14 Postoperative Management
Summary
The concept of breast augmentation as a Process is helpful both as a means to present breast augmentation to patients and as a guide for management to optimize results. The Process of breast augmentation is the most powerful concept in the specialty to practice this discipline at its highest level. All patients must understand that participation in postoperative routines is a critical element for a successful outcome, as each postoperative visit is an opportunity for refinement and improvement of a result. The authors found that most patients appreciate that breast augmentation is presented in this way, as the passion for great results and teamwork needed to get there are readily apparent.
Key Points
Defined postoperative care is the final and fourth part of the process of breast augmentation.
The more patients know and less surprises that patients have, the better they do.
Routine postoperative plan minimizes adjuncts and enhances patient recovery and experience.
14.1 Introduction
Defined postoperative management is the cornerstone of success in the postoperative phase of breast augmentation. It is also important to keep in mind that this is the fourth and final subprocess for the process of breast augmentation1. As mentioned previously, each step synergizes with the preceding and subsequent steps, resulting not only in the antegrade process but also multiple levels of feedback that reinforce previous steps and facilitate successful completion and outcomes for the latter subprocesses. Postoperative regimen and ultimately the patient experience can be virtually fully defined through the first three subprocesses (patient education, tissue-based planning, and refined surgical technique with fast-track 24-hour recovery) with the actual postoperative management occurring in seemingly passive fashion.
Discussing postoperative management in general can be a difficult task, as there are many different concepts used in the postoperative management of a breast augmentation patient. Nevertheless, certain concepts hold true of all postoperative management regimens regardless of the details. These include
Defined plan.
Minimize adjuncts.
Enhance overall patient experience.
This chapter offers suggested routines for the procedure types detailed in Chapters 7 through 10. The regimen discussed herein has been utilized by multiple surgeons with verifiable, peer-reviewed published outcome data. Use of postoperative drains is certainly surgeon dependent; however, with use of the techniques described in this book, including a precise bloodless dissection, postoperative drains have not been found to be necessary in primary augmentation, and it is universally known that patients despise having drains. Therefore, avoiding drains postoperatively has been a major benefit in the overall patient experience.
14.2 Inframammary Approach
s. Tab. lists the main components of the postoperative phase.
The goal is to minimize all adjuncts. Patients should not use special bras, straps, drains, pain pumps, or any other device or tactic to decrease pain, as these tend to slow recovery. In multiple peer-reviewed published series, narcotics have been eliminated from the routine postoperative phase with excellent results. 1 , s. Literatur , 3 A cyclooxygenase 2 (COX-2) inhibitor has been given in one dose preoperatively and ibuprofen 800 mg t.i.d. p.r.n. in the postoperative phase. Pain pumps have been developed; however, these have not been found to add an additional level of analgesia but certainly add cost and a hassle factor to the recovery phase. Exparel (liposomal bound bupivacaine) has proven effective for postoperative pain control; however, it is quite expensive and given the process for fast-track 24-hour recovery it is not cost-effective for breast augmentation.
Probably one of the most important aspects of the postoperative phase is the specific detailed postoperative instructions (s. Abb.) including arm raises, which patients do five times every hour while awake for the next 5 days. Patients are instructed to avoid sedentary behavior the first 2 to 3 days postoperatively. It is recommended that patients go out shopping and to dinner on the day of surgery, and this is important to prevent patients from not being active during window of recovery that lasts for approximately 6 to 8 hours after a breast augmentation. This window of recovery is an important phase and has not been previously described to the authors’ knowledge. Following a breast augmentation, patients have 6 to 8 hours to resume normal light activities of daily living before they become extremely stiff and sore and it becomes excessively hard to get back to these activities. For this reason, the instructions to resume light activities with specific light arm raises immediately following the surgery are extremely useful to maintain the patient in this window of recovery. It is also important to have at least one phone call postoperatively to make sure the patient is following the instructions and has no questions. The timing of this call should be following the 2-hour nap and should ensure that the patient is on a normal course. Patients who are not following the prescribed course will need to be redirected as soon as possible to avoid issues with their recovery.
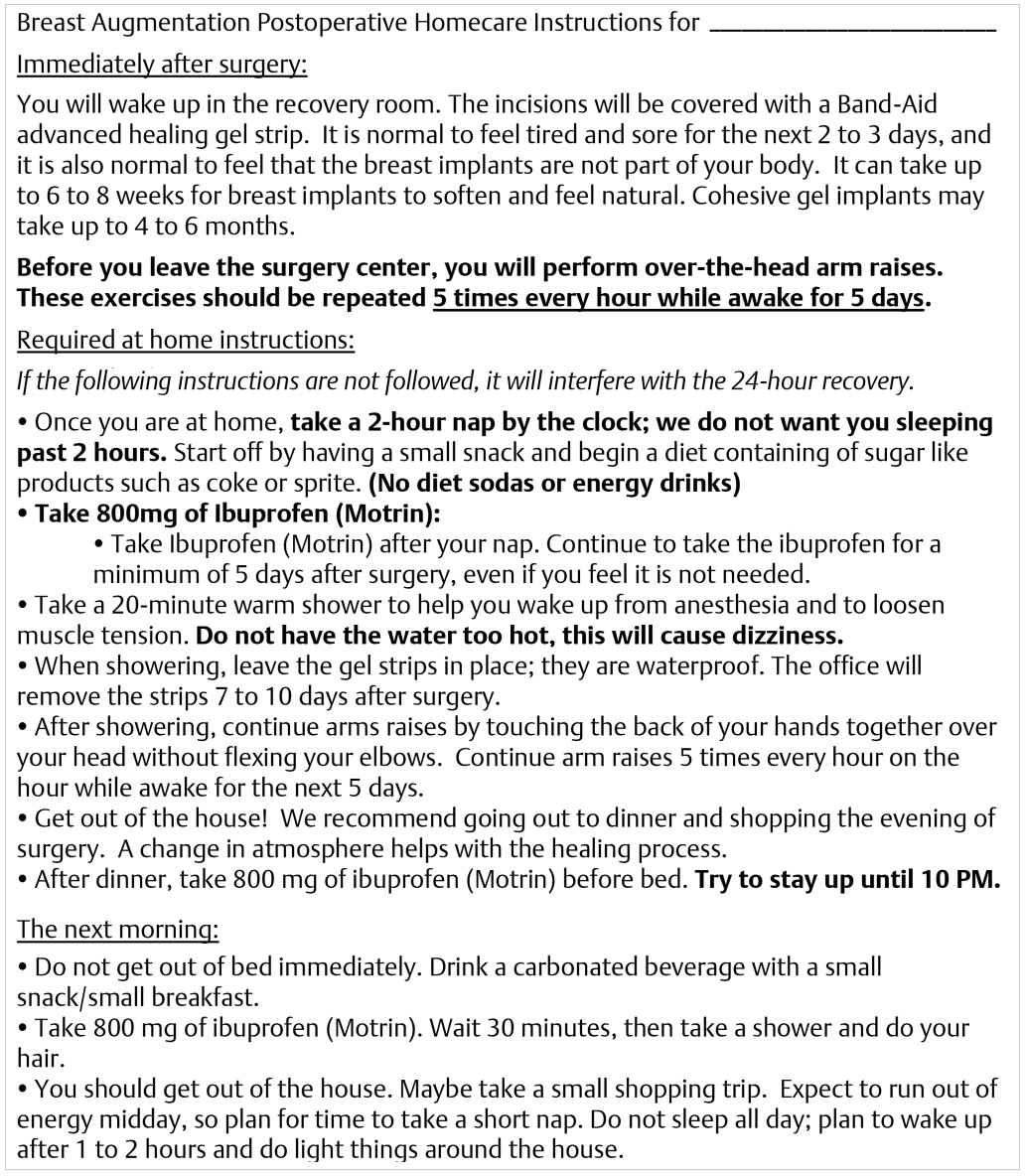
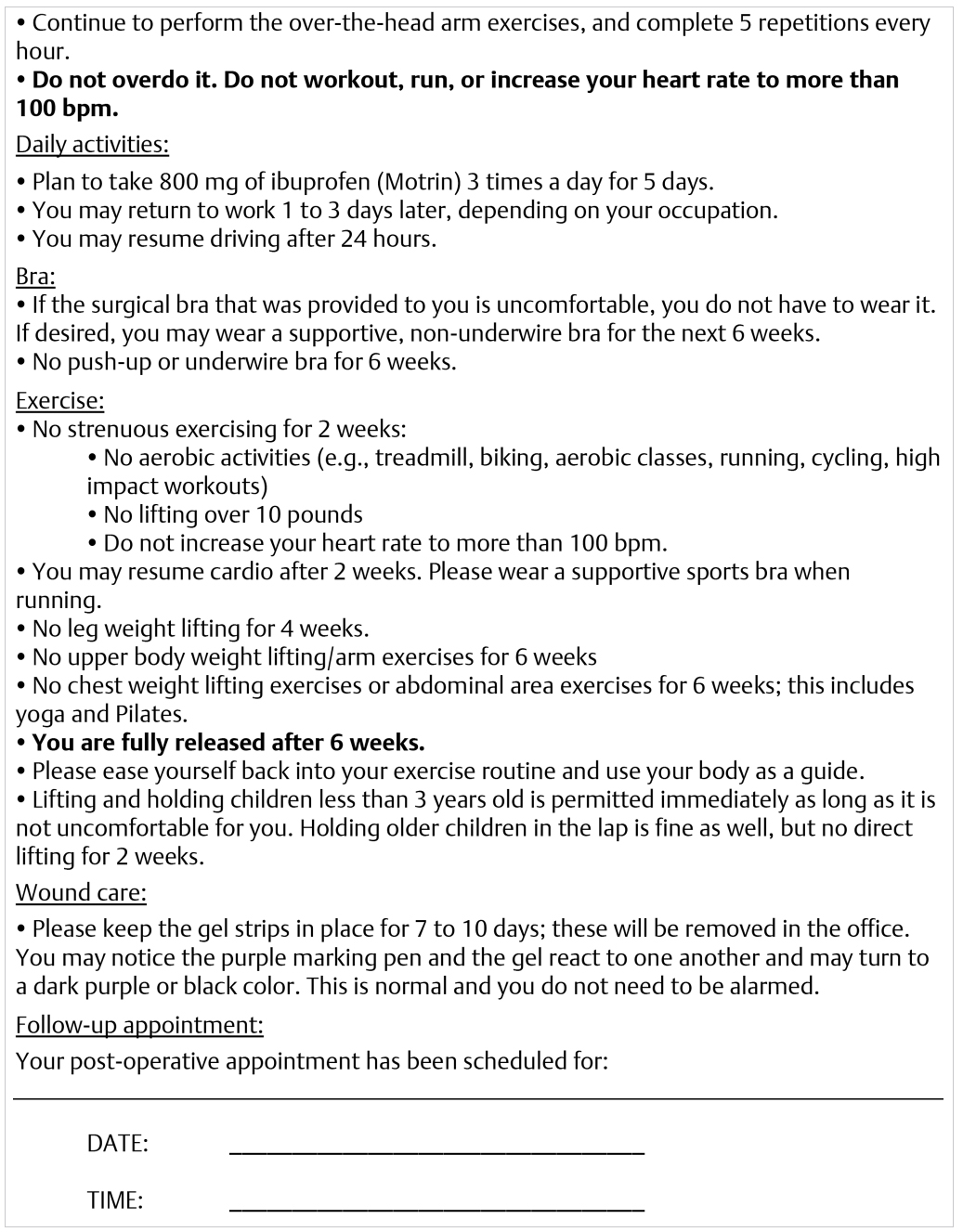
Other postoperative management points include the use of a bra, which has been found to be optional. This is clearly not needed if a pocket is dissected precisely; however, there are some patients who prefer wearing a bra and some patients who prefer not wearing a bra. With an atraumatic precise pocket dissection as described in preceding chapters, a bra may be worn if the patient desires. It is recommended that no push-up bras are worn for 6 weeks. A bra is recommended for patients with shaped implants. A tight-fitting bra may be useful in the cases where an overdissection of the pocket has been identified.
Implant displacement depends on the type of implant. Displacement is generally recommended for smooth, round implants only. Implant displacement would not be recommended for textured devices, most notably shaped implants. The follow-up intervals are also defined and should be fairly frequent for the first year postoperatively. The authors’ recommended follow-up is at 5 days, 1 week, 3 months, and 1 year, and then annually following the first year visit. Most problems with breast augmentation may be identified within the first year postoperatively, and it is important to closely monitor and address these problems should they arise.
Management of the scar regardless of its location is important. Scar therapy routines include use of silicone back strips, Band-Aid gel strips, Mepiform, and scar massage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree