled talking directly with the patient about the situation in order to move forward. Whether or not insurance is involved, an estimated breast resection volume should always be documented prior to surgery for your reference and for medical record.
It is generally agreed that the same recommendations for screening mammography should be followed for preoperative workup for breast reduction. The American Cancer Society recommends that all women over the age of 40 years obtain yearly mammograms for so long as they are in good health. 7 Among women younger than 40 years, evidence supports use of the screening mammography for only those considered high risk for breast cancer. 8 As a result of breast reduction surgery, the breast parenchyma develops scarring and possible calcifications that may be seen on future mammograms. As such a mammogram prior to surgery in the above appropriate patients is recommended to rule out abnormal findings. Patients should also be informed that a baseline mammogram will be obtained 6 months after surgery to serve as a baseline study for comparison with future mammograms.
30.4 Treatment
30.4.1 Options and Indications
Indications for breast reduction surgery are straightforward for the most part. If a woman presents with a majority of the constellation of symptoms—macromastia with upper back pain, neck pain, headaches, bra strap grooving, and recurrent intertrigo of the inframammary fold—then she should benefit from a breast reduction.
Many procedural options are available for breast reduction and should be based on the patient’s morphology, nipple placement, previous surgeries, goals, and very importantly upon surgeon’s comfort level, training, and expertise with certain techniques. Many different reduction techniques can yield excellent aesthetic results with symptom relief. All described procedures are based on pedicles designed to support a viable, sensate nipple while allowing resection and reshaping of the breast parenchyma. The only two techniques that are an exception to this are liposuction only and breast reduction techniques involving free nipple grafting.
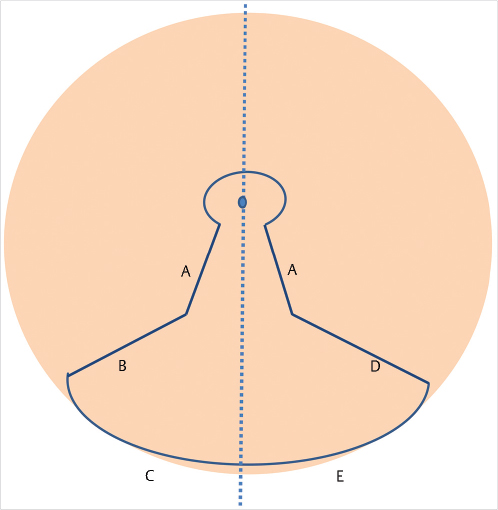
No matter the technique, five key steps are present in all: (1) Design a pedicle in order to keep the nipple–areola complex viable. (2) Decide how much and from where you will excise breast parenchyma. (3) Plan your skin access incisions. (4) Shape the remaining breast parenchyma. (5) Remove any excess skin. In order to reduce intraoperative blood loss, dilute epinephrine containing solution should be injected into the breast in all areas except the designed pedicle. The safety and efficacy of using epinephrine and tumescent solution in breast reduction has previously been reported. 9
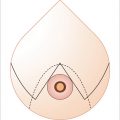
All patients should be marked in the preoperative holding area with patient sitting completely upright or in the standing position with shoulders even and rolled back and the face looking straightforward. No matter which technique is used, key markings should be placed on the sternal midline, breast meridians, inframammary fold, and desired position for the nipple–areola complex. The nipple–areola complex position is most often marked in the breast meridian at the level of the inframammary fold. This position can be adjusted intraoperatively after completion of breast shaping, if needed. A dire pitfall is marking the nipple–areola complex too high on the breast making it visible in a demi-cup bra or bathing suit. Should this occur, fixing the problem afterward can be almost impossible and should be avoided at all costs. Ideally the nipple–areola complex should sit at the area of most prominent projection of the breast. Keep in mind for vertical procedures that it should be placed somewhat lower to accommodate for the increased projection. If any uncertainty exists for placement of the nipple–areola complex, it is better to err on placing it slightly lower (Fig. 30‑4).
30.5 Surgery Procedures
Whether done as an outpatient or inpatient, reduction mammoplasty is mainly performed under general anesthesia. Despite the use of local anesthesia, for full patient comfort general anesthesia or deep total intravenous anesthesia is preferred. The patient is placed supine on the operating room table with both arms placed on arm boards and wrapped with padding beneath the elbows. It is very important to make sure the patient is centered and her shoulders are even on the operating table. Overlooking this simple detail can lead to asymmetric results. A single intravenous dose of a first-generation cephalosporin or clindamycin (penicillin-allergic patients) should be administered prior to the incision. 10 Evidence at this time supports the use of a single dose of perioperative intravenous antibiotic. However this is not common practice currently with more than 50% of plastic surgeons in the United States prescribing more than 1 day of antibiotics for breast reduction surgery. 11
After completion of the nipple–areola marking and delineating the pedicle, a wetting solution of 0.01% lidocaine with 1:1,000,000 epinephrine is then infiltrated into the breast parenchyma along the incision lines avoiding the parenchyma of the pedicle. Tumescent fluid is injected in a subdermal, wheel-like fashion within the pedicle to facilitate de-epithelialization of the skin overlying the pedicle. Any number of epinephrine-containing solutions can be used based on surgeon’s preference.
30.5.1 Surgical Options
Multiple methods for breast reduction have been described. Varying skin resection patterns and varying vascular pedicles for the nipple complex exist, each with potential advantages and disadvantages (Table 30‑1). The most common methods will be reviewed, with a detailed description of the authors’ favored method: superomedial pedicle combined with the inverted T scar pattern.
30.5.2 General Principles
The most common patterns for breast reduction are the vertical and Wise (inverted T) patterns. With either pattern, multiple pedicle options are available. Less common but also an option is the circumareolar pattern which works for a select population but has more limited access to the breast parenchyma with limited pedicle choices. No one approach will fit all patients such that it is up to the surgeon’s expertise and experience to decide which will be best suited for a patient. Breast shape is three-dimensional and when planning a breast reduction, this must always be kept in mind. Curvilinear incisions are preferred versus straight incisions in order to maintain a natural breast shape. Medial and upper breast tissue should be preserved as it is desirable in this location. The majority of resected breast tissue will come from the lower and lateral breast parenchyma. Depending on the technique, tissue may be removed from a desirable area; but as long as the breast shaping takes this into consideration and provides volumes to fill these areas the result will still be excellent. Skin plays little role in maintaining the breast shape in the long term and should be kept in mind when shaping the parenchyma.
30.5.3 Liposuction
This technique can be used in a specific population of patients to yield results. It relies on skin elasticity and retraction since no skin is resected and only fatty tissue is removed. It is good for women with mild volume excess with normal skin elasticity and mild ptosis, at most, who have a well-positioned nipple–areola complex at the apex of the breast. Tumescent fluid is injected into the breast and the inferior and lateral border of the breast are liposuctioned to reduce the fatty volume of the breast. The medial and superior poles are avoided to preserve the breast volume in those desirable locations. Liposuction only may also be the best option for a medically compromised patient, as it has a high safety index and a short operating room time compared to open techniques. This procedure can be used in those with greater degrees of ptosis or skin redundancy but will cause the breast to appear deflated with likely increased ptosis after surgery. Liposuction is not appropriate for adolescents and young adults, as their breasts are more fibrous and have little adipose tissue. But, for the rare patient who desires volume reduction for symptoms but is not worried about the skin excess or ptosis, liposuction may be a good option. Also in patients who present for secondary reduction with an unknown pedicle liposuction with skin only retailoring may be a safe and effective option.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree