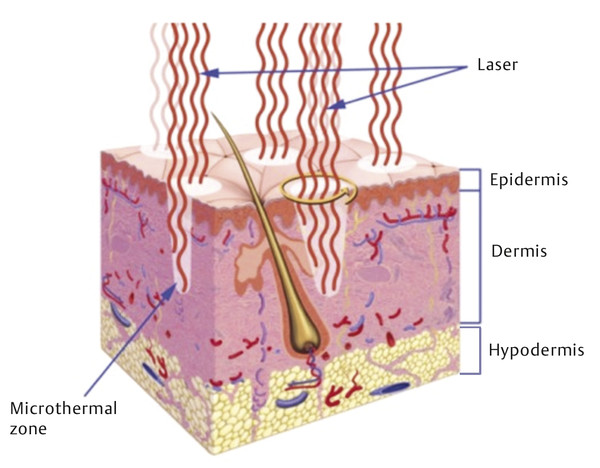
Skin types and colors are divided into six phototypes, Fitzpatrick skin types I through VI, with I being the fairest, and VI being the darkest (▶ Table 5.1).2 Within a single ethnicity, there may be variable phototypes and it is important to tailor the treatment to the patient. The number of melanocytes is consistent throughout all ethnicities. Melanocytes derive from neural crest cells and transfer melanosomes, which contain melanin, into keratinocytes. Melanin functions to protect the skin from ultraviolet radiation. The color of skin is dependent on the density, size, and activity of melanosomes because darker skin has a higher density of larger melanosomes.3 In addition, darker skin types, Fitzpatrick V and VI, have thicker and more compact skin layers with thicker collagen bundles, which increase the epidermal barrier and reduce skin sensitivity (▶ Fig. 32.1).4,5 This barrier delays skin damage from the environment and ultraviolet radiation and aging in darker phototypes when compared to lighter skin types. Due to these histological differences, darker skin is at increased risk for injury due to incidental laser absorption by melanin, problems with postinflammatory hyperpigmentation, and decrease of melanin production leading to hypopigmentation. Fig. 32.1 Layers of the skin. The skin is divided into the epidermis, dermis, and hypodermis. Darker skinned individuals have increased density of larger melanocytes, more compact skin layers, and thicker collagen bundles. Although there are many of types of lasers, the fundamental principle is the same: All lasers treat the skin by targeting a specific chromophore. A chromophore is an endogenous molecule that has a unique absorption spectrum and peak absorption wavelength. The main chromophores of the skin are hemoglobin, melanin, and water. In general, resurfacing lasers are designed at specific wavelengths that use water as a chromophore to cause targeted thermal damage in the dermis in order to promote new collagen formation and skin tightening.6 Other targetable chromophores include melanin, which has a broad, but gradually decreasing, absorption coefficient from 250 to 1,200 nm. The selection of a laser with a longer wavelength can allow for targeting of deep melanin or tattoo pigmentation in darker skin types.5 Other variables important to lasers include the thermal relaxation time, pulse duration, and energy fluence (▶ Table 32.1). The thermal relaxation time is the time required for a tissue to cool to one half the temperature to which it was heated. Heating the tissue for time longer than the thermal relaxation time can cause thermal damage to surrounding tissue. In darker skinned individuals, it is important to select a pulse duration longer than the thermal relaxation time of the epidermis but shorter than the target chromophore in order to avoid epidermal blistering, crusting, pigmentation changes, and scarring.5 The fluence is the joules per square centimeter (J/cm2) of energy emitted from the laser handpiece. The laser fluence may need to be decreased to protect the epidermis in order to safely treat a patient with darker compared to lighter skin types. Other helpful strategies in safely treating patients of color include longer wavelengths; longer pulse durations; and skin cooling before, during, and/or after the procedure to avoid overheating the epidermis.5,7 Variable Function Example Chromophore Laser target molecule, unique absorption spectrum and peak absorption wavelength Hemoglobin, melanin, water Wavelength Property of light measured in nanometers (nm) that influences how chromophores are targeted Hemoglobin (variable absorption from 300 nm–infrared) Melanin (gradually decreasing absorption from 250–1,200 nm) Water (1,000 nm–1 mm) Thermal relaxation time Time required for tissue to cool to one half the temperature to which it was heated Melanosome (250 ns) Vessels (2–10 ms) Hair follicles (100 ms) Pulse duration Time to heat tissue to target tissue; choose pulse duration less than or equal to thermal relaxation time of target chromophore to avoid damage to surrounding tissue Pulse duration 10–100 ns to target melanosome Energy fluence Joules per square centimeter (J/cm2) of energy emitted by a pulsed laser device 25 J/cm2 used by a 1,064-nm Nd:YAG for laser hair removal; highest tolerated fluences are 100 J/cm2 (IV, V)* and 50 J/cm2 (VI)3 Abbreviations: ms, milliseconds; Nd:YAG laser, neodymium:yttrium aluminum garnet laser; ns, nanoseconds. Note: Lasers perform differently based on variable characteristics, and the understanding of these variables may facilitate the selection of a laser for a specific treatment goal. *Italic type in parentheses denotes Fitzpatrick skin types. Lasers may be considered for a variety of indications and the goals of the treatment should reflect the patient presentation. There is an increased desire in all patients to achieve more youthful and refreshed facial skin. Over time, facial skin experiences photodamage, soft-tissue volume loss, rhytids, abnormal pigmentation, and irregular textures. The primary environmental factor that affects aging is ultraviolet radiation; however, given the protective effects of melanin and a thicker epidermis, individuals with darker skin may experience less skin laxity due to gravity and volume loss compared to others with fair skin.5 The primary concerns of patients may vary depending on ethnicity and skin type. Hispanic patients commonly present with complaints of acne vulgaris, eczema, contact dermatitis, photoaging, facial melasma, and hyperpigmentation.5,8 African American patients frequently complain of acne vulgaris, dyschromia (▶ Fig. 32.2), contact dermatitis, alopecia, and seborrhea dermatitis.3,8 And Asian patients often present with pigmentary disorders, facial melasma, freckles, lentigines, Ota-like macules, acne vulgaris, and hypertrophic scarring.4,8 Dyschromia is a common presentation of darker skinned patients and it is important to distinguish between melasma and postinflammatory hyperpigmentation when considering laser therapy.4,7,8,9,10 Options for laser treatment of dyschromia include the neodymium:yttrium aluminum garnet (Nd:YAG; CoolTouch, ICN Pharmaceuticals, Costa Mesa, California) laser and fractional nonablative devices.9 Fig. 32.2 Dyschromia. This alteration of the color of the skin may present as hyperpigmentation or hypopigmentation and is one of the most common treatment goals of laser therapy in ethnic populations. The use of lasers for hair removal (▶ Fig. 32.3) relies on melanin absorption within the hair follicle. Laser hair removal may be complicated in patients with darker skin due to disruption of melanin and subsequent risk for hypopigmentation at the site of hair removal.5 With this in mind, longer wavelength lasers (1,064-nm Nd:YAG; ICN) with lower fluences and postprocedural cooling may be used successfully in darker skin types for the treatment of hypertrichosis.3 When choosing a laser for hair removal, the 1,064-nm Nd:YAG is the safest choice in darker skinned individuals because the wavelength is poorly absorbed by melanin, which reduces the damage to dark epidermal pigmentation.3 The pulse length can be adjusted to deliver the pulse over a longer time period to facilitate cooling. Other laser choices for hair removal include the alexandrite and diode lasers at lower fluences and wider pulse widths. As with laser treatment of other skin disorders, multiple treatment sessions may be needed to achieve permanent results. Risks of laser hair removal in Fitzpatrick skin types IV through VI include blistering and temporary dyspigmentation with a low risk of permanent hyperpigmentation or hypopigmentation.3,4 Fig. 32.3 Laser hair removal. Lasers can be used for treatment of hypertrichosis in all skin types by targeting the melanin chromophore in the hair follicle. (a) A patient with Fitzpatrick skin type IV prior to laser hair removal of chin hair. (b) Postprocedure. Keloids and hypertrophic scars (▶ Fig. 32.4) occur more commonly in darker skinned individuals. Laser treatment of thickened scars may be considered in combination with intralesional steroid injections.5 The pulsed dye laser has been shown to decrease erythema, improve pain and pruritus, decrease lesion height, and improve hypertrophic scar pliability. These effects may facilitate intralesional steroid injection. However, the pulsed dye laser can target epidermal pigmentation and must be used with caution in patients with dark skin. Keloids may also be treated with the 1,064-nm Nd:YAG laser with moderate results of mild keloids. The lesion can be injected with intralesional triamcinolone 10 mg mL-1 up to 3 mL prior to starting therapy with regular laser treatments (fluence 13–18 J/cm2, 2,000 pulses) for 6 weeks.3 After 7 weeks, the lesion may be reevaluated and treatment repeated if necessary. Fig. 32.4 Keloids and hypertrophic scarring. Lasers can be combined with intralesional steroid injection for the treatment of keloids and hypertrophic scarring. (a) Detailing of keloid formation on the neck of a patient with Fitzpatrick skin type V. (b) The same patient is shown with improvement in keloid dyspigmentation and scar thickness following laser treatment. Before embarking on laser rejuvenation of facial skin, it is important to emphasize routine skin care to patients in order to optimize facial skin health prior to procedures. Sun should be avoided when possible and mechanical and chemical blockade (broad ultraviolet A and B sunscreens) should be used daily. Acne vulgaris can be treated with topical and oral antibiotics, hormonal treatments, and isotretinoin safely in all skin types and should be optimized before starting laser rejuvenation therapy.11 However, all isotretinoin should be avoided for a year prior to starting laser therapy due to increased risk of dyspigmentation. Furthermore, all herpes simplex virus (HSV) outbreaks should be treated with antivirals, and prophylaxis antivirals should be given to patients with HSV prior to starting laser treatments. Additional topical treatments with melanin suppressors, such as hydroquinone, kojic acid, azelaic acid, or emblica, may be considered for treatment of dyspigmentation and melasma before laser treatments, particularly in darker phototypes where nonablative laser therapies require several treatments with moderate results.5 In addition to using lasers with longer pulse duration and longer wavelength to decrease the risk of discoloration or scarring, periprocedural cooling should be considered to decrease thermal damage to surrounding tissues.4 Contact and noncontact cooling have the added benefit of improving patient comfort during laser therapy while decreasing thermal damage to the epidermis without interfering with laser intensity and direction. Options for contact cooling include skin moistening, application of ice or ice packs, and laser-specific cooling tips.7 When considering laser therapy on a patient with darker skin, a test spot adjacent to the intended area of treatment may be performed because individuals of the same ethnicity and phototype will react differently to the laser depending upon variable skin characteristics.12 Test spots should be started at low density, low fluence, and longer pulse duration settings. Full response and side effects should be observed at 1 month, at which point scarring and pigment changes will likely be evident. The major classes of lasers include ablative and nonablative lasers in both nonfractionated and fractionated varieties (▶ Table 32.2). Ablative lasers target water molecules in the epidermis, causing vaporization of skin cells and retraction of the dermis with collagen formation. Ablative lasers are more aggressive and function similarly to a skin peel with prolonged recovery time and a higher adverse-event profile.8 Nonablative lasers preserve the epidermis and target the dermal tissues to promote collagen formation. These nonablative treatments are milder and reduce the adverse-event profile and recovery time. Fractionated lasers are designed to target microscopic treatment zones (MTZs) to create columns of thermal injury with adjacent normal skin.5 This promotes healing and improves skin texture compared to nonfractionated lasers, without the high side-effect profile of ablative lasers. There are several options for laser therapy and it is important to consider the expectations of your patient while balancing the risks and benefits associated with laser therapy in patient-specific phototypes. Laser Outcomes Risks Ablative nonfractionated 10,600-nm CO2 2,940-nm Er:YAG Combined CO2 Er:YAG Dramatic improvement in wrinkle reduction, alleviate acne and atrophic scars8 Oozing, bleeding, and crusting [100%]8; acne, transient hyperpigmentation and hypopigmentation (IV) [55–68%]8,12; scarring and poor wound healing; permanent skin hypopigmentation5,8 Nonablative nonfractionated 1,319-nm Nd:YAG 1,320-nm Nd:YAG 1,450-nm diode Improvement in scar severity [29%]4; improvement in acne scars [10–50%]3,13; atrophic scarring and acne-induced PIH (III–VI) [51–75%]6; limited wrinkle improvement3 Minimal, few hours of erythema; no scaling or peeling; no abnormal pigmentation8 Nonablative fractionated 1,410 nm 1,440-nm Nd:YAG 1,540 nm 1,550-nm erbium 1,927-nm thulium fiber Moderate improvement in texture and wrinkles5; significant improvement in acne scarring [51–75%]4,6; overall appearance: excellent [30%], significant [59%], moderate [11%]4,13; safer in darker skin types due to limited tissue damage and melanocyte stimulation8 Moderate downtime; moderate pain6; PIH (III–V) [3, 12, 33%]6; acne [2%]12,14; herpetiform eruptions [2%]12,14 Ablative fractionated 10,600-nm fractional CO2 2,940-nm fractional Er:YAG 2,790-nm fractional Er:YSGG Moderate resurfacing power for mild skin laxity and rhytids3; moderate improvement in photodamage, scars [37%], and dyspigmentation3,8 Moderate downtime; moderate complications12; PIH (III-VI) [44%]4; use with caution in Fitzpatrick skin type VI3 Abbreviations: CO2, carbon dioxide; Er:YAG laser, erbium:yttrium aluminum garnet laser; Er:YSGG laser, erbium:yttrium scandium gallium garnet laser; Nd:YAG laser, neodymium:yttrium aluminum garnet laser; nm, nanometers; PIH, postinflammatory hyperpigmentation. Note: The four principal categories of lasers are presented here with examples of each laser and expected clinical outcomes and associated risks based on Fitzpatrick darker skin types (III–VI). ▶ Table 32.2 describes categories of lasers with specific examples of each type of laser. Ablative nonfractionated lasers include the 10,600-nm carbon dioxide (CO2) laser, the 2,940-nm erbium:yttrium aluminum garnet (Er:YAG) laser, and the combined CO2 Er:YAG laser. These lasers target the water molecules in the dermis and vaporize the epidermis. This class of laser has the most significant outcomes with significant improvement of fine wrinkles and acne scars.13 However, side effects of acne, permanent hypopigmentation, temporary hyperpigmentation, and skin infections are common. For these reasons, ablative nonfractionated lasers should be used with extreme caution in Fitzpatrick skin type IV patients and are contraindicated in phototypes V and VI due to the increased risk of scarring and dyspigmentation.5 Because of the high side-effect profile of the ablative nonfractionated lasers, a more gentle approach using nonablative technology was developed. The nonablative nonfractionated lasers include the 1,319-nm Nd:YAG laser, the 1,320-nm Nd:YAG laser, and the 1,450-nm diode laser. These lasers have demonstrated slight improvement with skin resurfacing and good results with acne treatment.2 There is minimal recovery time required, little erythema, and minimal peeling. The nonablative nonfractionated lasers often require serial treatment sessions (four–six treatments) to obtain improvement; however, they can be used safely in patients with darker skin due to decreased risk of scarring and dyspigmentation.8 In order to more effectively treat the skin, nonablative fractionated lasers were developed to combine a more aggressive pulse and the safety of fractionation while still avoiding the epidermal loss incurred with ablative lasers. These include the 1,410-nm laser, the 1,440-nm Nd:YAG laser, the 1,540-nm laser, the 1,550-nm erbium laser, and the 1,927-nm thulium fiber laser. These nonablative fractionated lasers frequently require several treatments (two–six) with moderate improvements in skin tone and texture with moderate downtime.8 The targeting of tiny diameter and deep dermal penetration of each MTZ allows for stimulation of collagen formation while avoiding disruption of the epidermal barrier function.13 These lasers can be used safely in darker phototypes with a small risk of temporary hyperpigmentation. The ablative fractionated lasers are the most recent addition to the laser family. These lasers were developed in an attempt to increase resurfacing effectiveness while still enjoying quicker healing with fewer complications compared to ablative nonfractionated resurfacing. These include the 10,600-nm fractional CO2 laser, the 2,940-nm fractional Er:YAG laser, and the 2,790-nm fractional erbium:yttrium scandium gallium garnet (Er:YSGG) laser. These lasers target MTZs with ablation and vaporization of dermal and epidermal tissues. A series of sessions may result in resurfacing results nearly comparable to the ablative nonfractionated lasers but with much-improved safety profiles.8 These lasers can improve skin laxity and mild rhytids; however, due to the violation of the epidermal layer, there is a risk of infection, scarring, and dyspigmentation and they should be used with caution in patients with Fitzpatrick skin types IV through VI.8 Ablative technologies offer the most significant reduction of rhytids and scarring but have the greatest risk of complications and should only be used in lighter phototypes.13 They can be utilized with extreme caution in Fitzpatrick skin type IV patients but should not be used in Fitzpatrick skin types V and VI because of risks of scarring and dyspigmentation.5 Nonablative fractionated and nonfractionated lasers may be used in all skin types with modest results for the reduction of fine wrinkles. These lasers may involve several treatments but require little recovery time with minimal erythema and sloughing.8 The importance of postprocedural planning and skin care cannot be overstated when managing patients following laser therapy. Because many of these procedures often entail several sessions, reducing skin damage between treatments can optimize epidermal healing and dermal collagen regeneration. The skin is more sensitive than usual for a short time after laser treatment and sun blockade and cooling agents should be used judiciously. Darker phototypes have more reactive and labile fibroblasts compared to Fitzpatrick skin types I through III and further dermal injury should be avoided.3 Most laser patients feel a sunburnlike sensation for the rest of the day following laser therapy. Topical skin care, oral analgesics, and cooling agents can all be used to improve patient comfort. Topical cooling agents, such as ice packs, are encouraged postprocedure to enhance patient comfort as well as decrease inflammation. Topical steroids may be considered in patients with persistent erythema. Depending on the type of laser used, mild erythema, edema, peeling, and flaking may occur and typically resolve over several days.14 The time period for full recovery depends on the type of laser process, and postoperative care must be tailored to the treatment administered. The postoperative skin care routine should include keeping the skin clean and moist to allow for re-epithelialization and to minimize the potential of scarring. In general, chilled, saline-soaked gauze can be applied intermittently for the first several days. The therapy area should be gently treated with a mild cleanser such as Cetaphil (Galderma Laboratories, Fort Worth, Texas) followed by the application of an oxygen-permeable ointment such as Aquaphor (Beiersdorf Inc., Wilton, Connecticut). Patients should be urged not to pull or pick at their skin as it starts to flake or peel because this may increase the likelihood of scarring. Depending upon the type of laser or resurfacing technique utilized, re-epithelialization typically occurs within a week. Avoidance of sun and the liberal use of sunscreen should be encouraged. Patients should avoid the use of retinoids and other bleaching agents at risk of causing irritation. Careful patient selection combined with conservative and judicious implementation of laser treatments can result in positive outcomes, when dealing with patients of color and darker skin types. In this particular subset of patients, the most common postprocedural concerns are related to dyspigmentation and scarring. Postinflammatory hyperpigmentation is a very bothersome side effect in darker Fitzpatrick phototypes (V and VI) (▶ Fig. 32.5).3,8 There are several choices for topical therapies when considering the treatment of hyperpigmentation, including hydroquinone, azelaic acid, kojic acid, and emblica. Hydroquinone, a common treatment option, is a plant-derived tyrosinase inhibitor and is often used to treat discrete hyperpigmented patches.5 Deleterious outcomes related to the use of hydroquinone may include hypopigmentation surrounding the treated area due to adjacent bleaching, in a “halo” effect.3,14 Fig. 32.5 Posttreatment postinflammatory hyperpigmentation. This complication is common with ablative lasers and may be reduced by using nonablative and fractionated techniques.
32.2 Treatment Goals
32.2.1 Skin Laxity
32.2.2 Dyschromia

32.2.3 Laser Hair Removal

32.2.4 Keloids and Hypertrophic Scarring

32.3 Medical Optimization
32.4 Classes of Lasers
32.5 Choosing a Laser
32.6 Postprocedural Care
32.7 Management of Possible Complications

Lasers for African Skin
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








