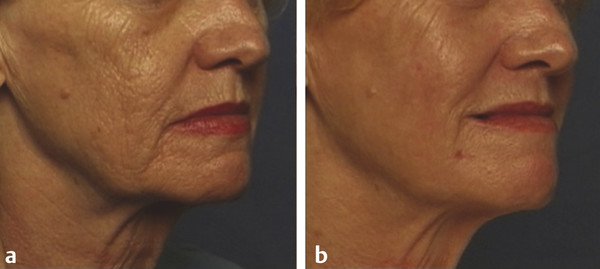
Introduction Acne vulgaris is one of the most common skin conditions in adolescents and adults, and has been reported to affect up to 80% of individuals between the ages of 11 and 30. The causes of acne vulgaris include: hormonal changes, increased sebum production, Propionibacterium acnes activity, follicular hyperkeratinization, and perifollicular inflammation. The incidence of acne scarring in the general population has been reported between 1 and 30%.1,2 Acne scarring is a consequence of abnormal wound healing due to damage in the pilosebaceous follicle during inflammation. Recent studies suggest that a patient’s risk of scarring correlates with the type and magnitude of the inflammatory response in acne lesions. Cell-mediated immune responses aid in clearance of an antigen but also contribute to the amount of tissue damage. Studies by Holland et al3 and Holland and Jeremy4 used immunohistochemical methods to determine the cell-mediated response in developing and resolving inflamed acne lesions. Patients prone to acne scarring have an ineffective early inflammatory response followed by a later increased inflammatory response with greater cellular activation and domination by an influx of macrophages. Acne scars vary in their clinical presentations with a wide range of both pigment and textural alterations in the skin. However, the psychosocial impact of an acne scar cannot be underestimated. Acne scarring can be very distressing to patients and can result in a decreased self-esteem and a diminished quality of life.5 It is important to note that the degree of an individual’s psychosocial distress associated with acne scarring may not correlate with the amount of acne scarring present on examination. Acne scars can be differentiated by color and textural changes in the skin. Postinflammatory erythema may be a resolving acne lesion’s initial presentation. Brown shades of postinflammatory hyperpigmentation may lighten and improve with time, whereas hypopigmentation represents the final result of the scarring process. Textural skin changes can be categorized as hypertrophic or atrophic. Hypertrophic scars are confined within the margins of the original injury. They are raised, firm nodular lesions. Keloids resemble hypertrophic scars but are characterized by a disproportionate deposition of collagen with an excess amount outside of the original injury margins. Hypertrophic and keloid scars are a result of excessive collagen deposition at the site of the skin injury where fibrosis has elevated the skin surface focally. In contrast, loss or damage of soft tissue is referred to as an atrophic scar. These acne scars result from collagen destruction in the dermis and soft tissue atrophy. Scar contraction results in the indentation of the skin. Atrophic acne scars are often erythematous initially and can become hypopigmented or hyperpigmented with time. In 2001, Jacob et al proposed a classification of atrophic acne scars into three types: ice-pick, rolling, and boxcar scars. Ice-pick scars are narrow (less than 2 mm), V-shaped epithelial tracts that extend deep into the dermis. Rolling scars are wider (4–5 mm) and are tethered to the subcutaneous tissue, resulting in an undulating appearance. Boxcar scars are sharply delineated round or oval depressions that can be shallow or deep and range in diameters of 1.5–4 mm.6 Atrophic acne scarring is by far the most common form of acne scarring, especially on the face.7 Goodman and Baron proposed a new qualitative grading system for acne scarring with suggested therapies for each scar type (▶ Table 17.1 and ▶ Table 17.2). This grading system has four levels of acne scarring: (1) macular, (2) mild, (3) moderate, and (4) severe. The subdivisions for level 1, macular disease, include erythematous, hypopigmented or hyperpigmented. Grades 2 to 4, mild to severe disease, are classified as being atrophic or hypertrophic. Grade 3, moderate, acne scars can be flattened by manually stretching the skin, and include rolling or shallow boxcar scars. Grade 4 scars are not distensible and include ice-pick, deep boxcar, and significant hypertrophic and keloid acne scars.8 The lack of a true consensus on a grading scale for acne scarring may limit the ability to clinically standardize the therapeutic approach to acne scars.9 Grade Level of disease Characteristics 1 Macular Erythematous, hyperpigmented or hypopigmented flat marks visible to patient or observer at any distance 2 Mild Mild atrophy or hypertrophy that may not be obvious at social distances of 50 cm or more, and may be covered adequately by makeup or the normal shadow of shaved beard hair in men or normal body hair if extrafacial 3 Moderate Moderate atrophic or hypertrophic scarring that is obvious at social distances of 50 cm or more, and is not covered easily by makeup or the normal shadow of shaved beard hair in men or body hair if extrafacial, but is still able to be flattened by manual stretching of the skin (if atrophic) 4 Severe Severe atrophic or hypertrophic scarring that is obvious at social distances greater than 50 cm, and is not covered easily by makeup or the normal shadow of shaved beard hair in men or body hair if extrafacial and is not able to be flattened by manual stretching of the skin (Reproduced with permission from Goodman GJ, Baron JA. The management of postacne scarring. Dermatol Surg 2007; 33: 1175–1188.) Grade Level of disease Examples of scars 1 Macular Erythematous, hyperpigmented, or hypopigmented flat marks 2 Mild Mild rolling, small soft papular 3 Moderate More significant rolling, shallow boxcar, mild to moderate hypertrophic or papular scars 4 Severe Punched-out atrophic (deep boxcar), ice-pick, bridges and tunnels, marked atrophy, dystrophic significant hypertrophy or keloid (Reproduced with permission from Goodman GJ, Baron JA. The management of postacne scarring. Dermatol Surg 2007; 33: 1175–1188.) Prevention of acne scarring is best achieved through early treatment of active acne. However, once a patient has acne scarring the treatment should be individualized to meet the needs of the patient. It is important to establish realistic expectations for patients. Patient education regarding the nature of acne scarring and the inability to remove the scar is imperative in the preoperative evaluation and consultation. Treatment for acne scars can be divided into medical, procedural, and surgical options. Typically, a wide variety of acne scars can exist in each individual patient, necessitating knowledge of the range of treatment modalities available. Topical retinoids are recommended as part of a combination treatment for inflammatory acne disease. Topical retinoids stimulate collagen formation, increase dermal collagen synthesis, and improve elastic fibers.10,11 Use of a 0.05% topical tretinoin for 4 months was reported to improve the appearance of facial ice-pick scars.12 Topical treatments including retinoic acid, hydroquinone, azelaic acid, and kojic acid are effective in decreasing postinflammatory hyperpigmentation.13,14 Tretinoin causes epidermal thickening, compaction of the stratum corneum, increased granular thickness, increased collagen synthesis, and decreased melanin content, which results in a decrease of postinflammatory hyperpigmentation and improved appearance of facial rhytids and scars. Options for treatment of hypertrophic and keloid scars include the glucocorticoids (triamcinolone, hydrocortisone, methyl prednisone, and dexamethasone). The glucocorticoids have anti-inflammatory properties and inhibit fibroblast growth while degrading collagen. Serial intralesional injections spaced 4 to 6 weeks apart can result in flattening and softening of hypertrophic and keloid scars. Injection of cystic, inflammatory acne lesions with steroids may help prevent scarring by decreasing the inflammatory response.15 Complications from excessive steroid injections include atrophy, hypopigmentation, and telangectasias.16 A pyrimidine analogue with antimetabolic activity, 5-fluorouracil (5-FU), has been shown to inhibit wound healing. This compound has an inhibitory effect on human fibroblast by inhibiting proliferation and myofibroblast differentiation. Fluorouracil is usually used at a concentration of 50 mg/mL with a total dose between 50 to 150 mg per session. Fluorouracil can be used alone or mixed at a ratio of 80:20 with a low-strength steroid.8 In a 2002 study by Gupta and Kalra, more than 50% of patients showed significant flattening of keloids as a result of intralesional injections with 5-FU.17 Additionally, Bleomycin has been shown to flatten hypertrophic scars by inhibiting collagen synthesis through its cytotoxic effects on dividing fibroblasts.18 Silicone gel sheeting is recommended as a safe and effective management option for keloid and hypertrophic scars.19 Several studies report that silicone gels and silicone sheets are equal in efficacy in improvement of scar redness, elevation, pain, and pruritus. Research suggests that the possible mechanism of action of silicone products is not only a result of occlusion but that the magnitude of the occlusion may be an important component in the mechanism of action of silicone. In addition, the decrease in transepidermal water loss and resulting increase in hydration from the occlusion provided by the silicone product may modulate the signaling cascade initiated by the epidermis that stimulates the collagen production by dermal fibroblasts. The use of silicone gels may be better accepted by patients than the silicone sheets due to the decreased visibility of the applied gel on the scar.20 Dermabrasion can be one of the most effective but operator-dependent therapies for acne scarring. It is most effective for rolling, undulating scars and superficial boxcar scars.21 Several dermabrasion devices exist using either a high-speed brush or diamond cylinder. Diamond fraises are available in varying degrees of coarseness and different shapes. Superficial dermabrasion eliminates the epidermis and a deeper treatment will cause an injury in the papillary dermis. Re-epithelialization occurs by migration of cells stemming from the adnexal structures including the hair follicles, sebaceous glands, and sweat glands. Active inflammatory acne lesions that are present must be treated first and resolved prior to the dermabrasion procedure. A complete re-epithelialization usually occurs within 7 to 10 days after dermabrasion. Postdermabrasion care may include leaving the area open or managing it with occlusive dressings. Complications from dermabrasion include hypertrophic scarring and keloid formation, dyschromia, and infection. Prophylactic treatment of patients with a known history of herpes simplex virus (HSV) and preoperative treatment with antibiotics are recommended. Eczema dermatitis has been reported in 10% of patients and can be treated with topical, intralesional, or systemic steroids.22 It is recommended that patients wait a minimum of 6 to 12 months after treatment of isotretinoin therapy before undergoing a dermabrasion treatment.6,7 Isotretinoin reduces the cellular activity of cutaneous adnexal appendages, which hinders the re-epithelialization after the dermabrasion procedure. Chemical peels differ in their depth of penetration into the skin. In general, patients are open to the option of chemical peels because they are relatively noninvasive; have little downtime; and can improve skin pigmentation, tone, and texture. Superficial peels include alpha hydroxy acids (glycolic, lactic, citric) or beta hydroxy acid (salicylic), Jessner’s Solution, modified Jessner’s Solution, resorcinol, and low-strength trichloracetic acid (TCA) (< 20%TCA). Light peels are used to treat the most superficial of acne scars and are beneficial for improving postinflammatory hyperpigmentation. TCA solutions of 30 to 40% are primarily considered medium-depth peels. These peels extend down to the papillary dermis. Following a TCA peel, the skin re-epithelializes during the next several days and dermal collagen remodeling may continue for the next several months. During this process there is an increase in the production of collagen, elastin, and glycosaminocans.23 Deep chemical peels are phenol or croton oil-based. Deep chemical peels using 50% or more TCA and phenol/croton oil-based peels can extend to the reticular dermis and may be more effective for deep atrophic scars; however, they do carry a higher risk for postprocedure dyschromia, milia, and secondary infection. Phenol peels also have an added risk of possible cardiotoxicity and require cardiopulmonary monitoring and intravenous (IV) hydration during the procedure.24 Chemical peels are typically performed to treat an entire face or an aesthetic unit. The use of TCA has been refined to only treat the atrophic acne scars, using the chemical reconstruction of skin scars (CROSS) method.25 This method is reported to improve clinical results with rapid healing times and lower complication rates.26 The CROSS technique uses focal application of a high concentration (65–100%) of TCA to produce frosting directly in the acne scars. Treatments are often repeated at 6-week intervals and patients can receive a total of six procedures. Histological examination of the treated acne scars revealed coagulative necrosis in the epidermis and necrosis of collagen in the papillary and reticular dermis. This resulted in increased collagen in the treated scars and increased collagen production and fragmentation of elastin fibers in the papillary dermis.27 Tissue augmentation using fillers is effective in treating patients with superficial atrophic scars such as undulating, rolling scars. The previously available injectable collagens have been replaced with products containing hyaluronic acid (HA), calcium hydroxylapatite, and poly-L-lactic acid. HA is a polysaccharide that occurs naturally in the body’s connective tissue, dermis, umbilical cord, hyaline cartilage, and synovial joint fluid. After the first HA filler was introduced in 2003, a variety of available HA products have become available that differ in their concentration, degree of cross-linking, particle sizes, and longevity.28 HA fillers may improve the appearance of atrophic acne scars alone or they can be combined with subcision. Disadvantages of using HA fillers include the need for frequent treatments, and HA fillers may only improve the appearance of mildly atrophic scars. Calcium hydroxylapatite, Food and Drug Administration (FDA) approved in 2006, is a semipermanent filler composed of synthetic bone with microspheres 25 to 45 µm in diameter in a carboxymethylcellulose gel vehicle. The calcium hydroxylapatite (Radiesse, Merz North America, Inc., Raleigh, North Carolina) is biodegradable and stimulates fibroblastic production of collagen. Calcium hydroxylapatite is often appropriate for improving the appearance of shallow, atrophic acne scars.29 Injectable poly-L-lactic acid (PLLA) (Galderma Pharma SA/Galderma SA, Lausanne, Switzerland) is a synthetic, long-lasting dermal filler initially approved in 2004 for the correction of facial lipoatrophy associated with treatment for human immunodeficiency virus (HIV) infections. PLLA is a synthetic polymer similar to absorbable suture material. It comes in a lyophilized form and requires reconstitution with sterile water for injection. PLLA stimulates collagen formation due to a foreign-body reaction. Treatment with PLLA may require several sessions over a 4- to 6-month period with lasting results of 24 months or longer. PLLA is used to restore facial volume and several clinical trials and case reports have documented improvement in atrophic facial acne scars.30,31 A recent study in 2013 found that the autologous fibroblast procedure was associated with a significantly greater treatment success than the vehicle control for grade 3 (▶ Table 17.1), atrophic, distensible facial acne scars. Autologous fibroblasts are cultured from postauricular, full-thickness, punch biopsies. The autologous fibroblasts were injected into the papillary dermal plane under the atrophic acne scars in three treatment sessions spaced approximately 2 weeks apart. Whereas the mechanism of action of the procedure is not well understood, the improvement in the scar appearance may be due to new collagen production and remodeling of preexisting extracellular matrix in the scarred tissue.32 Deep acne scarring can produce severe facial fat atrophy. During the aging process additional soft tissue loss can increase the appearance of the acne scarring and lipoatrophy. Fat augmentation is able to reproduce the youthful appearance of a fuller face by replacing the soft tissue volume. The success of fat grafting is technique-dependent and the treatment requires a second surgical site for harvesting the fat. Improvements and advancements in fat-grafting techniques are resulting in greater consistency and longevity of the procedures.33,34 Microneedling or rolling, also referred to as percutaneous collagen induction, utilizes 30-gauge needles introduced into the skin in multiple directions in a controlled fashion. The epidermal trauma heals with transepidermal migration and the dermal trauma heals with collagen remodeling. Skin needling triggers a cascade of growth factors that stimulate wound healing. Histological studies show an increase in collagen and elastin deposition at 6 months posttreatment and a normal stratum corneum; thickened epidermis and normal rete ridges at 12 months posttreatment are displayed.35,36 Microneedling or collagen induction therapy is an in-office procedure performed under local anesthetic. Several studies have suggested that it is best utilized for grades 2 and 3 atrophic rolling or shallow boxcar acne scarring with four to six treatment sessions spaced 4 to 6 weeks apart. An advantage of microneedling is that it can be used on all skin types with little downtime.37,38,39 Botulinum toxin type A can decrease the appearance of acne scars that are amplified with facial movement. This treatment option is limited but may be applicable for amelioration in the appearance of acne scars in the upper third of the face and the chin area.40 Several laser/light therapy options exist to correct the dyschromia of acne scars and to improve the appearance of atrophic acne scars with stimulation of collagen production and remodeling. These include intense pulsed light (IPL) lasers, Q-switched (QS) lasers, the microsecond pulsed neodymium:yttrium aluminum garnet (Nd:YAG) laser, erbium:yttrium aluminum garnet (Er:YAG) lasers, and erbium:yttrium scandium gallium garnet (Er:YSGG) lasers. Excimer lasers have a wavelength in the ultraviolet (UV) range (308 nm) and provide concentrated melanin stimulation to white scars. Treatment should be deemed unsuccessful if there is no improvement in the hypopigmentation after five to ten sessions of excimer laser therapy.41 IPL devices provide noncoherent light of multiple wavelengths ranging from 500 to 1,200 nm that are confined to narrow ranges by the use of filters. A series of IPL procedures spaced 3 to 4 weeks apart can treat several conditions, including reducing the superficial erythema in early acne scars and decreasing postinflammatory hyperpigmentation. IPL devices are able to treat large surface areas due to the larger spot sizes. The first report of a nonablative laser being used for erythematous facial acne scars was published in 1996.42 Average clinical improvement in the acne scars 6 weeks after one session with the 585-nm pulsed dye laser (PDL) was 67.5%. A series of treatments with the vascular-specific 585-nm PDL can significantly improve the appearance of erythematous hypertrophic scars by reducing the redness and by induction of dermal collagen remodeling without epidermal damage. PDLs can be used on all skin types. The most common adverse effect of treatment with a PDL is posttreatment purpura that can persist for several days. Other nonablative lasers used to treat atrophic scars are the 1,320-nm Nd:YAG, 1,450-nm diode, and the 1,064-nm Nd:YAG.43 A study by Tanzi and Alster demonstrated that the 1,320-nm Nd:YAG and the 1,450-nm diode lasers both offer safe and effective clinical improvement of mild to moderate atrophic facial scars. They reported that the maximum clinical improvement was seen 6 months after a series of nonablative laser treatments. However, a decrease of clinical results in a 12-month follow-up evaluation suggests that maintenance treatments may be warranted or needed to enhance or maintain the clinical improvement.44 Carbon dioxide (CO2) laser resurfacing and the Er:YAG laser are two ablative skin-resurfacing techniques used to treat acne scarring. The CO2 laser with a wavelength of 10,600 nm has as its target extracellular and intracellular water. CO2 laser resurfacing is useful for hypertrophic scars, boxcar scars, and rolling, undulating scars (▶ Fig. 17.1, ▶ Fig. 17.2, ▶ Fig. 17.3). The ER:YAG laser is a gentler ablative laser resurfacing as compared to the CO2 laser. The ER:YAG laser is 12 to 18 times more efficiently absorbed by water, leading to a more superficial penetration and less collateral damage with more rapid healing. The photothermal effect of ablative lasers accounts for the shrinkage of collagen and the neocollagenesis and collagen remodeling that leads to marked enhancement of skin-texture irregularity, skin tightening, and lifting. The goal of ablative laser treatments of atrophic scars is to reduce the depth of scar borders and stimulate neocollagenesis. The depth of ablation correlates with the number of passes performed. Treatment of entire cosmetic units has been recommended in order to avoid obvious lines of demarcation between treated and untreated sites. Isotretinoin use within the preceding 6- to 12-month period or a history of keloids is considered a contraindication to ablative laser treatment.45 Complications of ablative skin resurfacing include hypertrophic scarring, possible ectropion formation, infection, and dyschromia.46 Fig. 17.1 A 60-year-old woman before (a) and after (b) full ablative carbon dioxide (CO2) resurfacing of full face for aging skin and moderate acne scars.
17.2 Acne Scar Classification
17.3 Treatment Options for Acne Scars
17.3.1 Medical Options
17.3.2 Procedural Options
Treatment of Acne Scarring
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree