Abstract
This chapter offers a concise discussion of fracture types, surgical management, and areas of concern for each type of fracture involving the head, neck, and scalp. Areas of concern during the physical examination are listed so that no structure potentially affected by a fracture is overlooked. Diagnostic procedures, involving tools such as computed tomography imaging, are reviewed, and then each major type of facial fracture—frontal bone, nasoorbitoethmoid, nasal bone, zygomaticomaxillary complex, orbital, LeFort/maxillary, mandible, panfacial—is thoroughly detailed. Postoperative care guidelines and long-term outcomes conclude the chapter.
19 Facial Fractures
19.1 Goals and Objectives
Understand the physical exam findings and diagnostic maneuvers associated with each fracture type.
Define the surgical indications for each fracture type.
Understand the general surgical management and specific areas of concern for each fracture type.
Discuss routine postoperative care of the facial trauma patient.
19.2 Patient Presentation
Patients with facial fractures have typically been involved in assaults, motor vehicle accidents, falls, sporting accidents, or work related injuries. With exception, most facial fractures are non-emergent, and other injuries should be thoroughly evaluated and potentially treated prior to management of facial fractures. Evaluation and management of the airway, hemorrhage, and neurologic injury are priority during initial assessment.
A thorough physical examination of the hard and soft tissues of the head and neck is paramount for the diagnosis of maxillofacial fractures. Frequently missed soft-tissue injuries include the posterior neck and scalp due to cervical collar placement, external auditory canal, nasal mucosa, and intraoral soft-tissue structures. Palpation of the bony skeleton for irregularities, crepitus, and mobility, should be performed over the zygomatic arches, orbital rims, zygomas, frontal bone, nose, and mandible.
Otoscopic evaluation should be performed with assessment of the tympanic membrane and soft tissues of the external auditory canal. Hemotympanum or mastoid ecchymosis may indicate a skull base fracture. An anterior canal laceration can be seen with condylar fractures or anterior auditory canal fractures.
The ophthalmic examination should include evaluation of the cornea, conjunctiva, anterior chamber, lacrimal apparatus, intercanthal distance, lateral and medial canthus symmetry in the frontal plane, and fundus examination. Any patient with a known orbital wall fracture with forehead paresthesia should be closely scrutinized for superior orbital fissure syndrome or orbital apex syndrome. Hyphema, findings supporting globe rupture, intraocular foreign bodies, change in visual acuity, or a lid margin laceration warrant ophthalmologic consultation.
Subconjunctival hemorrhage, an inferiorly displaced lateral canthus, and zygomaticofrontal suture step-offs can be seen with zygomaticomaxillary complex (ZMC) fractures.
Increased intercanthal distance (normal female: 32 mm, normal male: 34 mm), lacrimal injury with epiphora, decreased nasal air flow, and rounding of the medial canthus are seen with nasoorbitoethmoid (NOE) fractures. A Jones I and II test can confirm the presence of lacrimal duct injury. The bowstring test may demonstrate an undiagnosed medial canthus avulsion. ZMC, NOE, and orbital wall fractures may present with diplopia and restricted movement of the eye. Fractures involving the orbital floor or LeFort 2 fractures will often have concurrent infraorbital nerve injury, with paresthesia of the cheek, lateral ala, lower lid, maxillary teeth, and buccal mucosa. Fracture of the frontal sinus may demonstrate clear rhinorrhea, anosmia, or epistaxis. A beta 2 transferrin test of clear nasal discharge is used to diagnose a cerebrospinal fluid (CSF) leak.
An anterior open bite is the most common physical exam finding in patients with maxillary fractures. Midface mobility may be present. Lack of midface mobility does not preclude a fracture, as an impacted maxilla may not be grossly mobile. Epistaxis is common with maxillary, nasal, and NOE fractures.
A step in occlusion with associated open bite is common in mandible fractures. Floor of mouth ecchymosis is pathognomonic of symphysis or body fractures. Vertical collapse of the posterior ramus/condyle height causes a contralateral dental open bite. Bilateral condyle fractures result in an anterior open bite, which may be confused with a midface fracture.
19.3 Preparation for Surgery
Laboratory data in preparation for facial fracture repair is dependent on age and other medical comorbidities. In general, extensive laboratory workup specific for facial fracture repair is limited to only those tests needed to ensure that the patient can tolerate a general anesthetic.
A baseline ophthalmologic examination is cursory, and expert consultation should be obtained should there be any question as to ocular injury. While not warranted in every instance, complex fractures involving the orbit, concern for ocular injury, or extraocular muscle impairment require expert evaluation. In our practice, any patient requiring orbital fracture repair is evaluated by ophthalmology preoperatively to document a baseline examination. Neurosurgery evaluation should be obtained in every patient with concern for a CSF leak post trauma. Patients with hemotympanum, tympanic membrane perforation, external auditory canal wall laceration or fracture, temporal bone fracture, or significant change in auditory acuity warrant evaluation with an otolaryngologist.
Computed tomography (CT) imaging is the gold standard for diagnosis of maxillofacial trauma. In our practice, any patient with significant facial fractures undergo CT imaging with 1mm cuts reformatted in coronal and sagittal planes. Panorex imaging has some utility in the diagnosis and management of injuries involving any tooth-bearing segment of the jaws. Fractures isolated to the mandible only, with no other distracting injury, may be diagnosed by Panorex in conjunction with other plain film modalities like the submentovertex or reverse Towne’s view plain films. Reliance on a single plain film view of the mandible can result in undiagnosed fractures. No matter the modality, a systematic approach to reviewing facial radiographs is critical given the complexity of the anatomy.
Most facial trauma involves the oral cavity or nose, creating specific concerns for the provider managing the airway. Airway emergencies are minimized with discussion of airway management with the anesthesia provider. Any dentate patient with a fracture involving the mandible or maxilla should undergo nasal intubation to allow maxillomandibular fixation. A sphenoid sinus fracture, or fracture involving the skull base, should alert the surgeon to possible inadvertent entry of a nasal endotracheal tube or any tube into the middle cranial fossa or adjacent spaces. 1 In pan facial fractures involving the mandible and maxilla, surgical airway management should be performed. In patients not requiring long term ventilator support, submental intubation provides the ability to perform maxillomandibular fixation (MMF) without the morbidity of tracheostomy. 2 In patients requiring long term ventilator support, tracheostomy should be performed.
19.4 Treatment
19.4.1 Frontal Bone Fracture
Frontal sinus fractures are generally caused by anterior blunt force trauma. The leading mechanism is motor vehicle accidents. With the increasing use of seat belts and airbags, there has been on overall decrease in incidence of frontal sinus fractures. 3 Other mechanisms of fracture include sports injuries, falls, falling objects, and interpersonal violence.
While many classifications of frontal sinus management exist, consideration for repair hinges on displacement of the anterior or posterior table and the patency of the nasofrontal duct. Patients with non-displaced frontal sinus fractures that involve the anterior or posterior tables, with an intact nasofrontal duct (NFD), and without the need for neurosurgical access should be managed non-operatively. Nasal precautions with avoidance of Valsalva maneuvers, closed mouth sneezing, or heavy lifting should be instated.
Any patient with a comminuted/significantly displaced (greater than the width of the outer table) posterior table fracture or with significant brain injury or dural tear should undergo cranialization of the frontal sinus and repair of the anterior table. In patients with a displaced anterior table fracture and intact NFD, anterior table repair only, without obliteration, should be performed. In patients with a displaced anterior table fracture with NFD involvement, obliteration of the frontal sinus should be performed with complete removal of all sinus lining. In patients with non-displaced anterior or posterior table fractures with NFD injury, reduction of the NOE component should be performed with evaluation of the NFD. If the NFD is not patent, then obliteration with removal of all sinus lining should be performed. 4
The frontal sinus is approached through existing lacerations, or via a bicoronal incision. Anterior table reduction techniques vary from simple elevation of bone fragments without fixation to removal of bone fragments and orientation extracorporeal with fixation and reimplantation. It is important to maintain orientation of the fragments. Traumatic distortion of the segments may occur. It may be necessary to trim the margins of the fragments to assist in the reduction of comminuted segments.
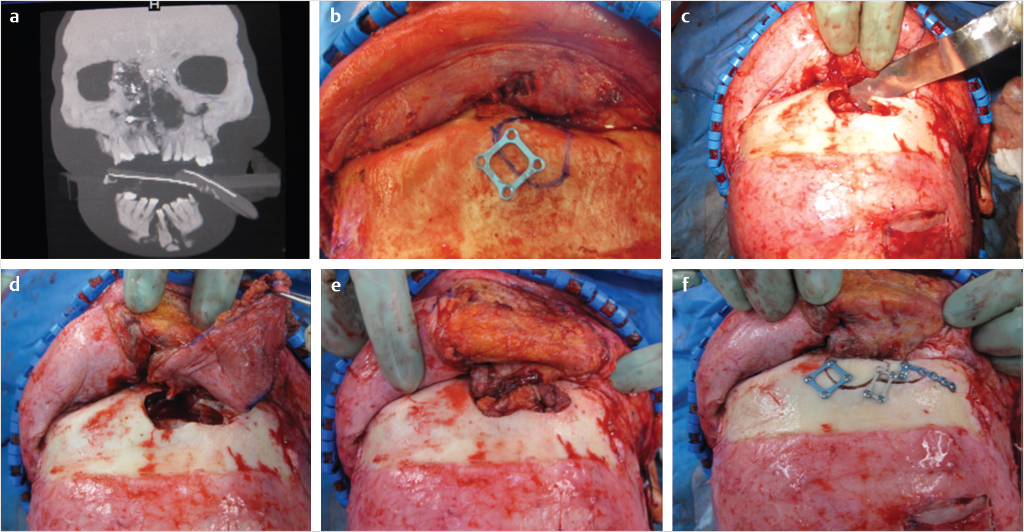
Exploration, sinus mucosa removal, closure of the NFD, and obliteration of the frontal sinus presents specific challenges. When sinus mucosa removal is indicated, removal of the entirety of the anterior table is indicated. A forceps can be placed into the sinus to define the boundaries of the sinus which are subsequently marked. The anterior table is indexed with fixation, the plates are removed, and the bone is subsequently osteotomized. The anterior table is then elevated and removed. All sinus mucosa and septae should be removed with diamond burs. Placement of methylene blue in the sinus prior to mucosa removal may help in preventing missed areas of sinus mucosa (Fig. 19‑1).
NFD obstruction is accomplished with elevation of the sinus mucosa in the frontal recess, which is then inverted and compressed inferiorly to obstruct the ducts. Bone, fat, fascia, or muscle may be placed into the recess. Obliteration of the sinus is accomplished with bone, bone substitutes, fat, pericranium, and muscle. Fat remains the most commonly used and studied material. 5 Synthetic resins should be avoided as they create an avascular medium with high potential for infection. 6 Posterior table fractures, dural repair, and cranialization are generally managed in conjunction with neurosurgery and are beyond the scope of this text.
Paramount to any frontal sinus repair is evaluation for a CSF leak. Clear rhinorrhea may be evaluated intraoperatively with a halo test, though this has low specificity and sensitivity. Fluid testing positive for beta-2-transferrin is diagnostic of a CSF leak. Most CSF leaks resolve spontaneously; however, persistent leaks may require cranialization and dural repair. Lumbar diversion may play a role in management of some leaks.
Complications of frontal sinus injury can be subdivided into early (<6 months) and late (>6 months). Early complications include sinusitis, CSF leak, and meningitis. Late complications include mucoceles, mucopyoceles, and brain abscess. 7 Late complications may present years later, therefore long-term surveillance with imaging is indicated.
Advancements in endoscopic sinus surgery have generated interest in treatment of anterior table fractures with NFD injury. Anterior table repair without obliteration with antibiotic administration and serial computed tomography is advocated by some authors. 8 NFD patency may spontaneously occur after repair of the anterior table in a majority of patients, with select patients requiring secondary endoscopic sinus surgery for NFD outflow obstruction. Expert consultation with an otolaryngologist may be warranted in select cases.
19.4.2 Nasoorbitoethmoid Fractures
The nasoorbitoethmoid (NOE) complex is the confluence of the nose, orbits, ethmoids, inferior frontal sinus, and floor of the anterior cranial base. Like frontal sinus fractures, NOE fractures are generally the result of blunt-force trauma to the midface. CSF leak, orbit, globe, nasolacrimal duct, nasal, and intracranial injuries are frequently seen in association with NOE fractures. The classic fracture pattern involves lateral nasal bones, inferior orbital rim, medial orbit/ethmoid wall, nasal maxillary buttress at the piriform aperture, and the junction of the frontal process of the maxilla with the frontal bone. The NOE region involves the major central vertical (nasomaxillary) and horizontal (frontal and inferior rim) buttresses of the face. Re-establishment of an ideal nasofrontal angle (115–130 degrees), nasal projection, and intercanthal distance are critical in appropriate repair.
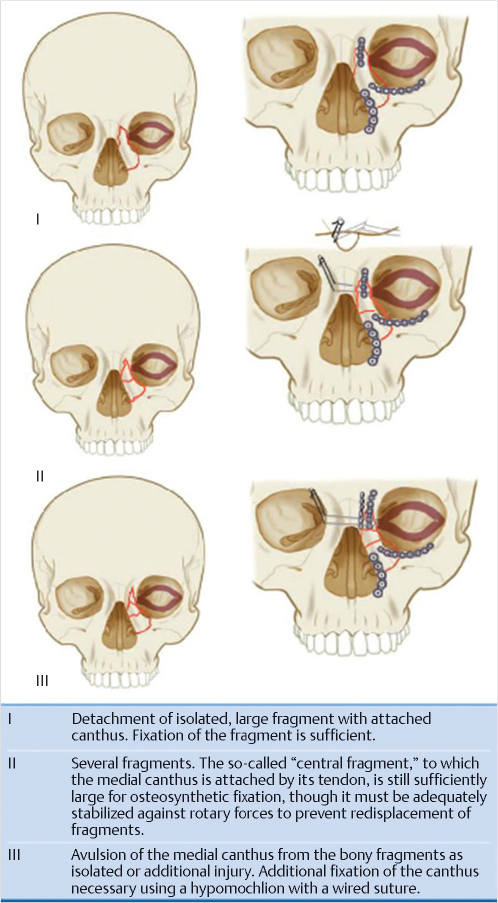
The medial canthal tendon (MCT) divides into anterior and posterior limbs which attach anteriorly along the anterior lacrimal crest and posteriorly along the posterior lacrimal crest. The MCT envelopes the lacrimal sac. The classification developed by Markowitz et al evaluated the MCT attachment and degree of comminution of the NOE fragment. 9 In type 1 fractures, the MCT remains attached to a large bony segment (central fragment) without comminution. In type 2 fractures, the NOE segment is comminuted with the MCT remaining attached to the central fragment. In type 3 fractures, there is comminution of the NOE segment with detachment of the MCT. A type 1 fracture is typically discernable from a type 2 or 3 fracture radiographically. MCT avulsion is generally determined intraoperatively making preoperative diagnosis of a type 2 versus type 3 fracture difficult (Fig. 19‑2).
Open reduction internal fixation for NOE fractures is indicated in all type 2 and 3 fractures, and in type 1 fractures with clinically significant displacement resulting in telecanthus or malposition of the MCT. In type 1 fractures with no clinically significant displacement and no mobility of the MCT, close observation of the fracture may be employed.
The NOE complex requires superior and inferior component access. As with all fractures, existing lacerations may be used. The superior NOE complex (nasofrontal region) is approached through a bicoronal incision with degloving of the superior and medial orbits. Scoring of the periosteal envelope over the radix reduces tension when retracting inferiorly. The inferior NOE complex is approached through a transconjunctival or external lower lid incision. Medial orbital/NOE exploration is facilitated with a transcaruncular incision if needed. The gullwing, extended glabellar incision, and Lynch incision are generally not recommended due to poor cosmesis. The piriform rim may be plated via an intraoral maxillary vestibule incision.
The sequencing of NOE complex repair after surgical exposure is as follows: the MCT is identified, the medial orbital rims followed by medial orbital walls are reconstructed, transnasal canthopexy is performed, the nasolacrimal apparatus is repaired, the nasal dorsum is reconstructed, the soft tissue is closed and the medial canthal soft tissue is bolstered. 10 If the MCT is not readily apparent, identifying the nasofrontal suture and dissecting inferiorly and posteriorly leads to the apex of the lacrimal fossa. The medial orbital rims are reduced and fixated with rigid fixation. Transnasal wiring posterior to the lacrimal fossa may assist in reduction of the medial orbital walls. Roughly half of all patients with NOE fractures required bone grafting or alloplastic reconstruction of the medial orbital wall. Inadequate medial reduction and anterior projection leads to cosmetic deformity with telecanthus that is exceedingly difficult to repair secondarily. Over-reduction is effectively impossible and leads to less postoperative complaints than under-reduction (telecanthus).
The transnasal canthopexy is the most difficult aspect of NOE repair. Fortunately, only 3% of patients require canthopexy. The MCT may be posteriorly approached through the coronal approach or anteriorly with a small incision through dermis 3mm to the medial canthus. There are multiple techniques to anchor the MCT to a point of attachment (transnasal wire, plate, screw). Regardless of the technique, the point of attachment should be located superior and posterior to the posterior lacrimal crest. Primary repair of the nasolacrimal apparatus is controversial and beyond the scope of this text (Fig. 19‑3).
Dorsal nasal support should be evaluated and repaired primarily. Dorsal nasal grafting is indicated if the cartilaginous or bony septum is significantly comminuted with anticipated loss of vertical support of the nasal bones and upper lateral cartilages. 11 A calvarial or costochondral graft may be utilized. The distal margin of the graft should be tucked under the lower lateral cartilages to prevent palpability.
The soft tissue of the medial canthal region is degloved during NOE repair. Tight adaptation of this region may be accomplished with medial canthal bolstering. A large nonresorbable suture may be passed from the medial canthal region, transnasal, to the contralateral medial canthal region. The suture may be passed back, and any type of bolster material (Xeroform) can be secured. The bolster is removed at 7 to 10 days. 12
Two main complications arise after NOE repair. Persistent telecanthus results from inadequate medial reduction and soft-tissue management postoperatively. Secondary repair is exceedingly difficult and often is unsuccessful. Like primary repair, secondary repair should focus on addressing both the hard and soft tissue. Epiphora occurs in approximately half of all NOE fractures immediately postoperatively. 13 Most resolve after soft-tissue swelling decreases with only 5–10% of patients having persistent nasolacrimal duct obstruction. 9 Persistent epiphora should be treated no earlier than 6 months after NOE complex repair.
19.4.3 Nasal Bone Fractures
The nasal bones are the most commonly fractured facial bone. 14 While primary repair of nasal bone fractures is generally “simple,” unfavorable results occur frequently. Open repair and posttraumatic repair are beyond the scope of this text. History should include mechanism of trauma, direction of impact, history of prior nasal trauma, discussion of prior nasal asymmetry and photographic evaluation. All patients should be evaluated for the presence of a nasal septal hematoma. If present, incision and drainage of the hematoma should be performed.
Indications for repair are esthetic and functional when nasal obstruction or airway compromise has occurred. Contraindications to closed reduction include severe comminution of the nasal bones or septum, associated displaced orbital wall fracture, caudal septum fracture dislocation, open septal fracture, and fractures greater than 3 weeks old. In the case of displaced orbital wall fractures, the orbital wall should be repaired prior to closed reduction of the nasal bones.
Fracture repair may be performed under local anesthesia or general anesthesia. In our practice, a general anesthetic is preferred as epistaxis is common following closed reduction. Local anesthesia administration should focus on regional blocks to the infraorbital, infratrochlear, supratrochlear, external nasal, and nasociliary nerves. The administration of an appropriate amount of local anesthesia with epinephrine to regional blocks prevents distortion of the nasal dorsum and ala. Judicious use of oxymetazoline spray, local anesthesia with epinephrine, and phenylephrine soaked cottonoids reduce the volume and incidence of epistaxis.
After reduction of the nasal bones, splinting should focus on three anatomic regions of importance. The external nose should be protected with an external splint, and the nasal septum should be maintained at midline with internal splints (Doyle, Merocel, etc.). The internal nasal valve is often overlooked and inadequately supported. Placement of bacitracin coated 1/4” strip gauze into the internal nasal valve helps prevent internal valve collapse. All patients with nasal packing should be placed on prophylactic antibiotics to prevent or limit the development of sinusitis and Staphylococcus aureus infection that could lead to toxic shock syndrome.
Pediatric nasal trauma is uncommon due to lack of projection and elasticity of the underdeveloped nasal bones and associated cartilage. There is significant nasomaxillary growth that occurs from the cranial base centered at the nasofrontal suture and nasal septum. 15 Most nasal growth is complete by age 5; however, significant vertical growth limited to cartilage and soft tissue occurs after this age. Because of this, pediatric patients should be counseled that secondary rhinoplasty is highly likely. Addressing nasal airflow and traumatic nasal deformities should be delayed as long as reasonably possible until growth of the nasomaxillary complex is complete.
19.4.4 Zygomaticomaxillary Complex Fractures
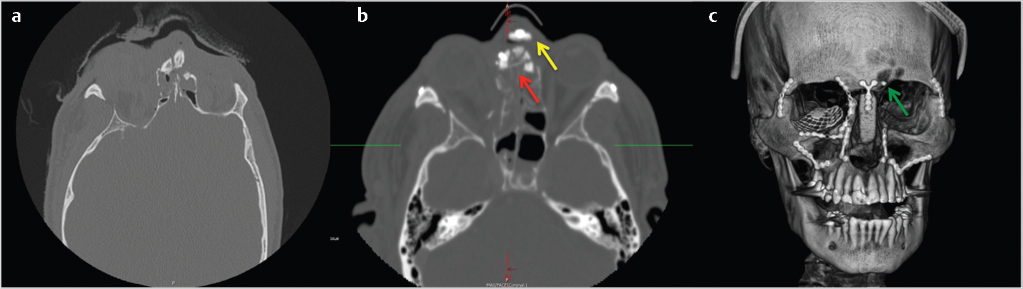
Zygomaticomaxillary Complex (ZMC) fractures are the most common midface fracture. The ZMC is a tetrapod structure with articulations classically described in four areas: (1) the zygomaticomaxillary buttress (ZMB), (2) the infraorbital rim (IOR), (3) the frontozygomatic suture (FZ), and (4) the zygomatic arch (ZA). The fifth articulation, and most reliable in determination of adequate reduction, is the zygomaticosphenoid suture (ZSS). The ZMC fracture propagates through the floor and lateral walls of the orbit (Fig. 19‑4).
Separate classifications by Manson et al and Zingg et al evaluated the degree of displacement and comminution of the ZMC. 16 , 17 The ZMC can be fractured at one or more of the previously noted articulations in the Manson low energy fracture, or Zingg type A fracture. Fracture of all articulations of the ZMC without comminution occurs in Manson medium energy fractures, or Zingg type B fractures. Manson high energy fractures, or Zingg type C fractures, result in comminution and displacement of the ZMC.
Indications for surgery are both aesthetic and functional. Significant aesthetic compromise can occur with bizygomatic widening, decreased malar projection, and displacement of the lateral canthus. Functional indications for repair are enophthalmos, diplopia, or restriction of mandibular movement due to compression of the muscles of mastication below the zygomatic arch. Contraindications to surgical repair include no functional impairment, a high-risk surgical candidate, minimally or nondisplaced fractures, and severe contralateral globe injury with vision loss or impairment.
Given the variation in displacement and location of fracture of the ZMC, difficulty surrounds three questions: (1) When should the orbit be explored? (2) How much exposure is required to verify adequate reduction? (3) Should fixation be applied, and where?
With the advent of CT scans, orbital exploration when treating ZMC fractures decreased from 90 to 30% in the late 1980s. 18 Surgical exploration and repair of orbital wall fractures center around function (diplopia) which cannot be fully determined at the time of repair. Evaluation of entrapment with a forced duction test is mandatory after reduction of the ZMC. The presence of entrapment or significant enophthalmos are indications for orbital exploration. Preoperative CT evaluation with greater that 50% of the floor fractured with soft-tissue herniation has been advocated as a guideline for repair of the floor. 19 In general, low-energy fractures involving isolated articulations do not require orbital exploration. High-energy ZMC fractures often require orbital exploration and repair (Fig. 19‑5).
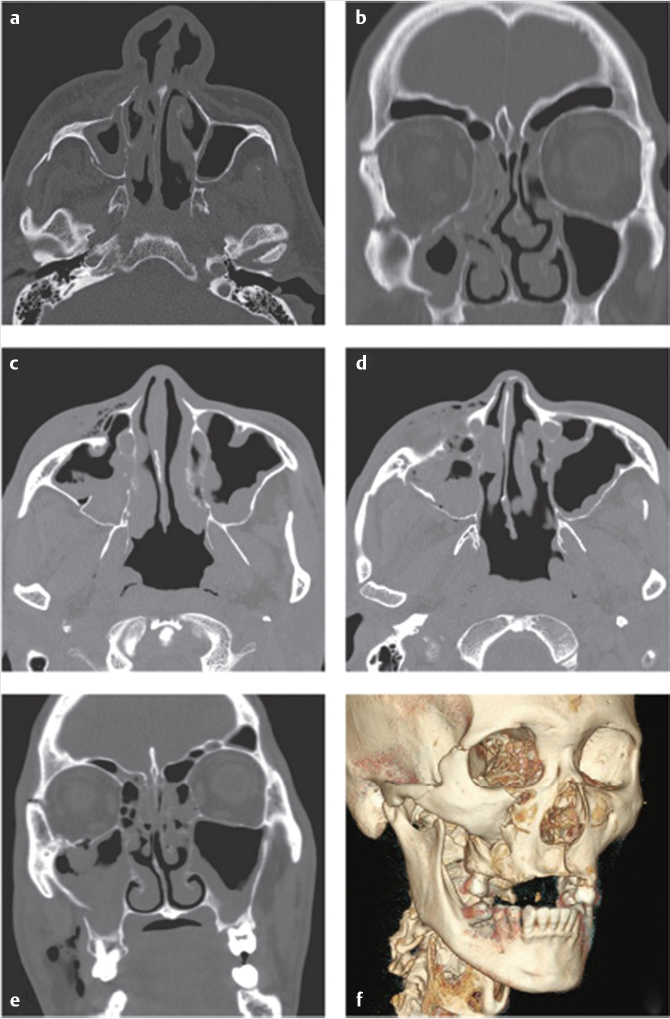
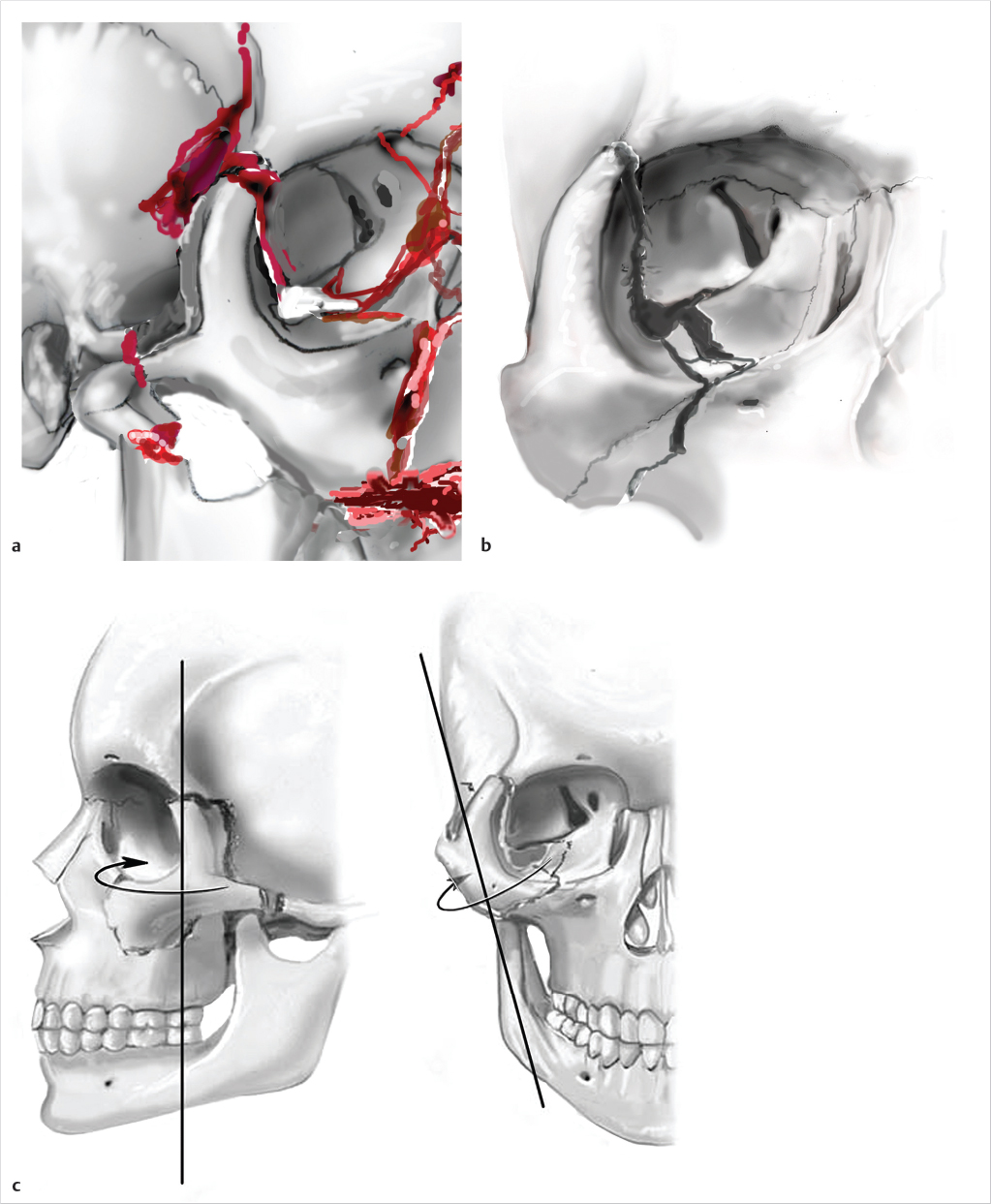
Rotation of the ZMC, in addition to displacement, creates challenges to ensure appropriate reduction. Axial rotation of the complex around any articulation may demonstrate adequate reduction at an isolated articulation, while globally the ZMC is still significantly displaced. The zygomaticosphenoid suture (ZSS) is the longest line of fracture and provides the most reliable indication of adequate reduction. The frontozygomatic suture does not reliably demonstrate adequate reduction of the ZMC due to ease of rotation of the complex around one point. Open evaluation of at least 3 points of articulation is typically recommended in significantly displaced medium and all high-energy fractures. Utilization of a Carroll-Girard screw or a Rowe elevator can be useful in mobilization of the ZMC.
While discussion of fixation is important, it should be stressed that reduction is the key to operative success. Ellis demonstrated that there was no perceptible change in ZMC position post-operatively when comparing fractures with and without fixation. 20 He suggested that post-operative asymmetry was likely secondary to unsatisfactory primary reduction. Fixation of the ZMC is primarily at the FZ and ZMB with the IOR as a secondary location for fixation. Fixation of the zygomatic arch is reserved for severely comminuted fractures or when coronal access is utilized for fixation of other fractures. The ZSS is rarely fixated. One point fixation is typically at the ZMB and two-point fixation is at the ZMB and FZ. Three or four point fixation including the IOR and ZA is reserved for significantly displaced or comminuted fractures. Should three or four point fixation be employed, orbital exploration should be considered given the high likelihood of significant floor displacement. With concomitant NOE and ZMC fractures, one must carefully consider fixation sequencing. When employing an “outside to inside” approach during treatment of multiple midface fractures, ORIF of the IOR to a laterally displaced NOE fracture can appear as an adequately reduced ZMC fracture. Significant bizygomatic widening can occur. It is the preference of the author to approach concomitant NOE and ZMC fractures medial to lateral in all but the most comminuted NOE fractures.
While discussion of all surgical approaches is beyond the scope of this chapter, careful consideration of the surgical approach is important. If evaluation of the ZF is indicated, the ZF and ZSS should be accessed simultaneously. An upper blepharoplasty incision is preferred approach for ZF/ZSS evaluation. The lateral brow incision should be discouraged due to poor cosmesis. If the IOR and floor are to be explored in addition to the ZF/ZSS, a transconjunctival incision with lateral canthotomy or subtarsal incision provides access to all of the aforementioned articulations. The ZMB should be accessed intraorally through a maxillary vestibular incision. Orbital floor exploration typically requires an orbital incision; however, endoscopic evaluation and management can be employed via the maxillary vestibular incision. The inferior orbital rim incision (directly over the infraorbital rim) is contraindicated due to morbidity and poor cosmesis.
The isolated zygomatic arch fracture has specific management concerns. Given the morbidity of a direct open approach, two alternative surgical approaches exist. The indirect open “Gillies” approach via a temporal incision allows insertion of an elevator deep to the temporalis fascia and superficial to the temporalis muscle to reduce the zygomatic arch fracture. Careful dissection prevents hemorrhage from the temporalis muscle. The “Keen” approach utilizes a small 2–3cm maxillary vestibular incision along the posterior maxillary buttress allowing indirect open access to the arch. It should be noted that both techniques are supraperiosteal, and rough manipulation of the tissues may result in neurovascular damage. Reduction of the arch confirmed by manual palpation is often adequate. Transcutaneous circumzygomatic arch wiring has been described with external splinting. Open fixation of the arch is via coronal access.
There are multiple complications that may occur related to ZMC fractures. In general, inappropriate reduction perioperatively is the cause of a preventable bony cosmetic deficit, and surgical access leads to the majority of soft-tissue complaints.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








