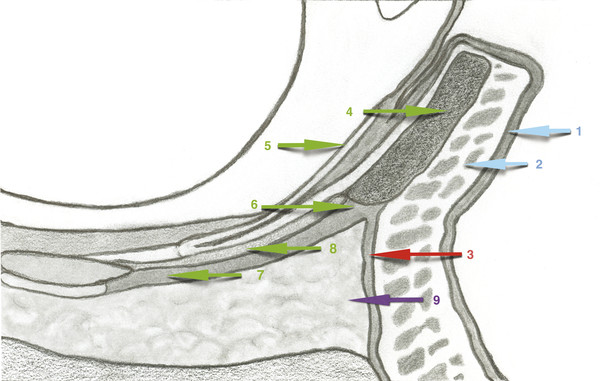
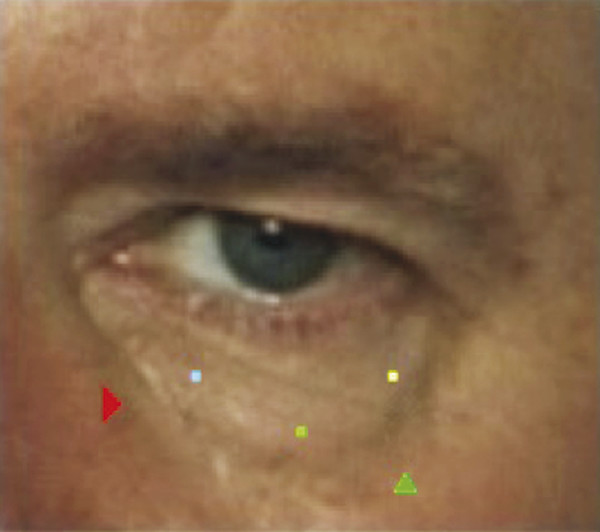
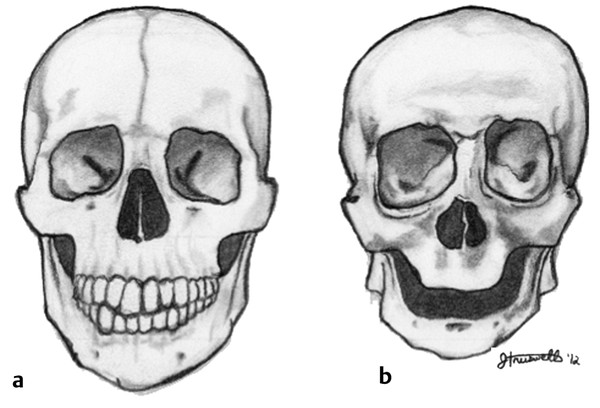
Poets have extoled the beauty of women’s eyes in countless ways and over all of time. When we first meet someone and when we converse we look into the person’s eyes. The eyes are the facial feature we spend the most time observing in human intercourse. Women spend millions of dollars each year on eyeshade, mascara, Latisse (Allergan, Inc., Irvine, California), brow waxing, neuromodulation, and surgery to make their eyes more attractive and alluring. When describing their perception of how they look, patients often use negative terms describing how their character or personality is projected vis-à-vis the appearance of their eyes. At the more youthful end of the aging spectrum, a patient will often complain of looking tired or unhappy. Whereas at the opposite end of this continuum, an older individual’s vision may be obscured by redundant upper lid skin, and laxity of the lower lid may cause ectropion with chronic inflammation and irritation.1 Patients, wishing to have a more youthful appearance of the lower eyelid, most often speak of “my bags,” wrinkles, and “dark circles.” The lower lid, with its own senescent changes to the surrounding anatomical structures of the midface, necessitates a broader discussion with the patient. In youth, the actual demarcation between the lower lid and cheek is blurred. As a person passes through the late 30s and early 40s the malar fat pad and suborbicularis oculi fat (SOOF) pad descend. This enhances the separation of lower lid and cheek and draws increased attention to aging changes in the lower lid.2,3 The goal of most patients is to have the “bags” reduced and the wrinkles softened. The procedure this author favors is a transconjunctival approach to the fat and fractional or ablative carbon dioxide (CO2) laser resurfacing of the eyelid skin. If needed, fat repositioning can be done at the same time. When the lid needs tightening, a concomitant “pinch” technique will gain access for canthoplasty, canthopexy, tarsal strip, or other lid-supporting techniques. The numerous techniques for lower lid surgery, midface elevation, and volume restoration are beyond the scope of this chapter. The focus of this chapter is on the application and rationale of using the CO2 laser in rejuvenation of the lower eyelid. All the ancillary procedures for lid tightening, midface lifting, and volume restoration can be done, if indicated, concomitantly. The lower eyelid extends from medial to lateral canthus and downward from its free upper edge to the orbital rim. There is a crease near the inferior border of the tarsal plate associated with fibers from the anterior layer of the capsulopalpebral fascia extending to the skin.4 The lower lid consists of three lamellae. The description of these lamellae is not universal in the literature; however, the concept is useful in surgical approaches to the lower eyelid. The anterior lamella is made up of the skin and orbicularis oculi muscle. The thinness of the skin of the lower eyelid is unmatched on the human body. The subcutaneous fat is meager and lies over the orbicularis oculi muscle. This muscle has three distinct parts, the pretarsal, palpebral or preseptal, and the orbital. Their points of origin are the inferomedial orbital rim, the frontal process of the maxilla, and the medial palpebral ligament.5,6,7 The medial canthal ligament attaches to the frontal process of the maxilla and the posterior lacrimal crest. The lateral canthal tendon attaches to the Whitnall tubercle. The tendons form thickened attachments to the tarsal plate, and together they support the eyelid (▶ Fig. 9.1).5,7 Fig. 9.1 Cross-sectional anatomy of the lower eyelid. Blue arrows are the outer lamella: 1, skin; 2, orbicularis oculi muscle. Red arrow is the middle lamella: 3, orbital septum. Green arrows are the inner lamella: 4, tarsal plate; 5, conjunctiva; 6, Lockwood ligament; 7, capsulopalpebral fascia; and 8, tarsal muscle. Purple arrow: 9, orbital fat. The middle lamella is the orbital septum. The orbital septum is a dense extension of the orbital periosteum arising at the arcus marginalis. The orbital septum retains the orbital fat. The fat is divided into three pads. The inferior oblique muscle lies between the medial and middle pads. The arcuate expansion of the Lockwood ligament delineates the middle fat pad from the lateral pad. This particular division usually becomes visible in the aging lower lid.5,6,8 The posterior lamella consists of the tarsus, the lid retractors, and the conjunctiva. The capsulopalpebral fascia of the inferior rectus muscle splits to encompass the inferior oblique muscle before reuniting and forming a dense band that joins with the orbital septum to become the Lockwood ligament. The Lockwood ligament inserts into the inferior edge of the tarsal plate. The lid retractors are composed of the capsulopalpebral fascia and the tarsal muscle. On the surface of the lower lid conjunctiva is a vertical array of blood vessels. The complex anatomical components of the lower eyelid age at different times and different rates. Like the entirety of the aging face, the lower lid will mature basically in three separate ways. The first to age is the skin, followed by laxity and loosening of structures, and volume loss of the tissues. When one is a teenager and is in the 20s and early-to-mid 30s, the skin shows that “glow of youth.” It is smooth without rhytids, discoloration, and visible pores. The keratinocytes form at the basement membrane and rise upward forming the various dermal layers and the epidermis until they become the stratum corneum, cells without nuclei and organelles. At this point washing the face sheds them. In youth, washing cleans the lost cells away.9 As age moves one into the later 30s and beyond, this layer becomes more adherent and the glow of youth surrenders to the flat and dull look of maturity. Extrinsic factors influence the rate and degree of aging skin. Sun exposure and tobacco use notoriously damage the skin. With time, the architecture of the dermis and epidermis alters. The skin becomes dry and flakey as the vascular supply diminishes and the tissue dehydrates. The epidermis no longer adheres firmly to the dermis with attenuation of the rete ridges. The various dermal glands and hair follicles lessen in number. Rhytids appear and deepen and elongate.9,10 Photodamage lends greatly to the appearance of lesions such as lentigines, actinic keratoses, seborrheic keratoses, and skin cancers. ▶ Fig. 9.2a shows a 60-year-old woman before surgery. ▶ Fig. 9.2b is a computer-generated depiction of a Wood lamp view of her face. This highlights the photodamage and marked rhytids of her face. ▶ Fig. 9.2c, d are the postoperative pictures of the same woman after undergoing an endoscopic forehead lift, upper and laser-assisted lower eyelid blepharoplasty, facelift, and full face and neck fractional laser resurfacing including the eyelids. Note the marked rejuvenation of her skin with considerable softening of her rhytids and improvement of her photodamage secondary to the laser resurfacing. A lifetime of smiling coupled with thinning periocular skin produces visible “crow’s-feet.” These are seen at first in the younger patient only with a smile. As time advances and aging changes accelerate, these rhytids remain visible at rest. Fig. 9.2 (a) A 60-year-old woman before surgery. (b) Patient in a computer-generated Wood lamp depiction demonstrating the marked rhytidosis and photodamage of her skin. (c, d) Patient after an endoscopic forehead lift, upper and laser-assisted lower eyelid blepharoplasty, facelift, and full face and neck carbon dioxide (CO2) laser fractional resurfacing. (Reproduced with permission from Truswell WH, IV. Combining fractional carbon-dioxide laser resurfacing with face-lift surgery. Facial Plast Surg Clin North Am 2012; 20: 201–213, vi.) The relation of the lower eyelid to the midface testifies to the youth or senescence of the face. In the young face, the skin descends from the lower edge of the tarsus in one smooth curve, a single convexity, to the mandible. This curve also extends smoothly from the nose, nasolabial fold, and corner of the mouth laterally across the cheek. The integrity of the lid structures is firm and supportive of lid position. Many events occur with aging in all the associated anatomical structures and contribute to the evolution of an older eye. Alterations in the appearance of the lower lid become evident about the start of the 5th decade of life. The orbital structures weaken and attenuate leading to descent of the globe within the orbit.5,11 This pushes the inferior orbital fat against the weakening orbital septum. The laxity of the orbital septum, the attenuation of the orbicularis oculi muscle, and the downward pressure of the globe force the fat pockets to move forward as a pseudoherniation and create the lower lid “bags.” The orbital septum is firmly attached to the orbital rim at the arcus marginalis. This prevents the lid structures from descending below the orbital rim.12 As the intrinsic changes of the lid occur, the malar fat pad and the suborbicularis oculi fat pad descend and pull away from the rim, which becomes skeletonized. Thus the single convexity of youth morphs into the double convexity of age. A depression is seen along the orbital rim between the pseudoherniated orbital fat and the lowering malar fat pad and SOOF, and the nasojugal groove or tear trough deformity develops. As the midface descent progresses and the lid structures continue to weaken, there is elongation of the lower eyelid. With time, senile ectropion may develop with all its attendant consequences of dry eye, chronic inflammation, and meibomian gland dysfunction (▶ Fig. 9.3).2,3,5,13 Fig. 9.3 The aging eye. Note: rhytids, photodamaged skin, eyebrow ptosis, upper eyelid dermatochalasis and hooding, laxity and rounding of the lower eyelid, elongation of the lower eyelid, nasojugal groove (red arrowhead), and skeletonization of the orbital rim (green arrowhead). There is also pseudoherniation of the medial, middle, and lateral fat pads (blue, green, and yellow dots, respectively). The aging changes occurring in the lower eyelid and periorbita and the descent of the malar and SOOF fat pads are further exacerbated by the alteration of the facial skeletal structure. As the soft tissues of the midface lower, volume is lost in the muscles, fat, and bone. The mature adult facial skeleton has a balance among the horizontal thirds of the face. As the face transitions to one of old age, the bony changes in the orbits manifest as an enlargement of the circle of the rims, and a lateral downward teardrop appearance occurs. This creates a more infantile shape where the upper third dominates the shape of the face and head (▶ Fig. 9.4).9,13 The eyes appear sunken. Fig. 9.4 The transition from the (a) adult to the (b) senescent facial skeleton. (Reproduced with permission from Truswell WH, IV. Aging changes of the periorbita, cheeks, and midface. Facial Plast Surg 2013; 29: 3–12.) Proper patient selection for lower eyelid blepharoplasty will be accomplished by conducting a complete and systematic consultation. As in all things medical, a total, detailed history is taken. The first things to be established are: Why is the patient seeking lower eyelid surgery? Are the patient’s expectations realistic? This process involves a give-and-take between surgeon and patient. An ophthalmic history is taken along with general medical queries. The doctor must also educate the patient on the findings of the eye examination, on what can be accomplished and how it will be done, on what the patient should expect the outcome to be, on the preoperative and postoperative course, and on the likely sequelae and possible complications of the procedure. It is essential to note the general health of the patient, what prescriptive and over-the-counter medicines and supplements are taken, and what surgeries the patient may have had. Note if there is a bleeding or easy-bruising tendency. It is important to include history of alcohol and tobacco use. Record when the last ophthalmic examination was done, what the patient’s vision is, and if there is a history of dry eye. The surgeon should ask the patient about itchy eyes or a sensation of something in the eye. Are over-the-counter eye drops used? Positive responses would suggest a developing dry eye syndrome and may warrant an ophthalmology consultation. Record the presence or absence of glaucoma, cataracts, recurring conjunctivitis, previous ophthalmic surgery, or trauma.1,5 It is also important to find out a history of skin disorders that could affect healing of lasered skin. Contraindications to resurfacing include skin diseases like scleroderma, sarcoidosis, psoriasis, eczema, irradiated skin, vitiligo, and a history of keloid or hypertrophic scarring. Is there a history of previous resurfacing of the skin? What cosmeceuticals does the patient use? Has the patient been on isotretinoin, which delays healing?10,14 The physical examination focuses on the structures to be addressed and the face as a whole. The Fitzpatrick or Glogau skin type, the amount of photodamage, and the degree of rhytids should be recorded. Determine the state of hydration. It is important to recognize telangiectasias and the presence of rosacea. Ascertain if there are any skin lesions such as lentigines, actinic keratoses, seborrheic keratoses, basal cell carcinomas, squamous cell carcinomas, and suspicious nevi. Determine how much asymmetry of the face is present and point it out to the patient. Pay particular attention to asymmetries of the periorbita and be certain the patient acknowledges them. The eye examination is done with the head and gaze in the neutral position. The lower lid margin will sit just touching the lower limbus. If the white of the sclera can be seen, it indicates possible lid laxity. Checking for lid laxity is done with the snap back test and the retraction test. To perform the snap back test (▶ Fig. 9.5), the lower lid is drawn gently forward from the globe and released. If it drifts back slowly it is an indicator of laxity. The lid retraction test (▶ Fig. 9.6) is done by drawing the lower lid downward. The test is positive if the puncta can be retracted more than 3mm beyond the medial canthus. If so, a medial canthopexy may be necessary. If both or either of these tests is positive, the surgeon must consider performing a horizontal lid tightening procedure at the time of surgery. The integrity of the medial and lateral tendons is also determined. The medial canthal tendon is drawn laterally and released and the lateral canthus is, likewise, drawn medially and released. If either is easily pulled or stretched, a canthal tendon tuck procedure may be indicated.15 If lid laxity goes unrecognized and addressed, it can lead to scleral show or ectropion. Fig. 9.5 The snap back test.
9.2 Anatomy of the Lower Eyelid
9.3 How the Lower Eyelid Ages

9.4 Clinical Assessment

Laser-Assisted Lower Lid Blepharoplasty
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








