Abstract
Vesicles and bullae, when intact, are easily recognized primary lesions ( Table 10.1 ). Crusts (dried serum and blood) are secondary lesions that should lead one to suspect a preceding vesicle/bulla or pustule. The etiology of vesicular and bullous diseases includes viral and bacterial infections, allergic and irritant contact dermatitis, and autoimmune, genetic, and metabolic diseases. Pathogenesis of the blister formation is helpful in understanding the location of the lesion within the skin. The blister may occur within the epidermis (intraepidermal) or beneath it (subepidermal).
- 1.
Blistering is an easily recognized primary lesion
- 2.
Weeping and crusting suggest a blistering process
- 3.
There are multiple causes of blistering
Where blisters occur in the skin helps in making the diagnosis
- 1.
Intraepidermally
- 2.
Subepidermally
The following diseases illustrate the pathogenetic mechanisms involved in blister formation at the different levels of the skin. Detachment of the horny layer by an epidermolytic toxin produced by Staphylococcus aureus causes a subcorneal blister. Invasion of epidermal cells by herpesvirus causes degenerative changes and intraepidermal vesicles. Intercellular edema caused by contact dermatitis results in stretching of the intercellular bridges (spongiosis) until they burst, forming intraepidermal vesicles. Dissolution of the intercellular adhesion molecules secondary to autoantibodies in pemphigus vulgaris causes loss of epidermal cohesion (acantholysis) and blisters within the epidermis.
| Disease | Frequency a | Etiology | History | Physical Examination | Differential Diagnosis | Laboratory Test |
|---|---|---|---|---|---|---|
| Bullous impetigo | 0.1 | Staphylococcus aureus | Pruritus | Circular yellow crusts, purulent bullae Head, neck, extremities | Contact dermatitis Herpes simplex Superficial fungus Pemphigus vulgaris Staphylococcal scalded skin syndrome | Gram-stain Culture |
| Contact dermatitis | 2.8 | Allergen Irritant | Irritant: exposure occurs hours to days before rash Allergic: exposure occurs 1–4 days before rash | Papulovesicles Conforms to area of contact with sharp margins Often has a geometric or linear configuration | Atopic dermatitis Bullous impetigo Herpes simplex Superficial fungal infection | Patch test |
| Herpes simplex | 1.5 | Herpes simplex virus | Itching or pain prodrome | Grouped vesicles Perioral and perineal location most frequent | Impetigo Superficial fungal infection Contact dermatitis | Tzanck smear Culture Immunofluorescent staining |
| Herpes zoster | 0.4 | Varicella-zoster virus | Itching or pain prodrome | Grouped vesicles Dermatomal distribution | Herpes simples in a dermatomal configuration | Tzanck smear Culture Immunofluorescent staining |
| Varicella | < 0.1 | Varicella-zoster virus | Marked pruritus | Macules, papules, vesicles, pustules Generalized | Rickettsialpox Smallpox Disseminated herpes simplex and herpes zoster Coxsackievirus, echovirus Monkeypox | Tzanck smear Culture Immunofluorescent staining |
a Percentage of new dermatology patients with this diagnosis seen in the Hershey Medical Center Dermatology Clinic, Hershey, PA.
Damage to the structures within the basement membrane zone causes loss of coherence between basal cells and dermis. These subepidermal bullae are characteristic of bullous pemphigoid, dermatitis herpetiformis, and porphyria cutanea tarda.
Blisters usually rupture, producing crusting and weeping. If they become filled with purulent material, they are called pustules .
Bullous Impetigo
- 1.
Fragile, clear or cloudy bullae
- 2.
S. aureus toxin causes the blister
- 3.
Treat with penicillinase-resistant antibiotic
Definition and Etiology
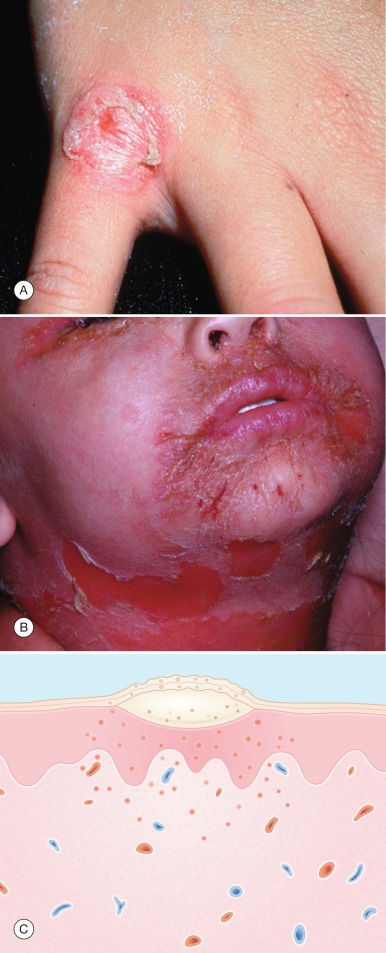
Bullous impetigo is an intraepidermal (subcorneal) bacterial infection of the skin caused by certain strains of S. aureus ( Fig. 10.1 ). Impetigo is also discussed in Chapter 12 .
Incidence
Bullous impetigo occurs most frequently in preschool- age children.
History
Crowding, poor hygiene, chronic dermatitis, and neglected injury of the skin are predisposing factors in the development of impetigo. An initial site of involvement is followed by multiple sites that may be pruritic.
Physical Examination
Fragile, clear or cloudy bullae ( Fig. 10.1A ) are characteristic of bullous impetigo. A thin, varnish-like crust occurs after rupture of the bulla. A delicate, collarette-like remnant of the blister roof is often present at the rim of the crust. Gyrate 0.05- to 2-cm crusted patches may be formed with clear centers and active margins. Autoinoculation results in satellite lesions. The face, neck, and extremities are most often affected. Regional adenopathy may be present, but patients have no systemic symptoms.
Differential Diagnosis
Contact dermatitis , herpes simplex virus (HSV) infection , and occasionally superficial fungal infections (see Fig. 9.8B ) may produce vesiculobullous or crusted lesions similar to those of impetigo. The history, patch tests, Tzanck and potassium hydroxide (KOH) preparations, and appropriate cultures differentiate these entities. Pemphigus vulgaris may also produce crusted lesions and should be suspected in patients with chronic, apparently impetiginized, patches that have not responded to appropriate antibiotics.
Staphylococcal scalded skin syndrome ( Fig. 10.1B ) is an uncommon disorder affecting primarily infants and young children. It is characterized by the sudden onset of fever, skin tenderness, and erythema, followed by the formation of large, flaccid bullae and shedding of large sheets of skin, leaving a denuded, scalded-appearing surface. In contrast to bullous impetigo, in which S. aureus may be recovered, the bullae of staphylococcal scalded skin syndrome are sterile. The usual source of infection is in the conjunctiva, nose, or pharynx. In the newborn, an infected umbilical stump may be the source.
- ●
Contact dermatitis
- ●
Herpes simplex
- ●
Superficial fungal infection
- ●
Pemphigus vulgaris
- ●
Staphylococcal scalded skin syndrome
Laboratory and Biopsy
Gram-staining of the clear or cloudy fluid from a bulla reveals gram-positive cocci. S. aureus grows out in more than 95% of the cultures. Biopsy of impetigo, which is usually not done because the diagnosis is obvious, reveals a subcorneal pustule or blister ( Fig. 10.1C ).
Therapy
Most S. aureus cultured from impetigo lesions is penicillin resistant. Therefore, a cephalosporin such as cephalexin, or penicillinase-resistant semisynthetic penicillin such as dicloxacillin should be chosen. Triple antibiotic, retapamulin, or mupirocin ointment applied three times daily is as effective as oral antibiotics in treating impetigo that is limited to a small area. For community-acquired methicillin-resistant S. aureus (MRSA), trimethoprim-sulfamethoxazole or doxycycline can be used as alternative treatments.
General hygiene should also be implemented to prevent spread. Cleansing with an antibacterial cleanser and gentle removal of crust hasten healing. Daily changing of items that contact the area of impetigo such as towels, washcloths, and shavers is recommended. For widespread or recurrent impetigo, bleach baths can be helpful.
Initial
Antibiotics
- ●
Cephalexin: 25–50 mg/kg daily in oral suspension, 500 mg b.i.d.
- ●
Dicloxacillin: 500 mg b.i.d.
- ●
Triple antibiotic, mupirocin, or retapamulin ointment applied b.i.d. or t.i.d.
General Hygiene
- ●
Antibacterial soap: chlorhexidine gluconate
- ●
Changing of towel, washcloth, shaver, etc., daily
- ●
Bleach baths: ¼–½ cup of bleach in ½ tub of water daily
Alternative – for Methicillin-Resistant S. Aureus (MRSA)
- ●
Trimethoprim-sulfamethoxazole one double strength table b.i.d. or 4–6 mg/kg b.i.d.
- ●
Doxycycline 100 mg b.i.d.
Course and Complications
Even without treatment, impetigo heals spontaneously in 3 to 6 weeks. Antibiotics hasten healing (within 1 week of starting therapy) and reduce contagiousness.
Pathogenesis
An epidermolytic toxin targeting desmoglein 1, a desmosomal adhesion molecule, causes the subcorneal cleavage characteristic of bullous impetigo and staphylococcal scalded skin syndrome. This toxin is from pathogenic phage group II S. aureus . In bullous impetigo, the toxin is produced at the site of the lesion. In staphylococcal scalded skin syndrome, it is produced remotely and then carried hematogenously to the skin.
Epidermolytic toxin causes bullae.
Contact Dermatitis (Acute)
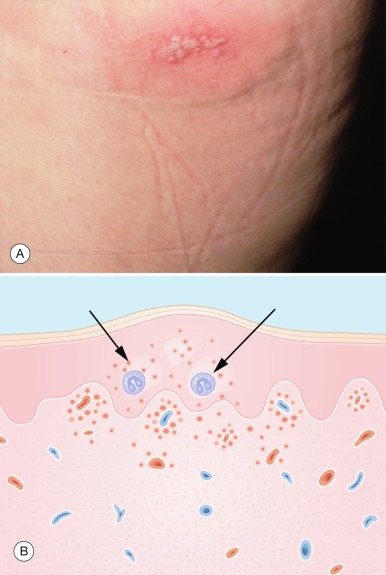
Because acute contact dermatitis is characterized by a vesicular eruption ( Fig. 10.2A ), it is mentioned briefly here. In Chapter 8 , it is discussed in more detail, along with other eczematous eruptions.

Contact dermatitis is an inflammatory reaction of the skin caused by an irritant or allergenic chemical. It may be an acute or chronic process. Intraepidermal vesicles are the hallmark of acute contact dermatitis. Additional characteristics are weeping, crusting, edema, and erythema. The areas involved frequently have sharp margins with geometric and linear configurations. Poison ivy and other plants characteristically cause linear streaks of papulovesicles. Treatment is with steroids (topical or systemic), antihistamines, and wet dressings or soaks. The biopsy of acute contact dermatitis reveals spongiosis and intraepidermal vesicle formation with inflammation ( Fig. 10.2B ).
Herpes Simplex
- 1.
Recurrent grouped vesicles in the same location
- 2.
Tzanck smear is diagnostic
- 3.
Treatment is suppressive, not curative
Definition
Herpes simplex is an acute, self-limiting, intraepidermal vesicular eruption caused by infection with herpes simplex virus (HSV) ( Fig. 10.3 ). HSV is a DNA virus that replicates within the nucleus. Based on culture and immunologic characteristics, it is divided into two types: HSV-1 and HSV-2. Usually, HSV-1 causes oral infection and HSV-2 causes genital infection. Primary infections with these viruses are characteristically followed by recurrent attacks.
Incidence
Infection with HSV is common worldwide. It is estimated that in the United States more than 50% of adults are seropositive for HSV-1 and more than 20% for HSV-2.
History
Primary infection with HSV-1 usually occurs in children, in whom it is subclinical in 90% of cases. The remaining 10% of infected children have acute gingivostomatitis. In contrast, HSV-2 primary infection usually occurs after sexual contact in postpubertal individuals, and it produces acute vulvovaginitis or progenitalis. Primary infections are frequently accompanied by systemic symptoms that include fever, malaise, myalgia, headache, and regional adenopathy. Localized pain and burning may be so severe that drinking and eating, or urinating, may be compromised.
Infection of the lips (herpes labialis) is usually caused by HSV-1, whereas the genitals and buttocks are more often infected with HSV-2. The risk of a woman developing genital herpes on exposure to an infected man is estimated to be 80% to 90%. The risk of recurrence after primary genital infections is less with HSV-1 (14%) than with HSV-2 (60%). Recurrent attacks are preceded by localized itching or burning and are characterized by occurrence in the same location. This prodrome usually begins within 24 hours before the appearance of the eruption and occurs in approximately two-thirds of patients.
Herpes should be suspected if a vesicular eruption is:
- 1.
Recurrent in same location
- 2.
Preceded by a prodrome
HSV infections are not limited to the lips and genital area; either type can infect any area of skin. Therefore, a history of a vesicular eruption recurring in the same location should lead to a suspicion of HSV infection.
Physical Examination
Indurated erythema followed by grouped vesicles on an erythematous base is typical of herpes infections. The vesicles quickly become pustules, which rupture, weep, and crust. Affected skin sometimes becomes necrotic, resulting in punched-out ulceration.
Grouped vesicles on an erythematous base are characteristic of HSV infection.
Primary infections – gingivostomatitis or vulvovaginitis – are characterized by extensive vesiculation of the mucous membranes. This results in erosions, necrosis, and a marked purulent discharge. Herpes infection can develop in any area where inoculation has occurred. Recurrent herpes infections are characterized by localized grouped vesicles in the same location. Herpetic whitlow is infection of the fingers. This is an occupational hazard of medical and dental personnel that can be prevented by wearing gloves. Traumatic herpes simplex has been reported in epidemics among wrestlers (herpes gladiatorum). Eczema herpeticum is a generalized cutaneous infection with HSV in individuals with predisposing skin diseases such as atopic dermatitis. It is accompanied by severe toxic symptoms and may be fatal.
Differential Diagnosis
Impetigo , contact dermatitis , and, less often, superficial fungal infections may be confused with herpes simplex and can be ruled out by the history, Gram-staining and culture of the blister fluid, patch testing with suspected allergens, and KOH preparation test of the blister roof.
- ●
Impetigo
- ●
Contact dermatitis
- ●
Superficial fungal infection
Laboratory and Biopsy
The occurrence of grouped vesicles on an erythematous base is characteristic of HSV infection. It can be confirmed with a Tzanck smear, which reveals multinucleated giant cells ( Fig. 10.4 ). The Tzanck smear is a simple yet reliable method of confirming a herpetic infection. Smears from the base of the lesion stained with Giemsa, Wright, or toluidine blue demonstrate multinucleated giant cells diagnostic of HSV infection. A detailed description of preparing a Tzanck preparation is presented in Chapter 3 . The positivity of the Tzanck preparation varies with the lesion sampled: vesicle, 67%; pustule, 55%; and crust-ulcer, 16.7%. A high correlation exists between the Tzanck preparation and viral culture. However, when performed properly, the culture has a greater positivity: vesicle, 100%; pustule, 73%; and crust-ulcer, 33%. Direct immunofluorescent staining of vesicle smears compares favorably with viral cultures. Although usually not necessary, the biopsy ( Fig. 10.3B ) reveals an intraepidermal blister with multinucleated epidermal giant cells and an acute inflammatory process. Patients with genital herpes should be screened for other sexually transmitted diseases.
Tzanck smear revealing multinucleated giant cells confirms a herpetic infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








