10 Periareolar Mastopexy Augmentation
Summary
Periareolar mastopexy augmentation is a technique to correct minor ptosis of the breast without extense scars. The ptosis is treated with periareolar ressection of the skin, providing the final scar around the areola in an upper position. It’s possible to improve breast and areola simmetry, as reduce the diameter of areola. The goal of this approach is to choose the minor ptosis and explain to the patient the possibility of a lower pole overprojection instead of extense scars. Round block suture is important to maintain the scar and the areolar with the better result aesthetically.
Key Points
Periareolar mastopexy is an important option to minimize scars in minor ptosis cases.
It is indicated to elevate nipple–areola complex and breast mound.
A mastopexy or reduction without an augmentation can result in lack of projection and desired volume.
10.1 Introduction
Correcting different degrees of breast ptosis with a single-stage augmentation/mastopexy procedure entails the challenge of augmenting breast volume with a silicone implant while resecting excess skin and concurrently relocating the nipple–areola complex (NAC) and obtaining a full upper pole.
Periareolar and vertical techniques for mastopexy were developed to minimize scars in minor ptosis cases. The periareolar technique was first described by Bartels et al. 1 In 1980, Gruber and Jones presented the donut mastopexy with its indications and associated complications. 2 This technique was popularized by Benelli 3 and Góes. 4
In augmentation mammaplasty, the selection of surgical approach for implants is based on the characteristics of each patient and the tissue conditions to ensure an optimal covering of these. The site must not be arbitrarily based on the preferences of the surgeon and the patient, but must ensure adequate tissue covering, thus minimizing short- and long-term risks. Circumareolar incisions in breast augmentation surgery can center slightly low areolas on the breast mound and treat minor to moderate ptosis. This maneuver, however, is limited to moderate cases because it does not achieve huge lifting of the breast.
Objectives of periareolar breast augmentation surgery are as follows 5 , 6 :
Less invasive surgery, suitable for minor ptosis degrees.
Elevation of the NAC.
Conversion from a ptotic breast to a conical breast.
Elevation of the mound.
Enlargement of volume/breast volume improvement.
Improved breast symmetry.
Minor scars/limited skin excision.
Preserve the integrity and the entire soft-tissue thickness of the breast’s lower pole.
Patient education and counseling of a possible lower pole overprotection instead of a vertical scar.
The conflicting goals of mastopexy and breast augmentation, one that reduces and one that fills it up, lead to additional risks of breast augmentation and mastopexy and magnifies them. 7 , 8 , 9 These include the following:
Increased risk of implant infection with either an exposure or malposition.
Increased risk of nipple or flap necrosis.
Uncertainty about nipple-to-breast and implant relationships with potentially worse scars and decreased nipple sensation.
Relapse of the associated ptosis and spreading of the areolar scars can be addressed, to some extent, by converting the periareolar mastopexy to a vertical or inverted T-scar procedure.
Periareolar mastopexy is mostly indicated to younger patients with good skin thickness and elasticity. The best candidates for mastopexy and augmentation are the worst candidates for mastopexy or breast reduction alone because the shape is discoid and the skin is very loose and distensible. 10 , 11 , 12 Firmer breasts with preserved integrity of Cooper’s ligaments are also desirable for better results.
10.2 Technique
Skin markings are done with the patient in stand-up position. Precise measurements must be taken using the inframammary fold (IMF), the NAC, and the suprasternal notch as key landmarks.
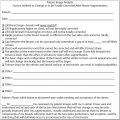
The midline of the chest and IMF are marked. Lines are drawn first straight down the midline from the suprasternal notch to the xyphoid process and second from a point 5 cm from the suprasternal notch at the clavicle to the NAC and then straight down to the areola. Setting the nipple height is extremely important. The position is determined by multiple factors. The distance from the sternal notch to the nipple should be in a range of 17 to 19 cm and it is influenced by height, breast, and body type.
The amount of excess skin is estimated and then a periareolar shape (oval in stand-up position) is marked around NAC. The inferior margin should be from 4.5 to 5.5 cm from IMF. The medial margin should be marked approximately 9 cm from medial line (Fig. 10‑1). Footprint of breast tissue is marked all over the breast to settle undermine limits.
The ideal size and shape of the female breast is inherently subjective and relates to both personal preference and to cultural norms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree