Total Skin-Sparing Mastectomy
V. Suzanne Klimberg
Introduction
Preservation of the native skin envelope facilitates immediate breast reconstruction (IBR) and has begun a new era in breast reconstruction. The skin-sparing mastectomy (SSM) removes the breast, nipple–areola complex (NAC), previous biopsy incisions, and skin overlying superficial tumors. Toth and Lappert (1) in 1991 were the first to describe the SSM followed by IBR. The most apparent advantage of SSM followed by IBR is the superior aesthetic and cost-effective result compared with either simple mastectomy with IBR or delayed reconstruction (2,3). In addition, this surgical technique is also psychologically beneficial to the patient (4,5).
Gerber and colleagues (6) described the SSM with conservation of the NAC (a subcutaneous mastectomy) to leave a woman with a natural-appearing breast. Petit and colleagues (7) have described technique what is basically a subcutaneous mastectomy followed by intraoperative radiation to the preserved NAC with a very low recurrence rate (1.4%) none of which were in the NAC. The NAC necrosed totally in 3.5% and partially in 5.5% or was removed in 5% of 1,001 reported cases. Twenty-month follow-up demonstrates 96% disease-free survival rate.
The term total skin-sparing mastectomy (TSSM) was described by Margulies et al. to denote that the NAC proper was removed but the skin overlying the NAC was spared (8). Other authors describe the procedure as nipple-sparing mastectomy (9). This is a confusing term in that only the skin overlying the nipple proper has been retained. This is considered safe as the cuboidal-lined ducts begin only at approximately 7 mm from the surface of the nipple (10).
There is no long-term follow-up after TSSM. A few small series with short follow-up show the expected safety of TSSM with approximately a 5% partial or full-thickness loss of the NAC skin but a much higher rate (17%–20%) of NAC involvement and elective removal dependent on selection criteria (11).
Sakamoto and colleagues (12) described an endoscopic technique for TSSM. A 52-month follow-up showed no local recurrences in a series of 87 patients. The rate of nipple necrosis among the procedures with nipple coring was statistically higher than that among those without nipple coring (7 of 17, 41% vs. 9 of 72, 13%).
The indications for a TSSM include the following:
Can include any indication that a simple mastectomy can be performed for (see Simple Mastectomy chapter) as long as the pathological entity does not involve the NAC. This most commonly would involve ductal carcinoma in situ that by review of the pathology and imaging studies does not appear to involve the NAC. In-house review of pathology is important to rule out an invasive component or a significant risk of such a component (high-grade, >2 cm, multicentric) as to warrant a sentinel lymph node. A cytologic diagnosis is not considered sufficient to proceed with mastectomy.
Prophylactic contralateral simple mastectomy (SM) is indicated for those patients with a high risk of bilaterality (lobular pathology, locally advanced or inflammatory invasive breast cancer, and especially multicentricity).
Prophylactic bilateral mastectomy can be performed in those with atypia and lobular carcinoma in situ who cannot reliably be screened (difficult mammogram or examination) or in those with a known genetic predisposition to breast cancer.
Completion mastectomy after a conservative surgery with positive margins
Completion mastectomy after a local recurrence although prior radiation if administered can cause sufficient skin damage to significantly increase the complication rate and impair the cosmetic result.
Contraindications/Relative Contraindications
Many patient-related risk factors such as smoking, previous irradiation, diabetes, increased body mass index, and large ptotic breast have been found to associate with an increased risk of skin necrosis in SSM.
Preoperative planning of TSSM should include consideration of preexisting incisions, need or risk of resection of the NAC, and removal of the entire breast parenchyma.
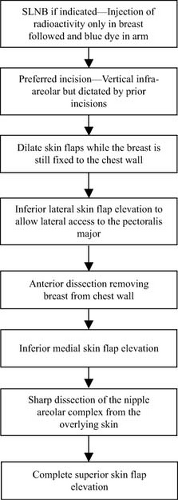
Order of Procedures
The radiopharmaceutical is injected into the breast first and blue dye is injected into the arm for axillary reverse mapping (ARM) (see Axillary Reverse Mapping chapter). Blue dye should be avoided in the skin or around the areola in TSSM as it may cause a higher incidence of skin loss when doing so. The sentinel lymph node biopsy is then performed (see Sentinel Lymph Node Biopsy chapter) first but if one wants to avoid, a separate incision can be done through the same incision as the TSSM but with much greater difficulty and delay in the results of the SLN intraoperatively and whether or not the patient requires an ALND (Fig. 25.1).
Relevant Anatomy
Figure 25.2A demonstrates the limits of a simple mastectomy that run from the second to third rib superiorly down to the insertion of the rectus and medially to the sternum and lateral to the mid axillary line. Figure 2B demonstrates the blood supply to the skin of the breast. Superiorly the skin is feed by the superficial cervical artery, laterally by the lateral thoracic vessels, medially by the perforators from the internal mammary vessels, and inferiorly from branches of the superficial epigastric and vessels extending from the medial and lateral blood supply.
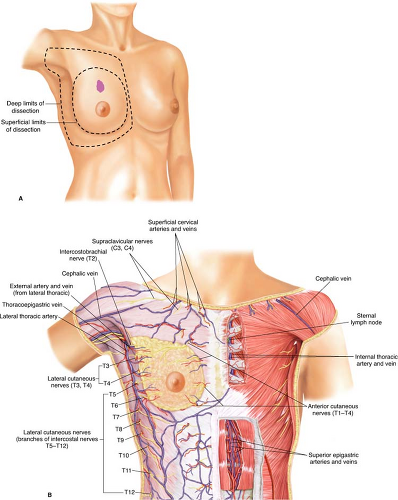 Figure 25.2 A. Borders of breast and limits of dissection for total skin-sparing mastectomy. B. Blood supply of the skin of the breast. |
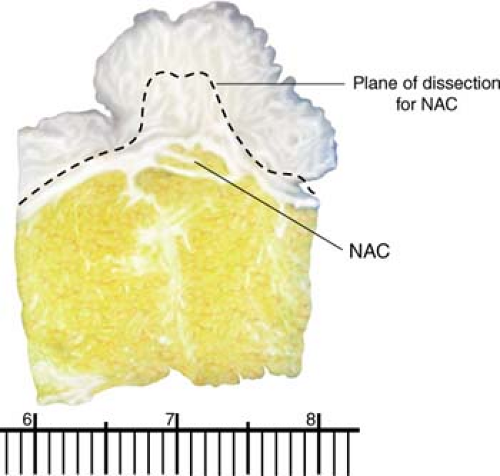
Figure 25.3 demonstrates the relevant anatomy of the overlying breast. The cosmetic result of any lumpectomy depends on the depth of the subcutaneous tissue underneath the incision. Thus, if only thin flaps remain after the resection of a superficial tumor and breast, it is best to resect an overlying ellipse of skin. A simple mastectomy also removes the fascia overlying the muscle because the fascia of the breast melds with the fascia of the pectoralis major. Removal of the pectoralis major fascia facilitates as much removal of breast tissue as possible. Complete removal is impossible as some breast tissue intercollates into the muscle itself. If the tumor is deep, muscle may be removed.
The ducts of the breast proper begin approximately 7 mm from the skin surface, thus making it safe to leave the thin skin overlying the nipple proper (10). Rusby et al. have tried to develop a model to predict the risk of nipple areolar involvement and thus recurrence. The percentage of NAC involvement appears to be dependent on the distance from the NAC but also proportional to the depth at which one defines the NAC (13,14) (Fig. 25.4).
Surgical Technique
Anesthesia
Although a simple mastectomy can be performed under local anesthesia, it is rarely if ever necessary and should be performed under general anesthesia. Some have advocated spinal or vertebral block for anesthesia. Significant time preoperatively should be allocated to this endeavor not only by the patient but for coordination of the team effort. The preoperative pain experienced by the patient for the necessary block is the trade-off for avoidance of general anesthesia.
Positioning
The patient is placed supine with the arm extended at right angle with the body positioned as with lumpectomy juxtaposed to the edge of the table for a unilateral mastectomy such that the surgeon and assistant can stand on opposing sides of the arm and assist in surgery. Both breasts should be prepped in the field as a TSSM is almost always done with follow-up reconstruction. The patient should be positioned in the middle of the table for bilateral mastectomies. The arm board should be padded, so the arm is at the level of the body. Too much or too little padding can lead to nerve praxis. For a simple mastectomy, there is no need to drape the lower arm into the field (Fig. 25.5).
Incision
There is no long-term follow-up on local recurrence after TSSM or comparison or clear consensus in the literature on what is the best incision for TSSM. Several incisions have been described, such as the mastopexy incision, incisions crossing the NAC, radial and the inframammary, (15




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree