Monobloc and facial bipartition combined with distraction osteogenesis (MFBDO) has gained popularity over the past several years as a treatment of syndromic craniosynostosis, in part because this surgical technique effectively removes many stigmatic clinical features associated with the syndromic face. The objective of this study is to detail the surgical planning used to achieve medialization of the orbits and describe the authors’ experience using MFBDO to destigmatize the syndromic face. By using MFBDO, hypertelorism, vertical orbital dystopia, and downslanting of the palpebral fissure were surgically corrected in all patients, thereby destigmatizing the syndromic face.
Key points
- •
Monobloc Facial Bipartition Distraction Osteogenesis is a highly complex operation requiring a multidisciplinary team having both craniofacial and neurosurgical expertise.
- •
Syndromic patients operated on at 9 years of age or older present greater bony stability and therefore will most likely have lower relapse rates.
- •
The myriad of stigmatic facial features characteristic of Apert syndrome can be greatly improved with Monobloc Facial Bipartition Distraction Osteogenesis and internal devices.
Introduction
Monobloc facial bipartition (MFB) was predominantly used before the distraction osteogenesis (DO) era to simultaneously address midface retrusion accompanied by hypertelorism. MFB is a technique that combines 2 other landmark techniques based on specific principles originated by Tessier. Facial bipartition was added to frontofacial monobloc advancement in order to treat certain syndromic clinical features that could not be resolved by monobloc advancement alone.
Because DO was applied to the skull and other areas of the craniofacial skeleton, the increased bony stability and lower complication rates associated with monobloc DO compared with monobloc advancement became increasingly recognized. In the late 1990s, DO was added to MFB to create a novel technique named monobloc and facial bipartition advancement with distraction osteogenesis (MFBDO).
Patients whose syndromic craniosynostosis (SC), such as Apert, Crouzon, and Pfeiffer, with significant hypertelorism, are among those who benefit from medialization of hemi-halves of the face, in combination with midface advancement in a single bloc. Moreover, this technique is particularly effective for those syndromic patients simultaneously presenting a combination of midface retrusion and hypertelorism, vertical orbital dystopias, downslanting of the palpebral fissure, associated divergent strabismus, or a collapsed maxillary arch with an inverted “V” deformity. Among the syndromes referenced above, patients with Apert syndrome most commonly present features that are characteristic of the syndromic face, and frequently benefit from the palatal expansion generated by hemi-facial medialization. , Although MFBDO is a proven effective technique that corrects the aforementioned clinical features in SC patients, this technique is not currently used by most craniofacial centers worldwide.
The objective of this study is to describe the authors’ experience using MFBDO in patients with SC and provide in detail the surgical planning used to achieve medialization of the orbits and destigmatize the syndromic face.
Patients and methods
A retrospective study was performed on consecutive patients with SC who underwent MFBDO between 2007 and 2019 performed by the same craniofacial plastic surgeon and neurosurgeon (C.E.R.-A. and E.G.) working in tandem. Patients who solely underwent monobloc advancement and patients with incomplete medical records were excluded from this study.
Demographic data (patient gender and age when the procedure was performed), diagnosis, surgical-related data, and outcome data (mean midface advancement and mean interorbital distance before and after facial medialization) were verified via medical records, clinical photographs, and frontal and lateral cephalograms. Intraoperative complications related to orbital medialization, an inability to bring the midface forward during the distraction activation period (described as a collapse of the face), and improvement of strabismus, were all recorded.
Indications for MFBDO included SC patients with mild to severe exorbitism and/or midface retrusion, patients with recessive brow position, with or without clinical signs of elevated intracranial pressure, and patients who presented at least one of the following clinical features: hypertelorism, vertical orbital dystopias, marked downslanting of the palpebral fissure whether or not associated with divergent strabismus, or a collapsed maxillary arch with an inverted “V” deformity.
Distraction Protocol
After surgery, there is a 5- to 7-day latency period to facilitate sealing of the anterior cranial base. The latency period is followed by an activation period during which the midface is advanced at a rate of 1 mm per day. After the activation period is concluded, there is an 8-week consolidation period. In this study, the average total distraction advancement during the activation period ranged from 9 to 17 mm, depending on clinical need and patient age.
Distraction End Points
The endpoint for distraction was the orbital level, which left those patients operated on at skeletal immaturity with mild enophthalmos, to be corrected later. Conversely, patients who underwent surgery at skeletal maturity did not need subsequent overcorrection. The technical details of the surgery have been described in other articles by the authors. ,
All subjects enrolled in this study completed a consent form signed either by each adult patient or by the patient’s parents for patients younger than 18 years of age, in accordance with the Helsinki Declaration of 1975, as amended in 1983. Local institutional research ethics board approval was obtained for this study.
Surgical Technique
The 5 main specific surgical steps that are necessary in order to successfully perform an MFBDO were recently described in detail and demonstrated in 5 educational videos. The key component of the combined MFBDO technique is separation of the cranial segment, which is then followed by medialization of the face. These 2 important steps consisting of facial bipartition and facial medialization are further discussed later and are specifically referred to as facial bipartition and medialization of the facial segments.
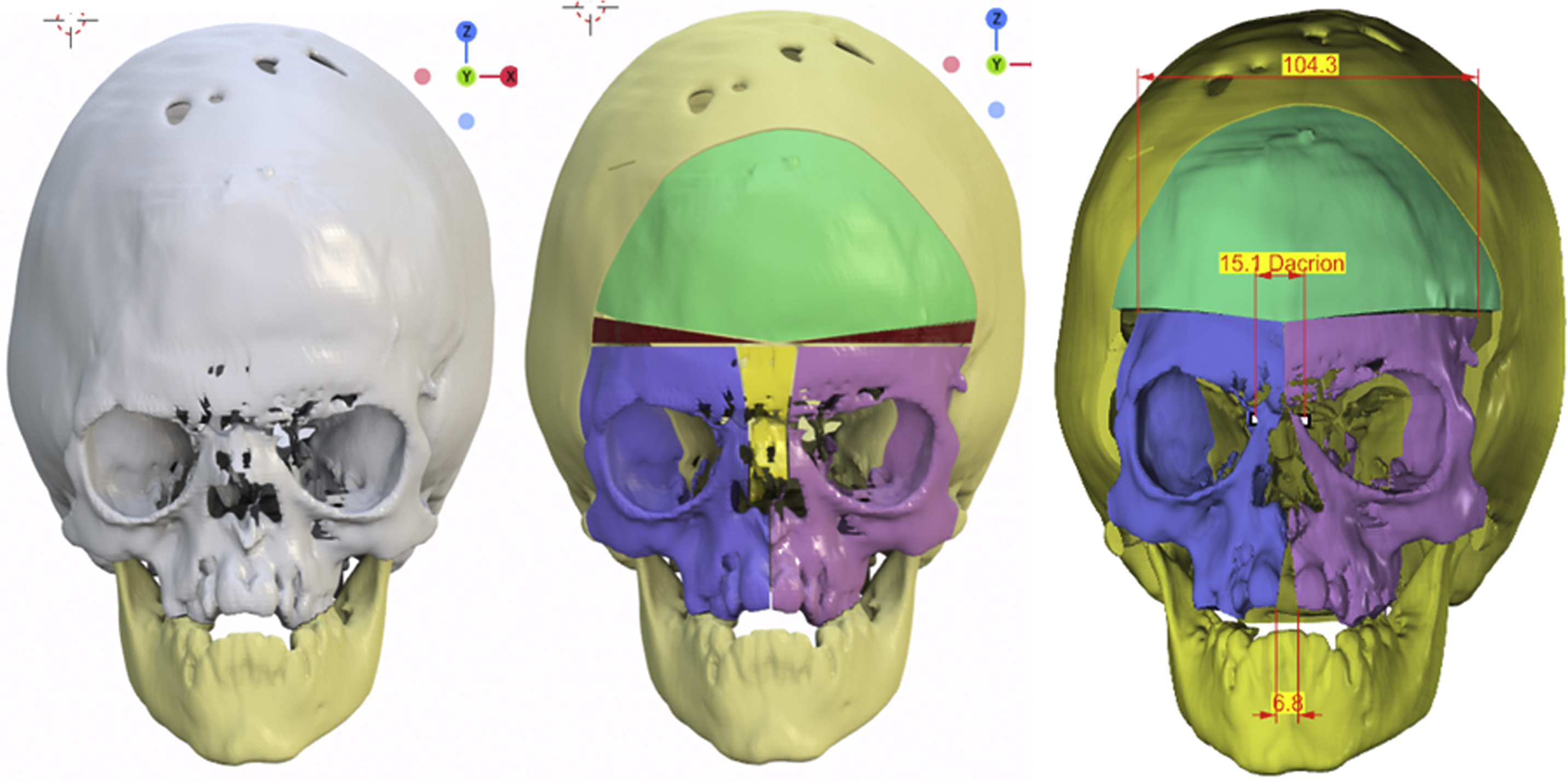
Facial bipartition
Before bipartition, the interdacryon distance is measured with a caliper, and a V-shaped osteotomy is marked and performed via reciprocating saw from the upper medial orbital border toward the nasal bone. An approximate average of between 5.5 and 9.5 mm of bone is maintained as a margin between each medial orbital wall, leaving between 11 and 19 mm of bone separating the medial canthi. The larger the degree of hypertelorism, the wider the angle of the midline “V” needs to be, in order to adequately medialize the hemi-facial halves. Thus, it is essential to accurately determine the amount of residual bone that will be left in place, rather than the amount of bone that needs to be resected. If the patient also presents vertical orbital dystopia, this factor should be taken into account during the medialization maneuver in order to compensate for the vertical discrepancy between the orbits.
The hard palate is osteotomized at the midline, followed by an alveolar osteotomy between the frontal incisors, using a smaller osteotome. These midline palatal and alveolar osteotomies usually result in a frontal incisor diastema or in some cases a height discrepancy between the frontal teeth.
The pericranial flap is inserted into the midline region at the anterior cranial base in order to keep the oral and nasal cavities separate from the brain, and the flap is then sutured to the dura mater. Alternatively, a periosteum patch can be sutured to the dura mater at the anterior cranial base.
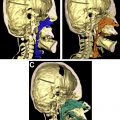
Medialization of Facial Segments
The facial segments are moved medially and vertically as needed to achieve facial convexity. There is also a small degree of rotation along the vertical axis (yaw) that also restored facial convexity. All bone in the midline, beginning at the frontal bone of the supraorbital rim, across the ethmoid bone, up to and including the nasal bone, needs to be removed in order to enable facial segment medialization. Facial segment stability is ensured by fixation with 2.0-mm titanium plates and screws at the midline region, and by wires at the maxillary region. Nasal bone grafts as needed can also be placed in the midline region. Interdacryon distance is remeasured. Medial canthopexy with wires is performed to enable the redundant midline tissue to shrink and provide better definition to the midline region. The authors’ preference is to use Kawamoto midface internal distraction devices (KLS Martin, Jacksonville, FL, USA), which are placed anteriorly in the inferior region of the lateral orbital wall, posteriorly behind the zygomatic root, and above the auditory canal, as these areas of the craniofacial skeleton and cranial base are particularly thick. An external halo device can also be considered.
After placement of 2 drains below the scalp between the periosteum and galea tissue, the distractors are partially activated and then reversed to test for bony stability, and incisions are sutured. The frontal bone flap is carefully trimmed in order to closely correspond with the new orbital bar position, which usually has a V shape. The inferior border of the frontal bone must be trimmed into an inverted V shape to securely attach to the superior orbital bar ( Fig. 1 ).
Results
Among the 18 patients who underwent monobloc advancement during the study period, 9 patients underwent MFBDO. The average patient age at MFBDO surgery was 11.6 ± 6.6 years. The average length of hospital stay was 5 days. Mean distraction advancement was 14.3 ± 2.68 mm. The mean preoperative interorbital distance measured intraoperatively was 32.2 ± 1.85 mm, and the mean postoperative interorbital distance was 14.4 ± 2.45 mm.
Hypertelorism, vertical orbital dystopia, and downslanting of the palpebral fissure were corrected in all patients. Divergent strabismus, which was presented by 5 of the 9 patients who underwent MFBDO, was corrected without the need for separate ophthalmologic surgery.
During the medialization maneuver, an unexpected fracture line of the orbital bar occurred with 1 Apert patient, which extended to the medial, superior, and lateral orbits. The upper facial segment, where the fracture line occurred, was affixed laterally with a 2.0-titanium plate and medially to the contralateral side and maintained stability throughout activation process; there was no collapse or disruption of the bony segments. This particular patient did not present divergent strabismus preoperatively but developed convergent strabismus postoperatively ( Figs. 2–5 , Table 1 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree